Lots of interesting abstracts and cases were submitted for TCTAP 2022. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-175
Valve-In-Valve Transcatheter Aortic Valve Replacement in a Patient With Severe Left Ventricular Systolic Dysfunction in Previous Bentall Procedure
By Satej Sadashiv Janorkar, Sachin Shirke, Prashant Mishra, Nilesh Juvekar
Presenter
Satej Janorkar
Authors
Satej Sadashiv Janorkar1, Sachin Shirke2, Prashant Mishra2, Nilesh Juvekar2
Affiliation
Deenanath Mangeshkar Hospital & Research Center, India1, Deenanath Mangeshkar Hospital, India2,
View Study Report
TCTAP C-175
STRUCTURAL HEART DISEASE - Valvular Intervention: Aortic
Valve-In-Valve Transcatheter Aortic Valve Replacement in a Patient With Severe Left Ventricular Systolic Dysfunction in Previous Bentall Procedure
Satej Sadashiv Janorkar1, Sachin Shirke2, Prashant Mishra2, Nilesh Juvekar2
Deenanath Mangeshkar Hospital & Research Center, India1, Deenanath Mangeshkar Hospital, India2,
Clinical Information
Patient initials or Identifier Number
HR
Relevant Clinical History and Physical Exam
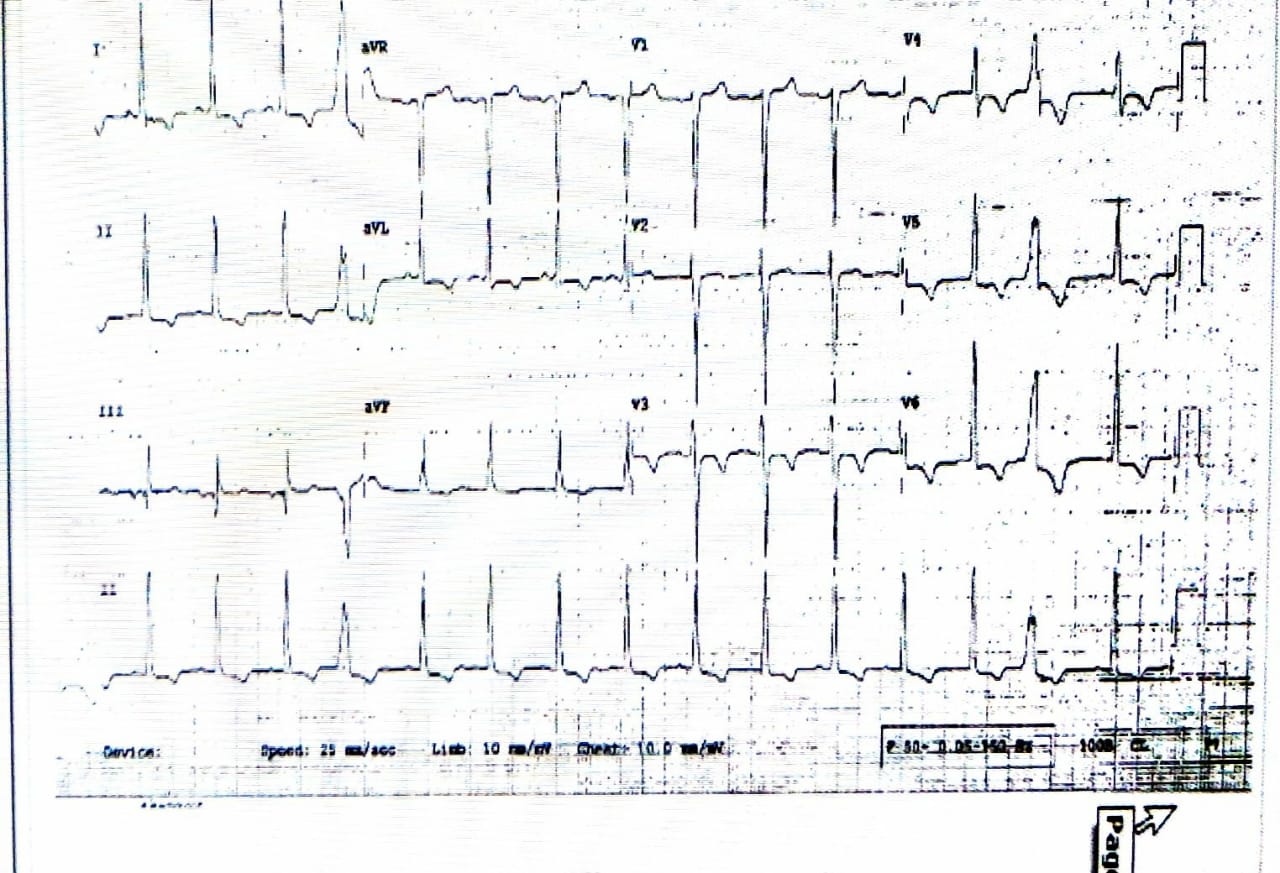
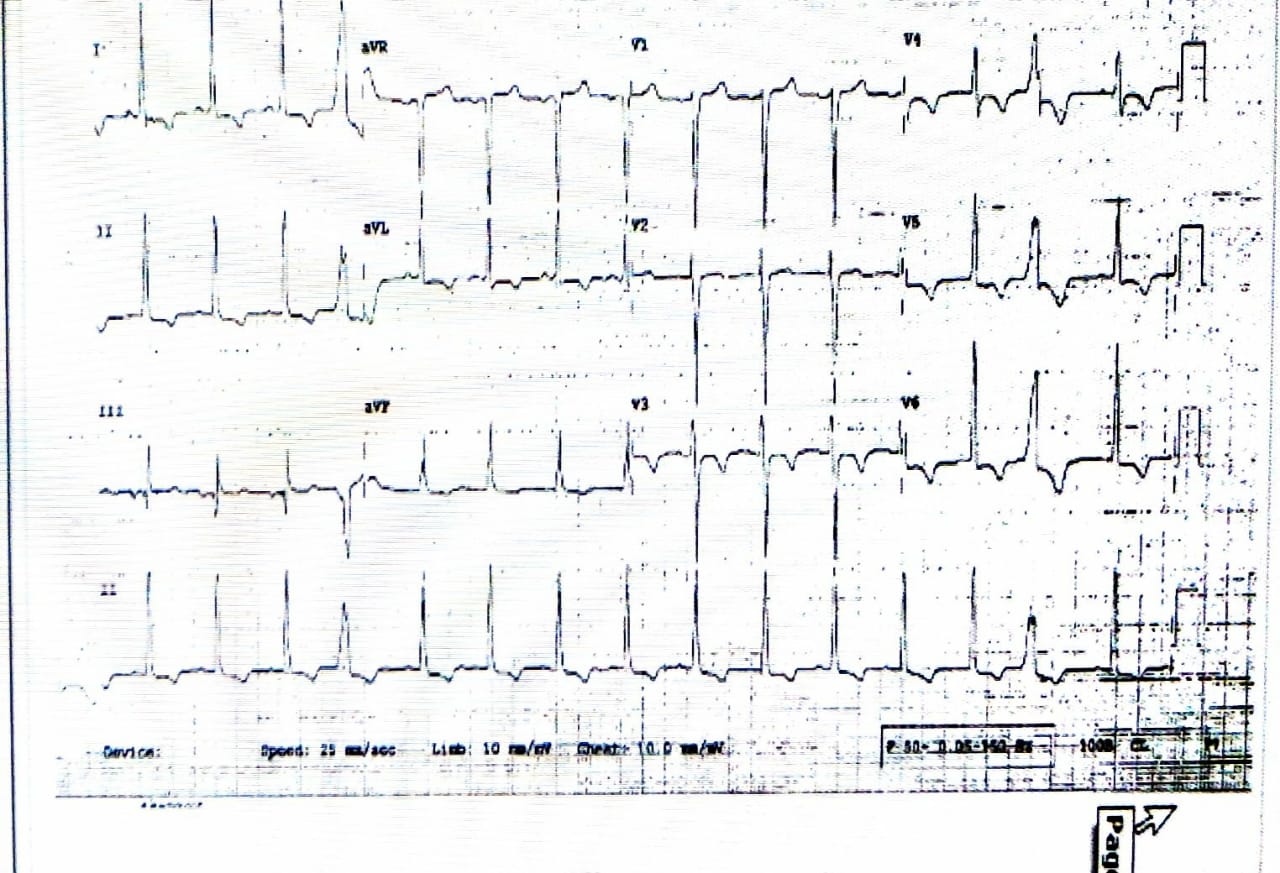
62 year old male with known Type 2 Diabetes mellitus and Hypertension and a history of Bentall Procedure (23 mm prosthesis-Perimount valve) in 2008 and a history of IE in 2012. NYHA Class III for last 3 months. BP 130/80 mm Hg. ECG showed LVH with strain and 2D echo showed severe increased transaortic gradients with severe LV systolic dysfunction, LVEF 25%. Surgeon declined re-do procedure.
