Lots of interesting abstracts and cases were submitted for TCTAP 2022. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-171
Successful Transcatheter Thrombectomy in High Risk Massive Pulmonary Embolism Patient With Recent Major Cerebral Hemorrhage
By Thinnakrit Sasiprapha, Sarunyoo Suttipongkeat, Nahathai Chatrasingha
Presenter
Thinnakrit Sasiprapha
Authors
Thinnakrit Sasiprapha1, Sarunyoo Suttipongkeat2, Nahathai Chatrasingha3
Affiliation
Ramathibodi Hospital, Thailand1, Bhumibol Adulyadej Hospital Royal Thai Air Force, Thailand2, Navavej, Thailand3,
View Study Report
TCTAP C-171
STRUCTURAL HEART DISEASE - Pulmonary Intervention: CTEPH, PHTN
Successful Transcatheter Thrombectomy in High Risk Massive Pulmonary Embolism Patient With Recent Major Cerebral Hemorrhage
Thinnakrit Sasiprapha1, Sarunyoo Suttipongkeat2, Nahathai Chatrasingha3
Ramathibodi Hospital, Thailand1, Bhumibol Adulyadej Hospital Royal Thai Air Force, Thailand2, Navavej, Thailand3,
Clinical Information
Patient initials or Identifier Number
SS
Relevant Clinical History and Physical Exam
A 37 years old man with the underlying disease of uncontrolled DM and HT presented with sudden alteration of consciousness and right hemiparesis. CT brain demonstrates left basal ganglia hemorrhage. After a week of admission, he developed sudden dyspnea and chest discomfort. His blood pressure was 91/60 mmHg, his heart rate was 160 bpm, he was intubated and his oxygen saturation was 80 % (FiO2 1.0). The lung auscultation was clear and no murmur was audible, mild pitting edema right leg is noted.


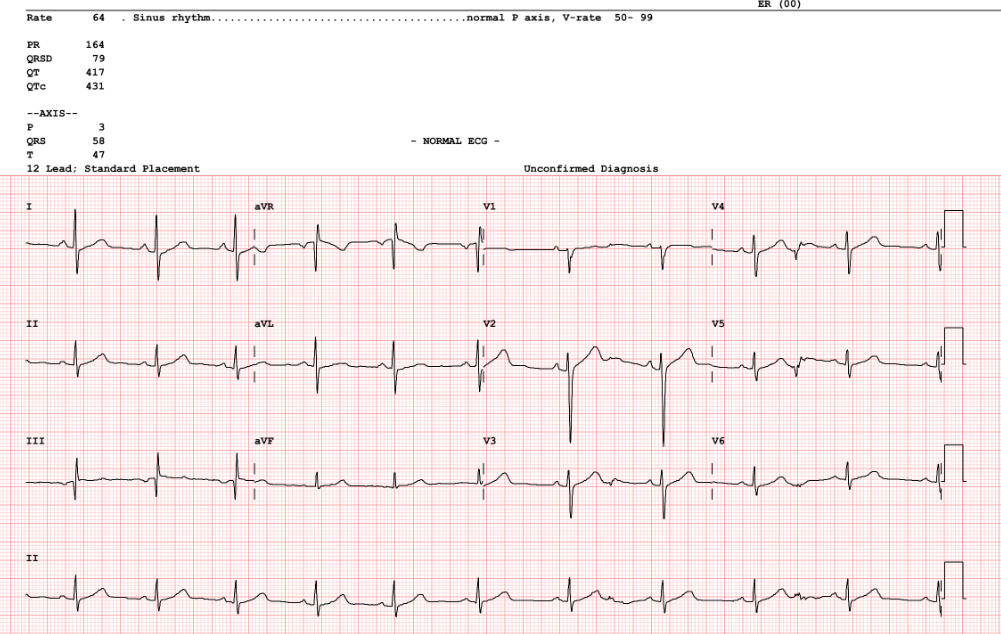


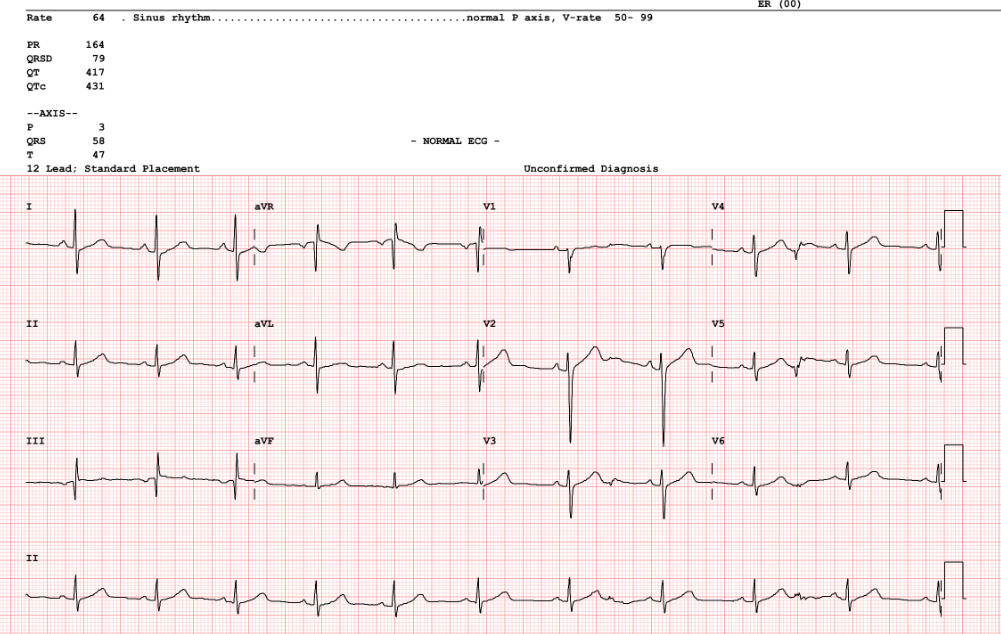
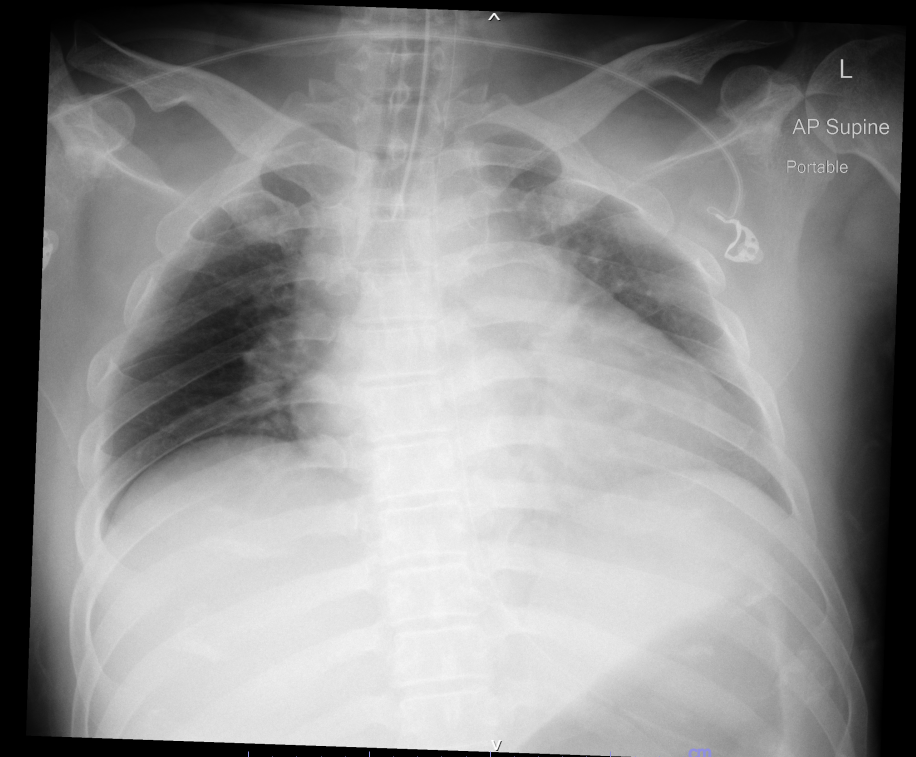
