Lots of interesting abstracts and cases were submitted for TCTAP 2022. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-158
Hemodynamic Assessments to Guide Revascularisation Strategy in Cardiomyopathy of Unclear Aetiology: Are We Too Quick to Blame Ischemia?
By Wee Meng Ng, Cliff Li, Fahim Jafary
Presenter
Wee Meng Ng
Authors
Wee Meng Ng1, Cliff Li1, Fahim Jafary1
Affiliation
Tan Tock Seng Hospital, Singapore1,
View Study Report
TCTAP C-158
IMAGING AND PHYSIOLOGIC LESION ASSESSMENT - Physiologic Lesion Assessment
Hemodynamic Assessments to Guide Revascularisation Strategy in Cardiomyopathy of Unclear Aetiology: Are We Too Quick to Blame Ischemia?
Wee Meng Ng1, Cliff Li1, Fahim Jafary1
Tan Tock Seng Hospital, Singapore1,
Clinical Information
Patient initials or Identifier Number
S C W
Relevant Clinical History and Physical Exam
Our patient is a 45-year-old Chinese male who presented with exertional dyspnea for 6 months. He had history of hypertension, diabetes and previous PCI to left circumflex artery in 2015 but defaulted follow up. Of note, history taking revealed alcohol intake of 41 standard units per week.
Clinical examination was unremarkable – examination of the precordium did not reveal any murmurs, there were also no findings suggestive of heart failure clinically.
Clinical examination was unremarkable – examination of the precordium did not reveal any murmurs, there were also no findings suggestive of heart failure clinically.
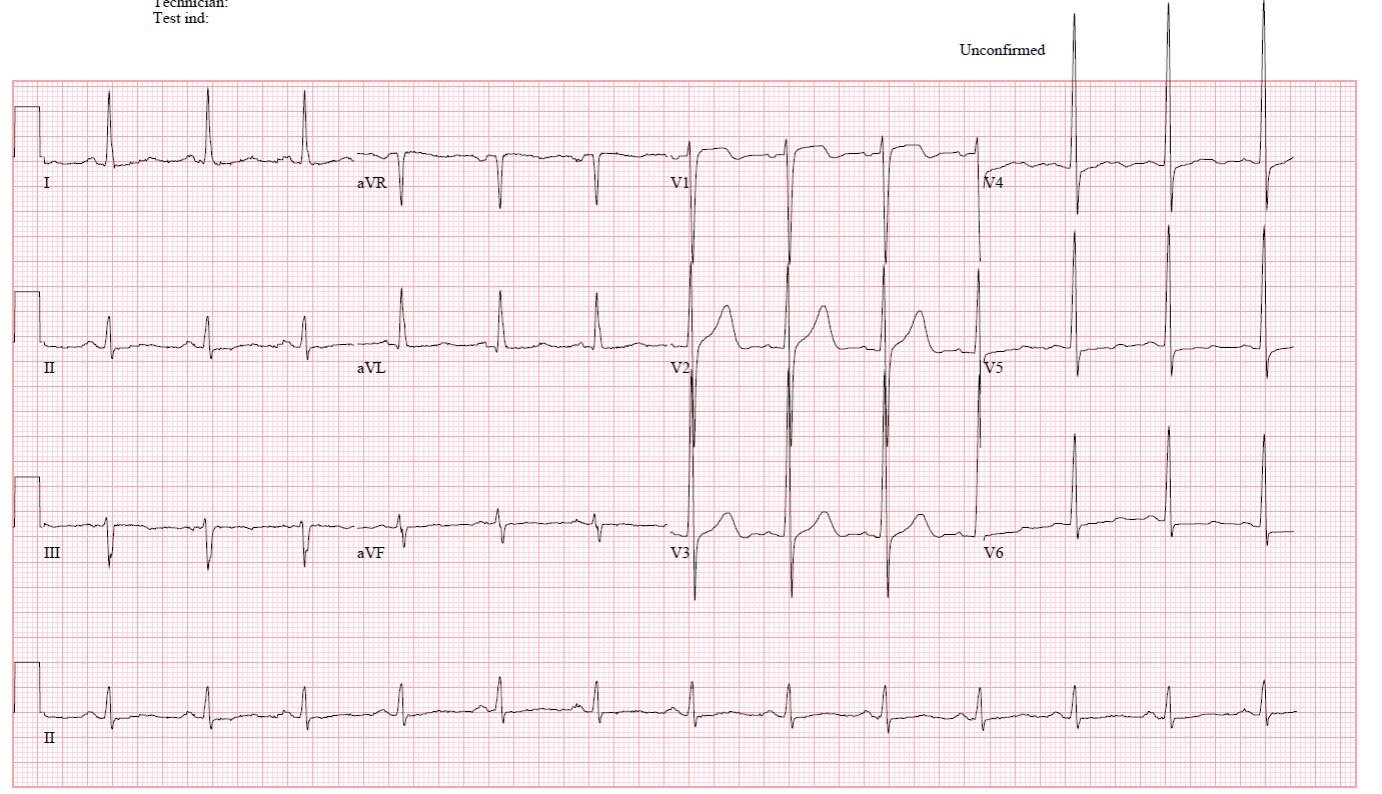
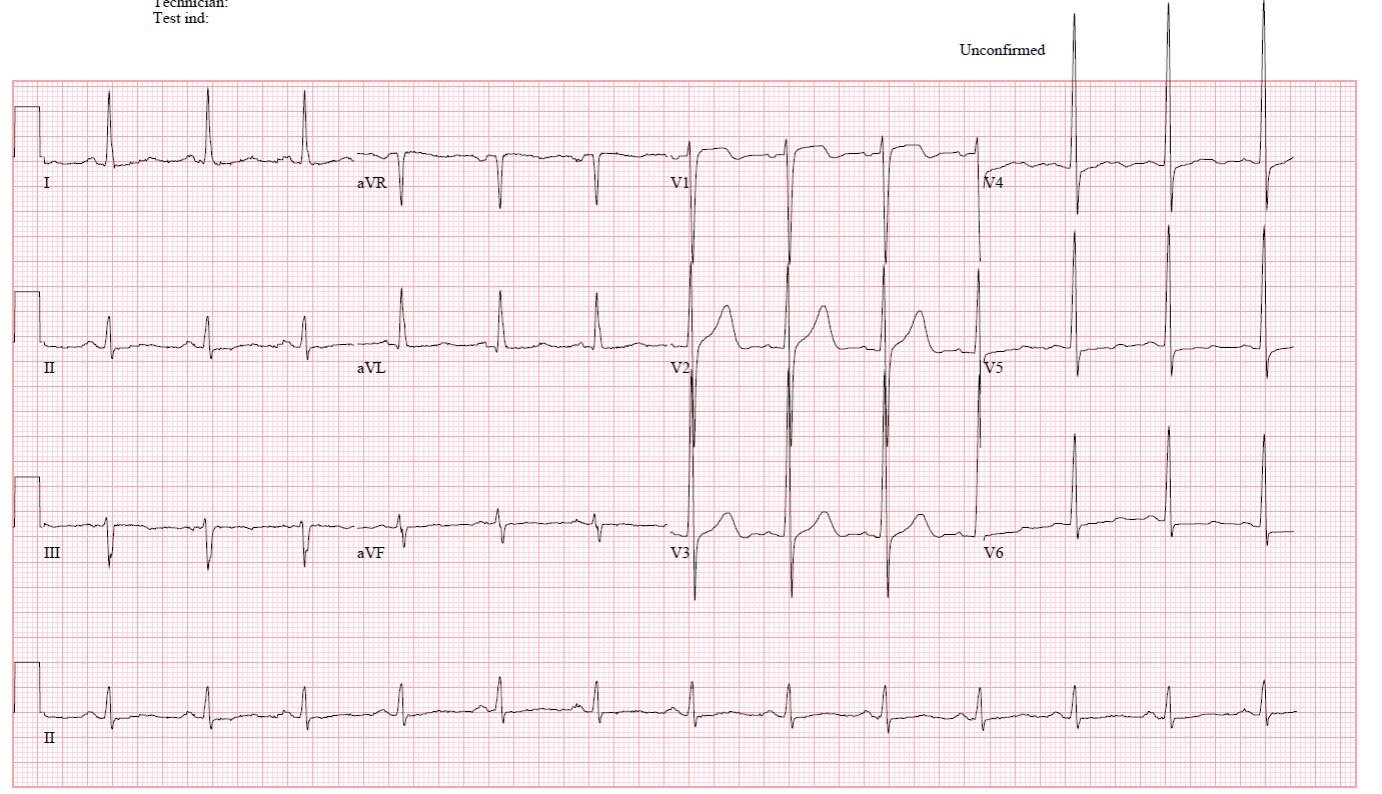
Relevant Test Results Prior to Catheterization
An echocardiogram showed LVEF of 35% with global hypokinesis and eccentric left ventricular hypertrophy, and no significant valvular disease.