Relevant Test Results Prior to Catheterization
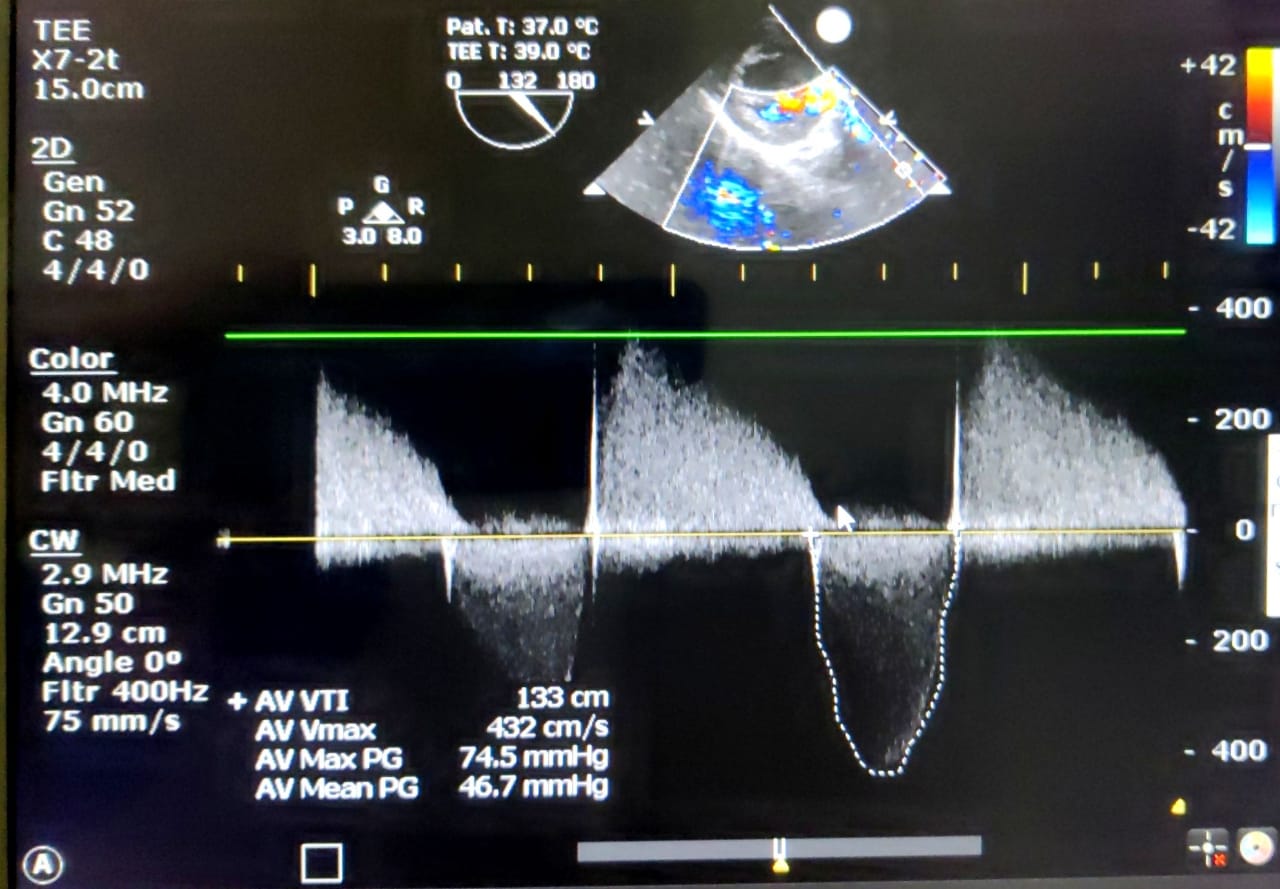
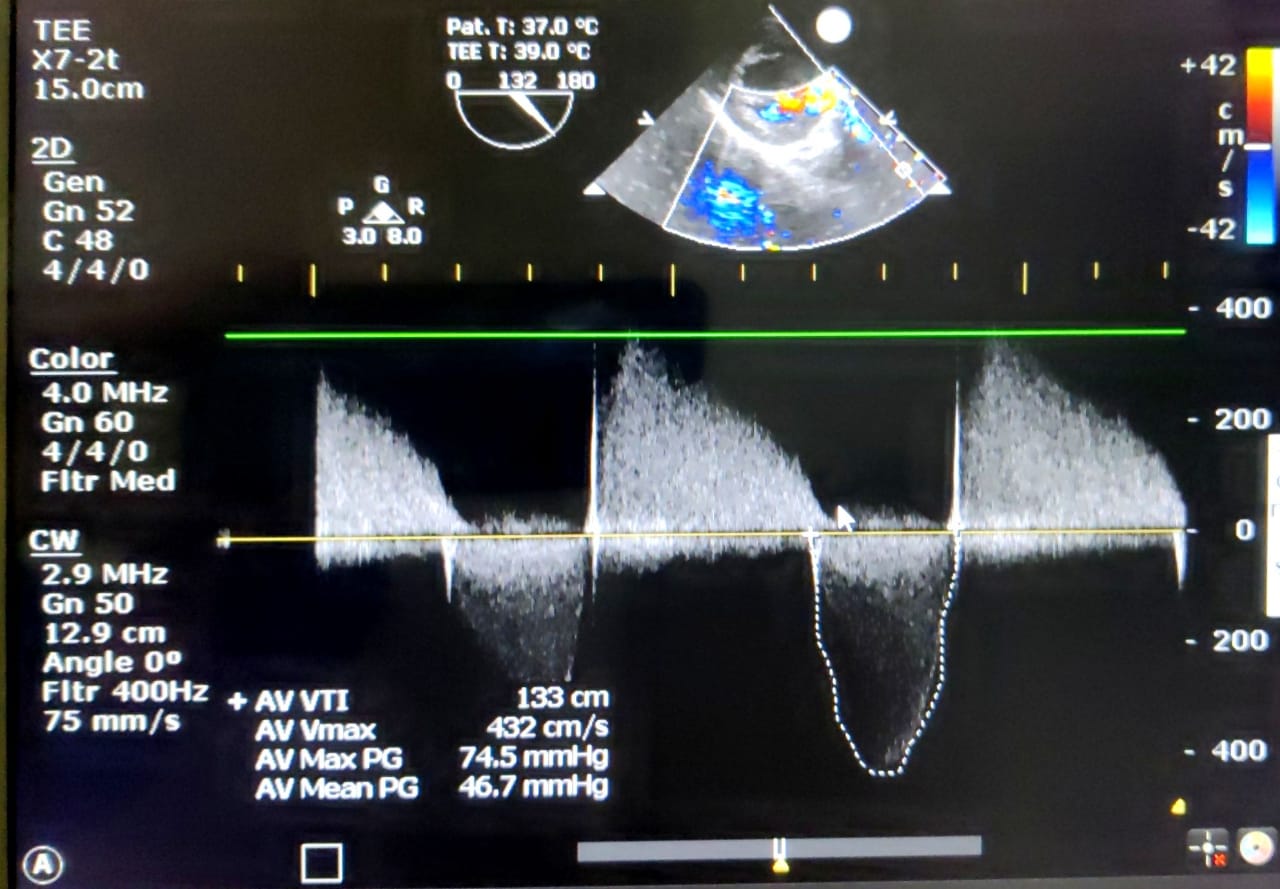
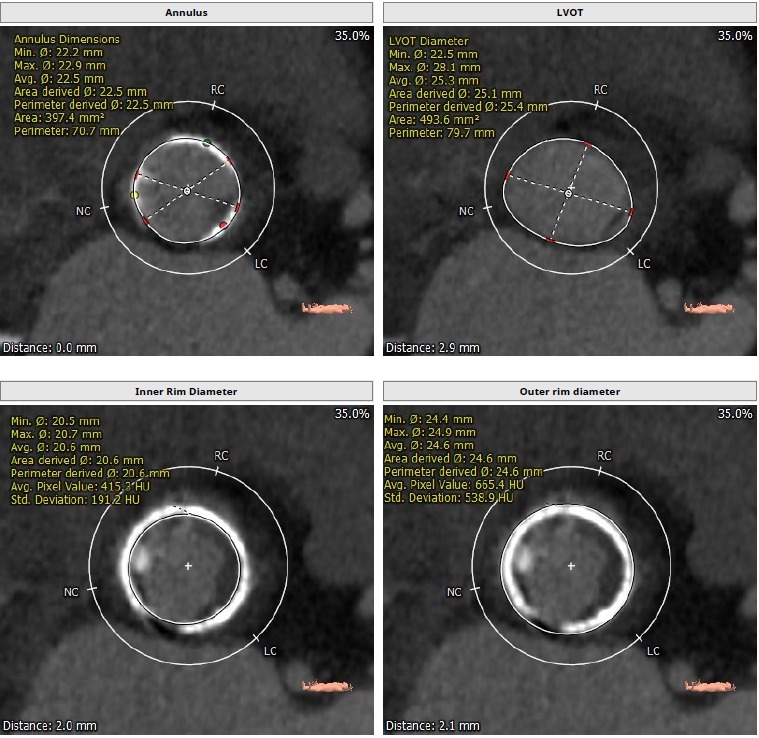
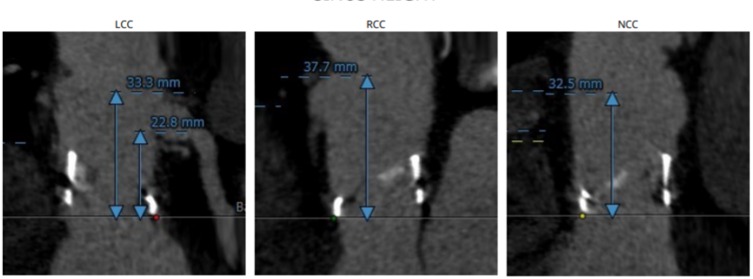
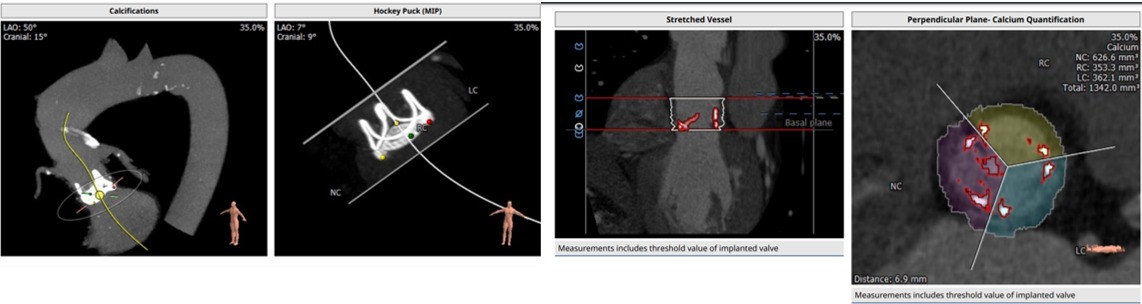
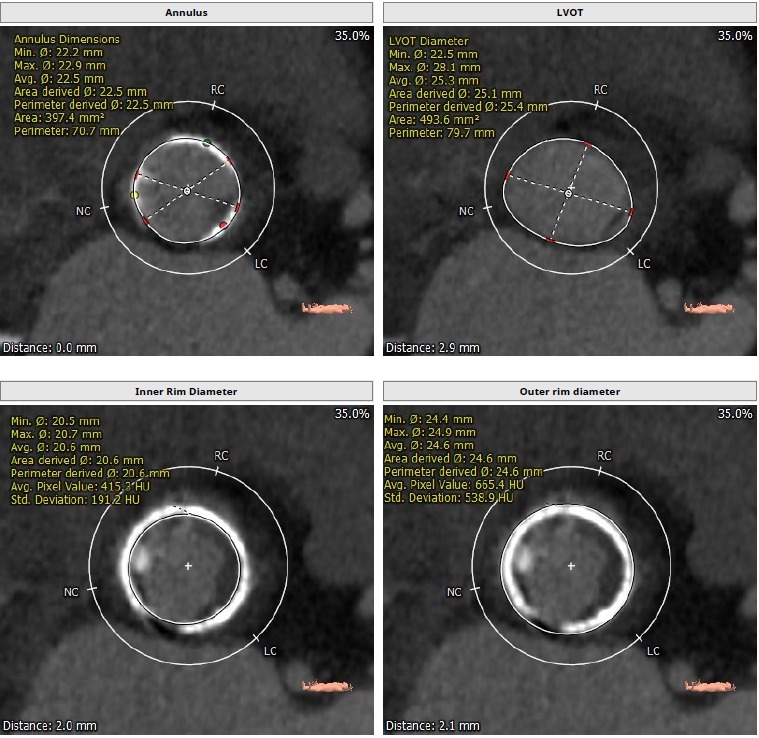
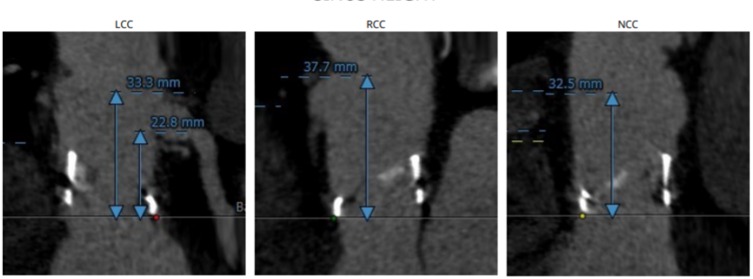
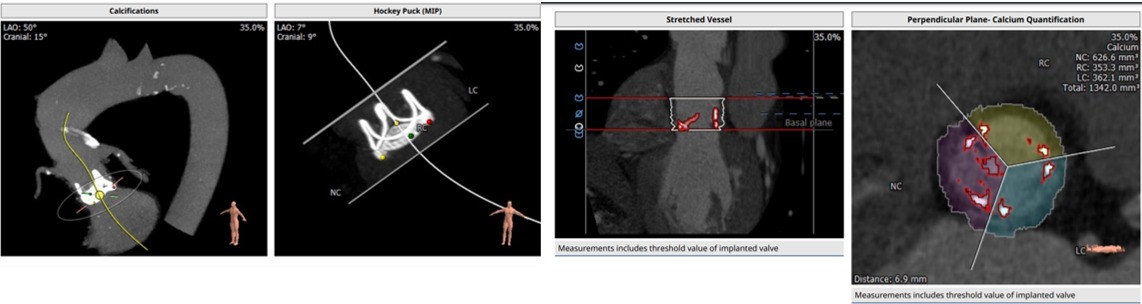
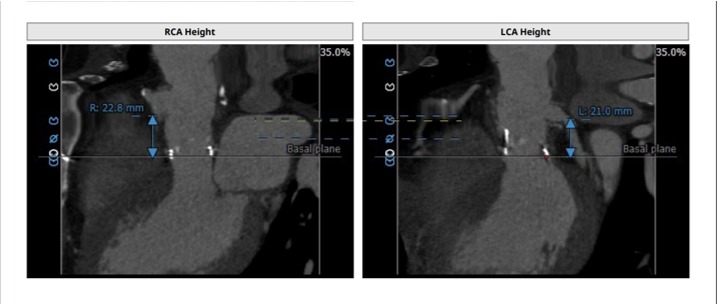
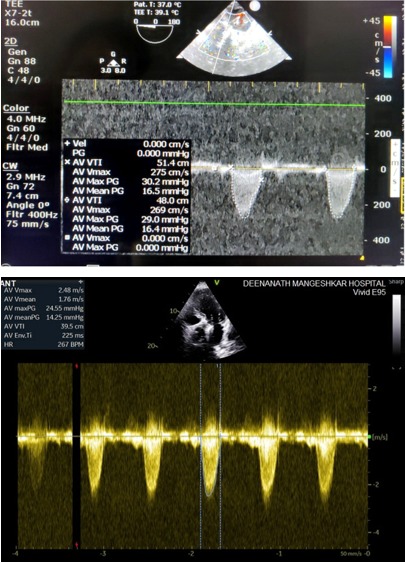
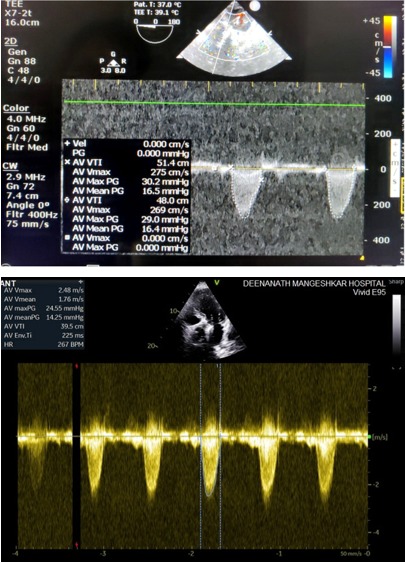
TEE showed AV prosthesis with conduit in situ with increased systolic gradients across it, 78/39 mm Hg, with moderate AR with a reduced