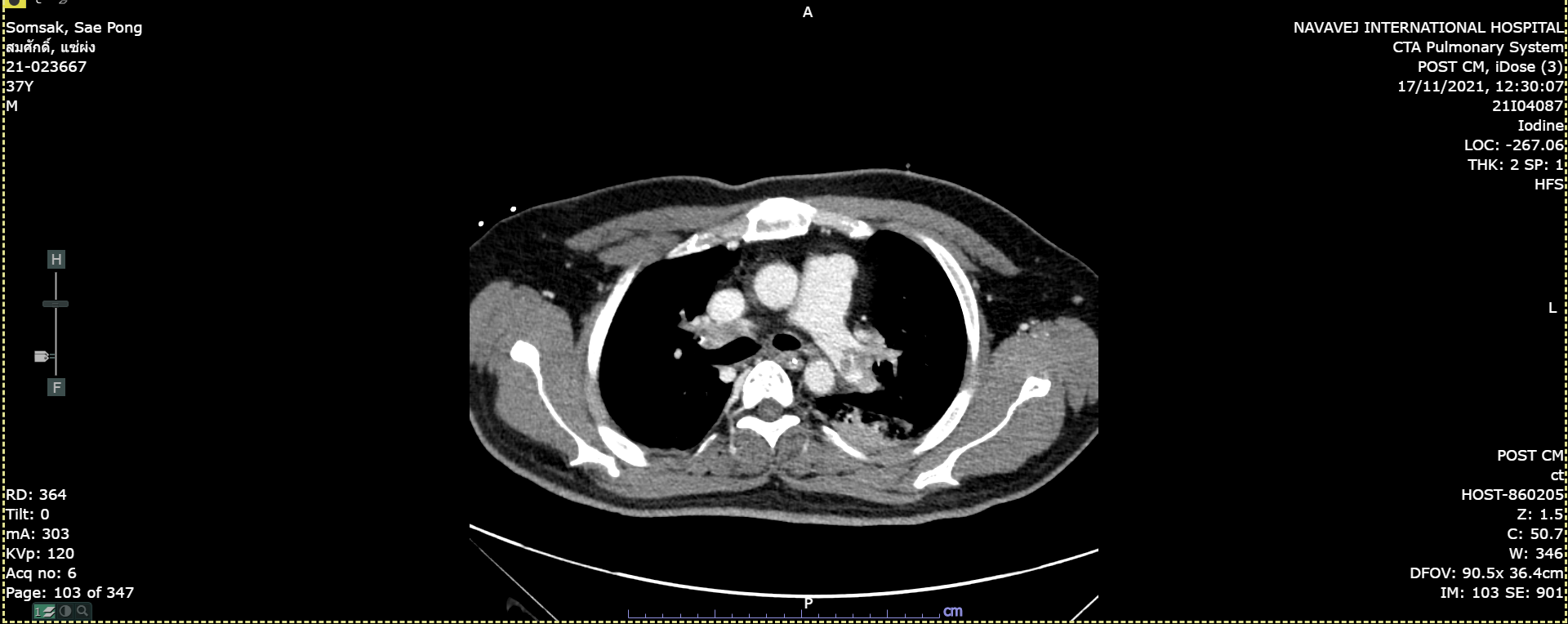
Relevant Test Results Prior to Catheterization
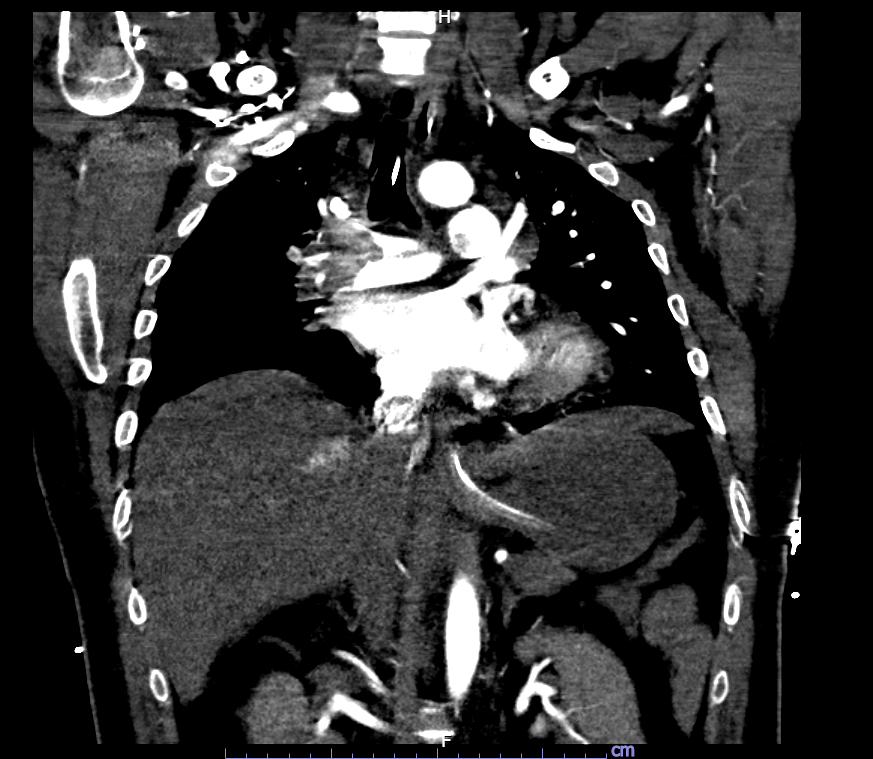
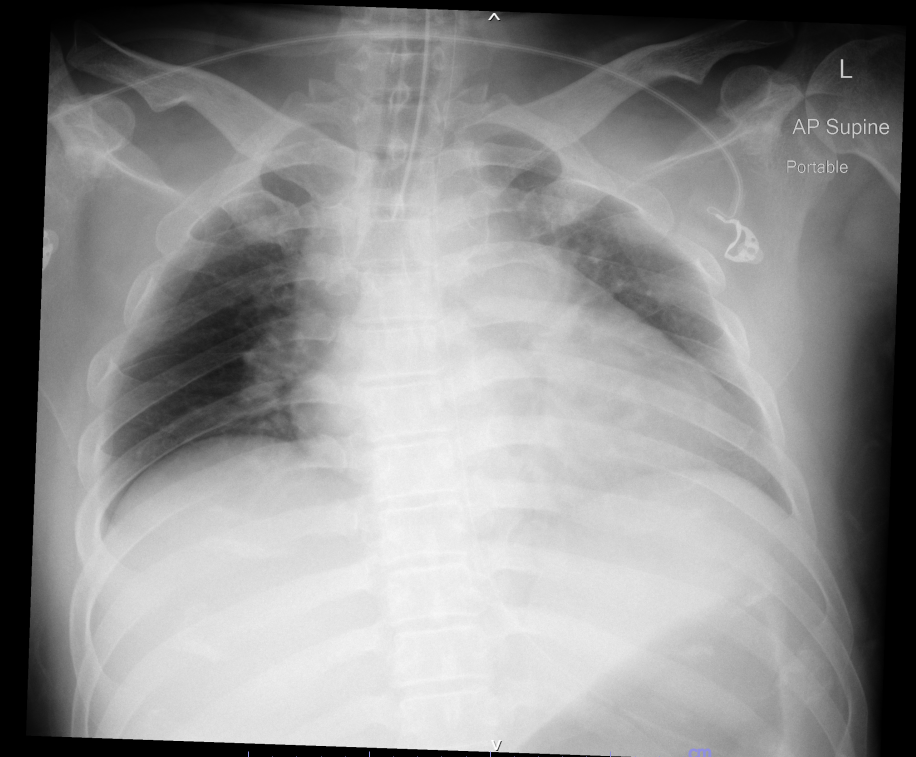
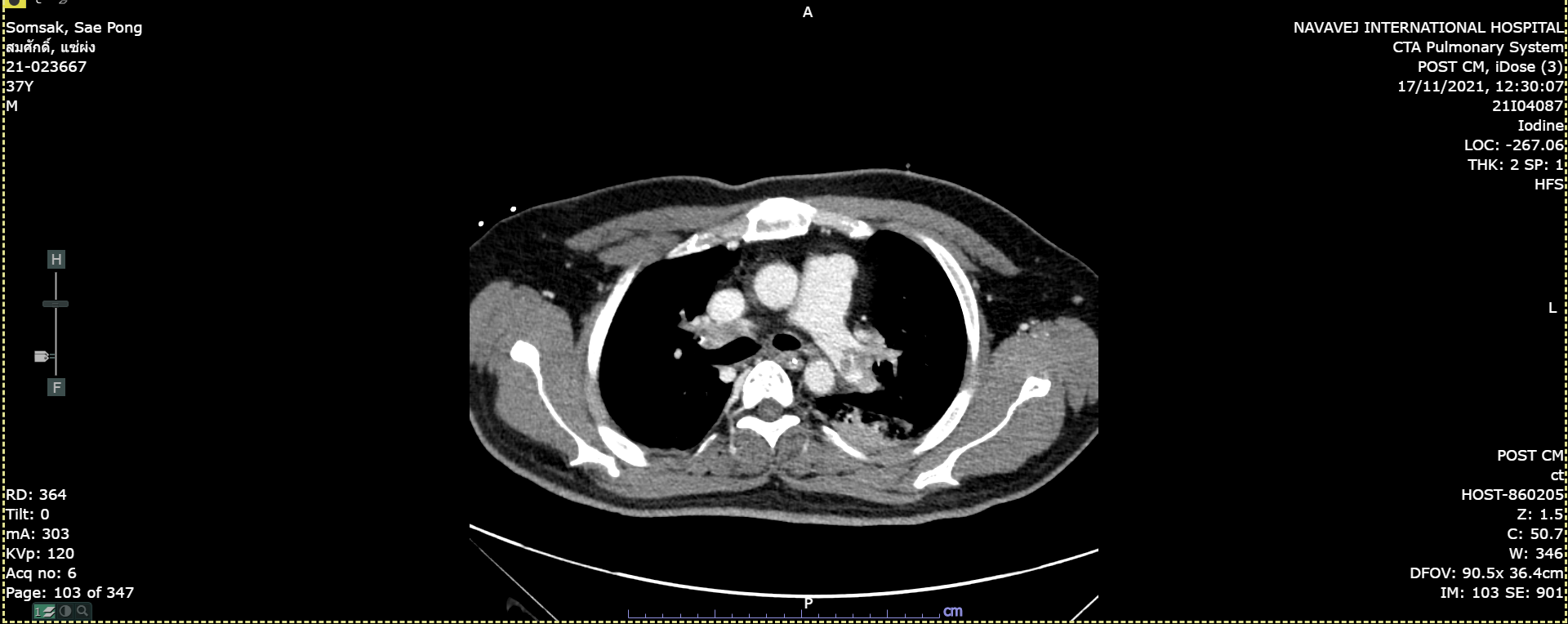
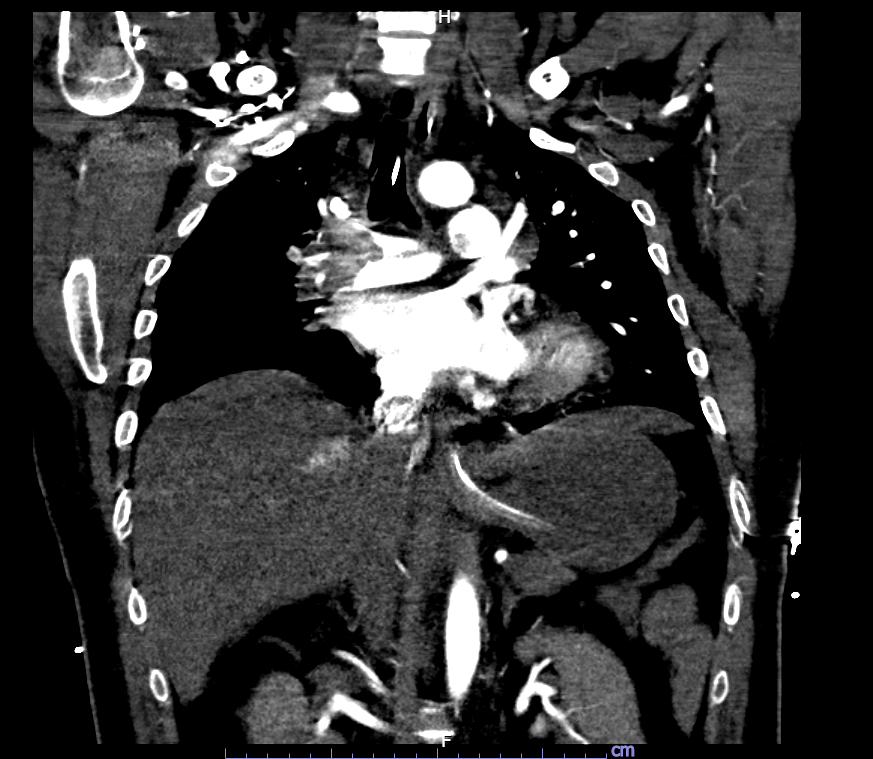
A chest X-ray showed no new pulmonary infiltration but diffuse lung oligemia and cardiomegaly were detected. The CTA revealed a huge concentric intraluminal filling defect involving RPA and LPA confluence (saddle embolism) extending to RPA, LPA, bilateral ascending and descending interlobar arteries, all lobar pulmonary arteries as well as segmental/subsegmental branches pulmonary arteries. An echocardiogram showed severely dilated RV with RV systolic dysfunction.
Relevant Catheterization Findings