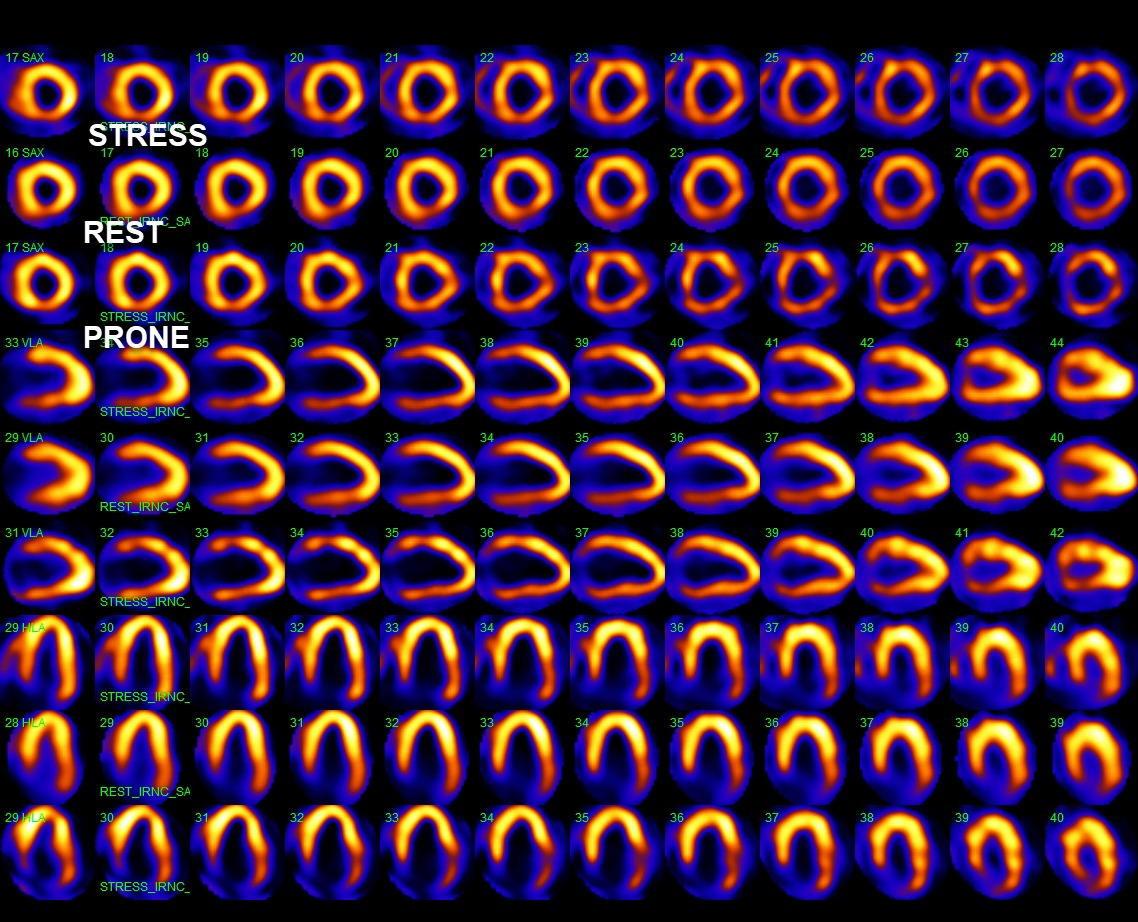
Myocardial perfusion scan showed fixed medium sized perfusion defects in the inferior and lateral segments, consistent with partial thickness infarcts with no superimposed ischemia and moderate retained viability. Significantly, there was a small sized basal to mid anterior perfusion defect which was predominantly reversible, consistent with ischemia.