systolic function (LVEF: 30%). CAD was excluded by CT Angiography. The annulus was 22.2 x 22.9 mm, the Sinus of Valsalva was 25.4 × 25.4 × 26.2 mm, ascending aorta diameter was 28.1 mm. Distance between annulus and left coronary artery ostium was 22.8 mm and distance with the right coronary artery ostium was 30 mm.
Relevant Catheterization Findings
Interventional Management
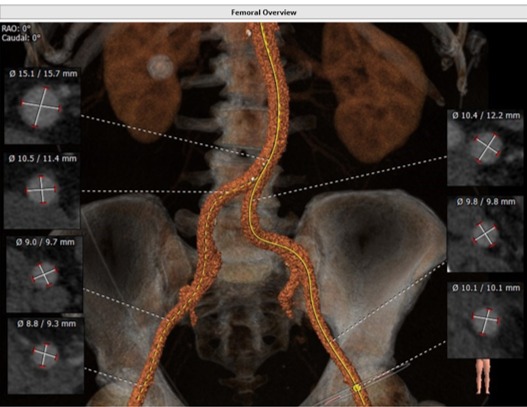
Procedural Step
The procedure was started with Femoral access with preclosure using 2 suture-mediated closure devices (Perclose ProGlide®, Abbott Laboratories, Abbott Park, IL) under general anaesthesia and TEE guidance. 