A selective LPA angiogram showed total occlusion of the left upper lobe branch and subsegmental branches of the lower lobe. The selective RPA revealed a large filling defect at the right main pulmonary artery with subtotal occlusion at the right upper lobe segmental branches and right descending interlobar artery with slow pulmonary blood flow.
 RPA dx.mp4
RPA dx.mp4
 Left Dx4.mp4
Left Dx4.mp4
Interventional Management
Procedural Step
The patient's condition rapidly deteriorated then he was transferred to the cath lab immediately. A 10F sheath was rapidly placed into the right femoral vein, 6F JR3.5 catheter was passed along with 0.035" Glidewire(Terumo) to the left pulmonary artery. The initial PA pressure was 55/29(40). Then we switched to 0.035" J wire and placed it in the distal left PA as far as possible. We removed the JR catheter and a 10F sheath and inserted the Indigo aspiration catheter(CAT8) to the left PA just proximal to the thrombotic lesion. We selectively did an angiogram to the left PA to identify the target branch, we connected the CAT8 catheter to the Penumbra engine and an Indigo separator was inserted. We rotated the catheter to place it in the target branches, then we opened the vacuum system. If the catheter is in the thrombus or target area, the flow will be slow or no flow then the separator is advanced and retracted to facilitate clearing of the thrombus. The vacuum was turned off if there was free flow during a suction, meaning that the catheter was not in the target area. After that, We moved the catheter to the right PA and did the same steps. Finally, we could remove a large amount of clot from the upper branch and interlobar artery, the final flow was improved. The patient intermittently developed asystole required CPR during the procedure and he needed high dose inotropic drugs to maintain his hemodynamic. We decided to stop the procedure and placed the IVC filter.
 RPA treat1.mp4
RPA treat1.mp4
 RPA upper lobe final.mp4
RPA upper lobe final.mp4


Case Summary
At CCU, the patient's hemodynamic was stable and we could discontinue inotropic drugs in 2 days and extubate the endotracheal tube on day 3. The patient consciousness was recovered back to the same level as before this event. There was acute kidney and liver injury from obstructive shock on the first day but gradually improved and fully recovered in a week. We presented the case with acute massive pulmonary embolism who had an absolute contraindication for fibrinolysis and anticoagulant and was successfully treated by transcatheter thrombectomy with a good result.