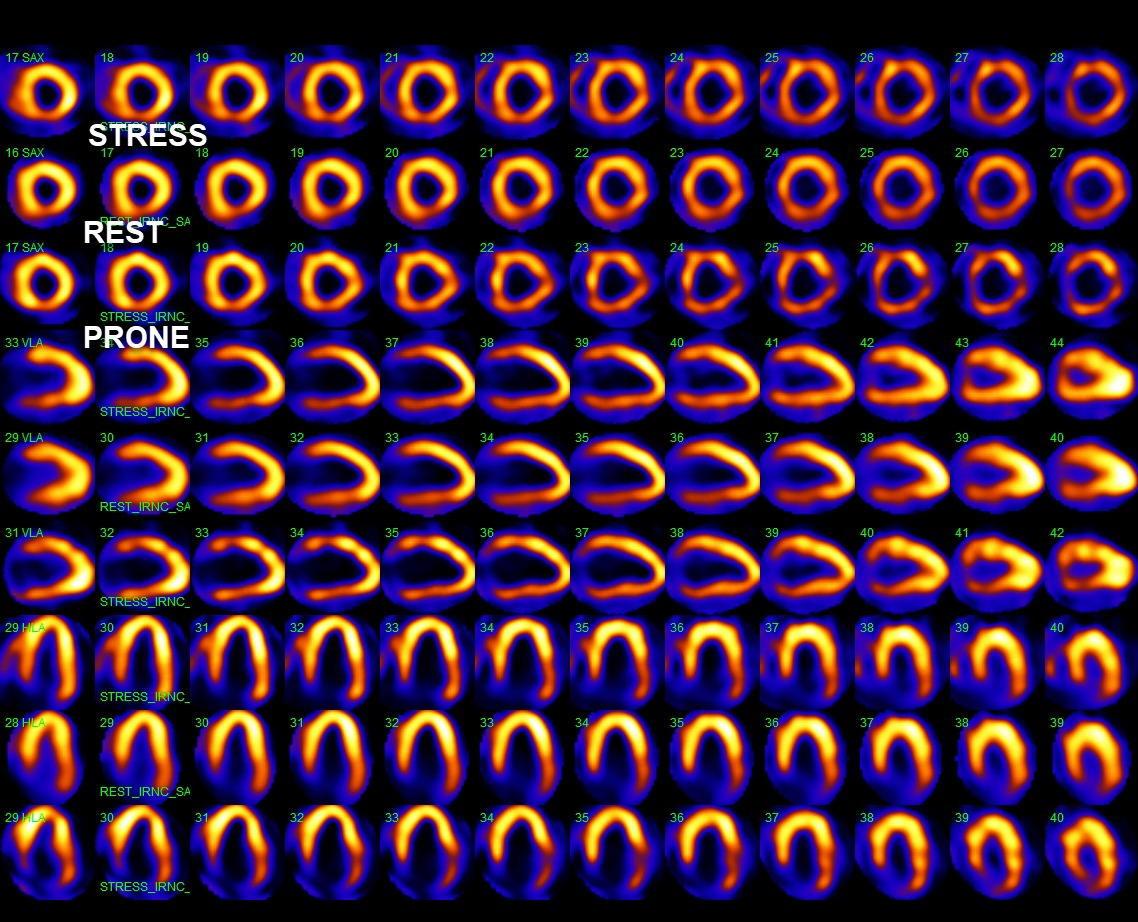
Myocardial perfusion scan showed fixed medium sized perfusion defects in the inferior and lateral segments, consistent with partial thickness infarcts with no superimposed ischemia and moderate retained viability. Significantly, there was a small sized basal to mid anterior perfusion defect which was predominantly reversible, consistent with ischemia.