6F AL1 catheter was passed through the valve delivery sheath over 0.035inch J Tipped guidewire and exchanged with straight tip wire to cross the valve which was then exchanged with Confida guidewire. The valve delivery system attempted to navigate a turn but failed. So Lunderquist® wire (Cook, USA) also was utilised which acted as a buddy system. Self expandable valve Evolut R 26 mm (Medtronic, USA) was implanted under rapid ventricular pacing, using a standard technique via a 14 F femoral sheath followed by post-dilatation using the 23 mm True Dilatation balloon (Medtronic, USA). TEE confirmed accurate positioning of the valve. TEE and hemodynamics confirmed the absence of gradient and of relevant AR (max gradient 16 mm Hg, mean gradient 6 mm Hg). No complications observed during or after the procedure. Device site closure was done with angioseal. TEE repeated after three days showed good function of valve and absence of paravalvular leak. Patient discharged 4 days later with significant symptomatic improvement documented in two weeks follow up. TTE showed max gradient 14 mm Hg, mean gradient 6 mm Hg.
 PreDil.mp4
PreDil.mp4
 DepPD.mp4
DepPD.mp4
Case Summary
First Asian Valve in Valve procedure performed in previously done Bentall surgery with history of endocarditis and severe LV dysfunction. It demonstrated feasibility of TAVR with self expanding valve in setting of degenerated, perforated prosthesis. Challenges were absence of landmarks, calcification, stentless conduit and fully biological valve. Confida with Lunderquist wire acted as a buddy system in order to navigate the turn of conduit. Accurate planning, CT scan were crucial to choose correct valve and to determine the position of reimplanted coronary ostia, which were high in this case, mitigating the risk of coronary occlusion. Postdilatation was essential to achieve optimal result.