Relevant Catheterization Findings
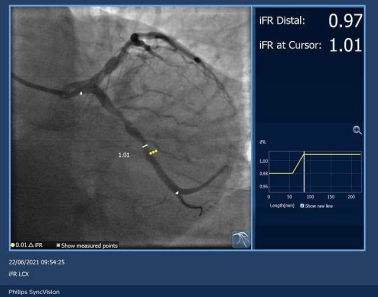
The coronary angiogram demonstrated angiographically moderate to severe stenosis in left circumflex (LCx) and right coronary artery (RCA) disease with moderate left anterior descending (LAD) disease.
Left main – free of disease
 iFR NICMP - RCA 1 (1).mp4
iFR NICMP - RCA 1 (1).mp4
 iFR NICMP - Cx 2 (1).mp4
iFR NICMP - Cx 2 (1).mp4
 iFR NICMP - LAD 2 (1).mp4
iFR NICMP - LAD 2 (1).mp4
Left main – free of disease
Interventional Management
Procedural Step
We regarded the myocardial perfusion scan findings as somewhat non-diagnostic for the following reasons – (1) the degree of left ventricular dilatation and dysfunction seemed somewhat out of proportion to the extent of the coronary artery disease (2) the “basal anterior ischemia” reported was perhaps artifactual given the fact that isolated basal ischemia is distinctly unusual without concomitant apical ischemia and (3) this patient had other features in his history, including a history of alcoholism as well as non-compliance to medications that compelled additional evidence before revascularization (surgical or PCI) was undertaken.
As such, decision was made to proceed with hemodynamic assessment of all 3 vessels. iFR was chosen instead of FFR in view of significant transient bradycardia at the start of the procedure, limiting use of adenosine. Surprisingly, iFR readings of 0.92 (LAD), 0.96 (LCx) and 0.99 (RCA) indicated hemodynamically insignificant lesions.
In view of the discordant results between the stress myocardial perfusion scan and invasive hemodynamic assessment findings, a joint decision was made with the patient for a trial of optimal medical therapy and alcohol abstinence.
Cardiac magnetic resonance imaging performed 4 months after demonstrated recovery of left ventricular dysfunction, with no dyskinetic/akinetic segments, late gadolinium enhancement and an ejection fraction of 60%.


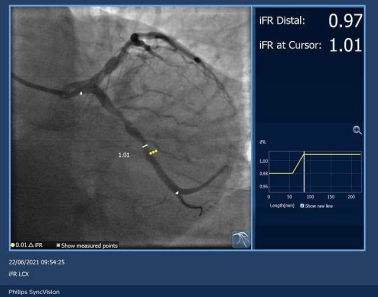
As such, decision was made to proceed with hemodynamic assessment of all 3 vessels. iFR was chosen instead of FFR in view of significant transient bradycardia at the start of the procedure, limiting use of adenosine. Surprisingly, iFR readings of 0.92 (LAD), 0.96 (LCx) and 0.99 (RCA) indicated hemodynamically insignificant lesions.
In view of the discordant results between the stress myocardial perfusion scan and invasive hemodynamic assessment findings, a joint decision was made with the patient for a trial of optimal medical therapy and alcohol abstinence.
Cardiac magnetic resonance imaging performed 4 months after demonstrated recovery of left ventricular dysfunction, with no dyskinetic/akinetic segments, late gadolinium enhancement and an ejection fraction of 60%.


Case Summary
Our patient had left ventricular dysfunction, non-invasive functional assessment demonstrating ischemia, and angiographically moderate/severe multi-vessel disease. In a large number of practices this would have led to an “ischemic cardiomyopathy” label followed by revascularization along with optimized medical therapy. Subsequent improvement in ejection fraction would have erroneously been attributed to revascularization.
In summary, we present a case of cardiomyopathy with coincidental coronary artery disease - treated medically with normalization of structure and function on cardiac MRI. Invasive physiology gave us robust grounds to defer revascularization and optimize medical therapy.
In summary, we present a case of cardiomyopathy with coincidental coronary artery disease - treated medically with normalization of structure and function on cardiac MRI. Invasive physiology gave us robust grounds to defer revascularization and optimize medical therapy.


