Lots of interesting abstracts and cases were submitted for TCTAP 2022. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-062
Successful PCI for In-Stent CTO Assisted via IVUS-Guided Active Antegrade True-Lumen Seeking Technique: A Case Report
By Jing Xu, Yi Xu, Yuejin Yang
Presenter
Jing Xu
Authors
Jing Xu1, Yi Xu2, Yuejin Yang1
Affiliation
Fuwai Hospital, China1, The First Affiliated Hospital of Jinan University, China2,
View Study Report
TCTAP C-062
CORONARY - Chronic Total Occlusion
Successful PCI for In-Stent CTO Assisted via IVUS-Guided Active Antegrade True-Lumen Seeking Technique: A Case Report
Jing Xu1, Yi Xu2, Yuejin Yang1
Fuwai Hospital, China1, The First Affiliated Hospital of Jinan University, China2,
Clinical Information
Patient initials or Identifier Number
Liu
Relevant Clinical History and Physical Exam
A 73-year-old male was admitted to our hospital due to worsen of chest pain and tightness for a month. He went to the local hospital again in 2015 where he received coronary angiogram and was discovered to have coronary stenosis (LAD [proximal]: 70% stenosis, LCX [distal]: 100% stenosis, RCA: 60% stenosis). He was then implanted with 3 stents (2 in LCX and 1 in left main [LM]-LAD).
Relevant Test Results Prior to Catheterization
His comorbidities include hypertension and hyperlipidemia. Physical examination showed no remarkable findings. Echocardiogram (at admission) showed a left ventricle end diastolic diameter of 53mm and ejection fraction of 61%.
Relevant Catheterization Findings
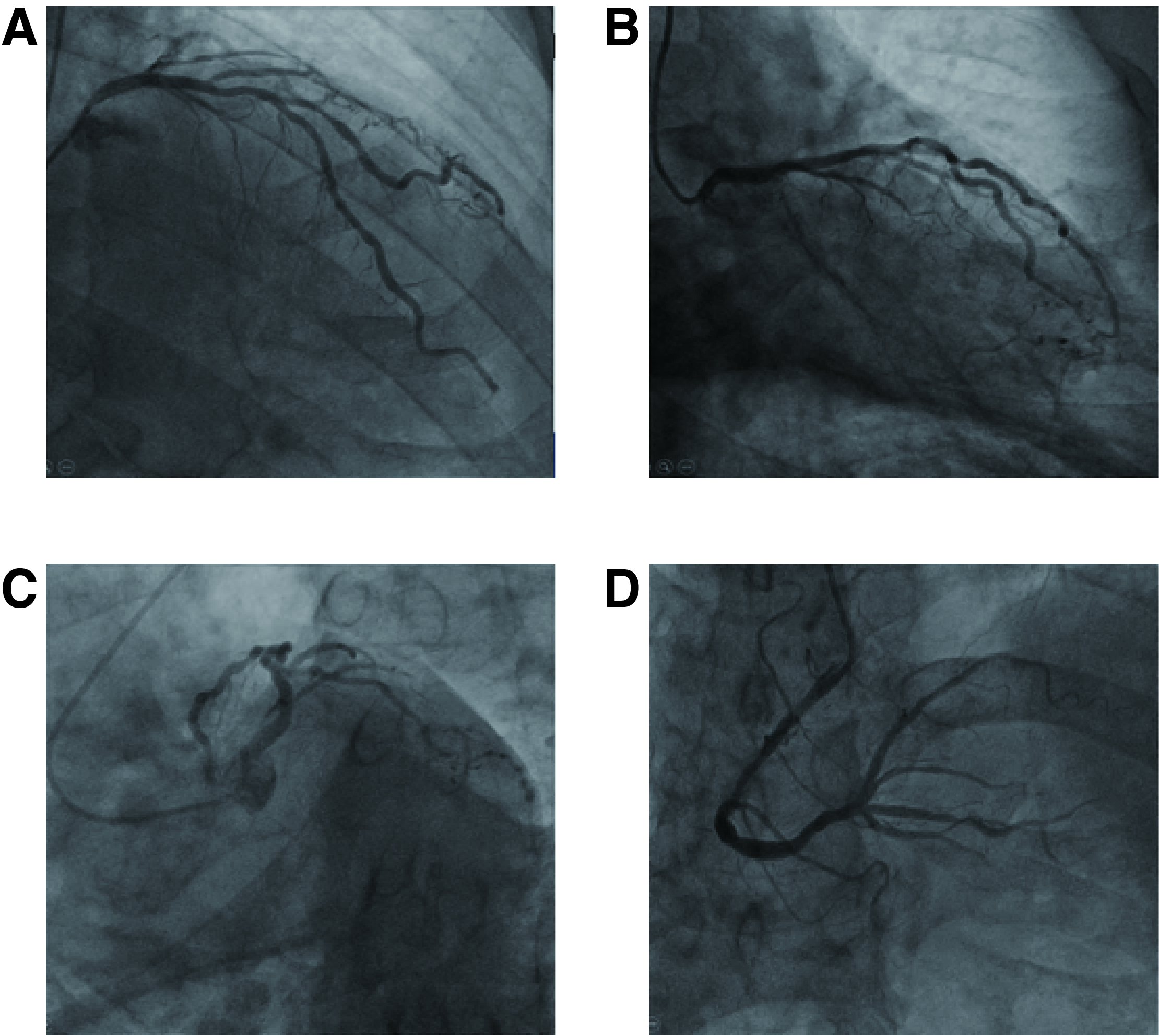
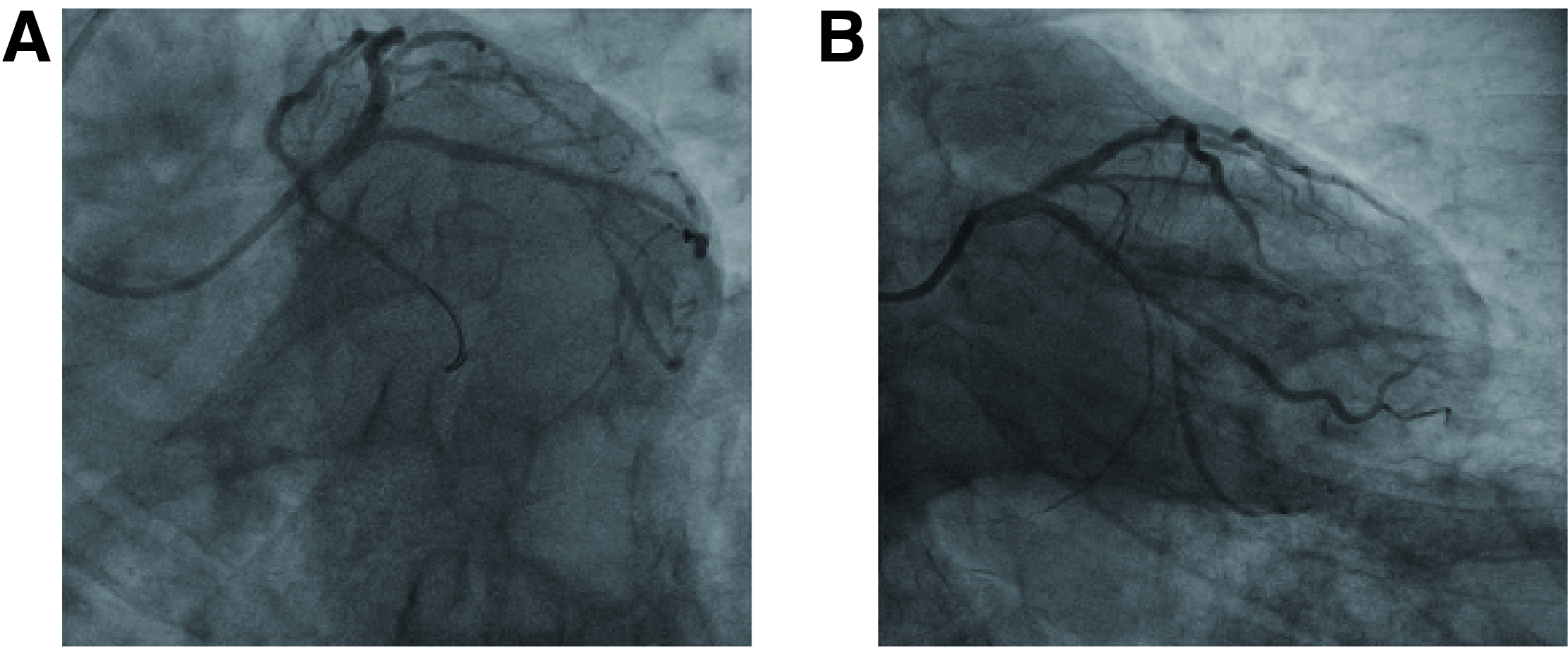
Coronary angiogram was performed via the right transradial approach using a 5F radial Tig. It showed that the LM-LAD stent was patent, but ostial LCX had in-stent chronic total occlusion (IS-CTO). Middle RCA had 50% stenosis and posterior descending artery had 70% (Figure 1).
Interventional Management
Procedural Step
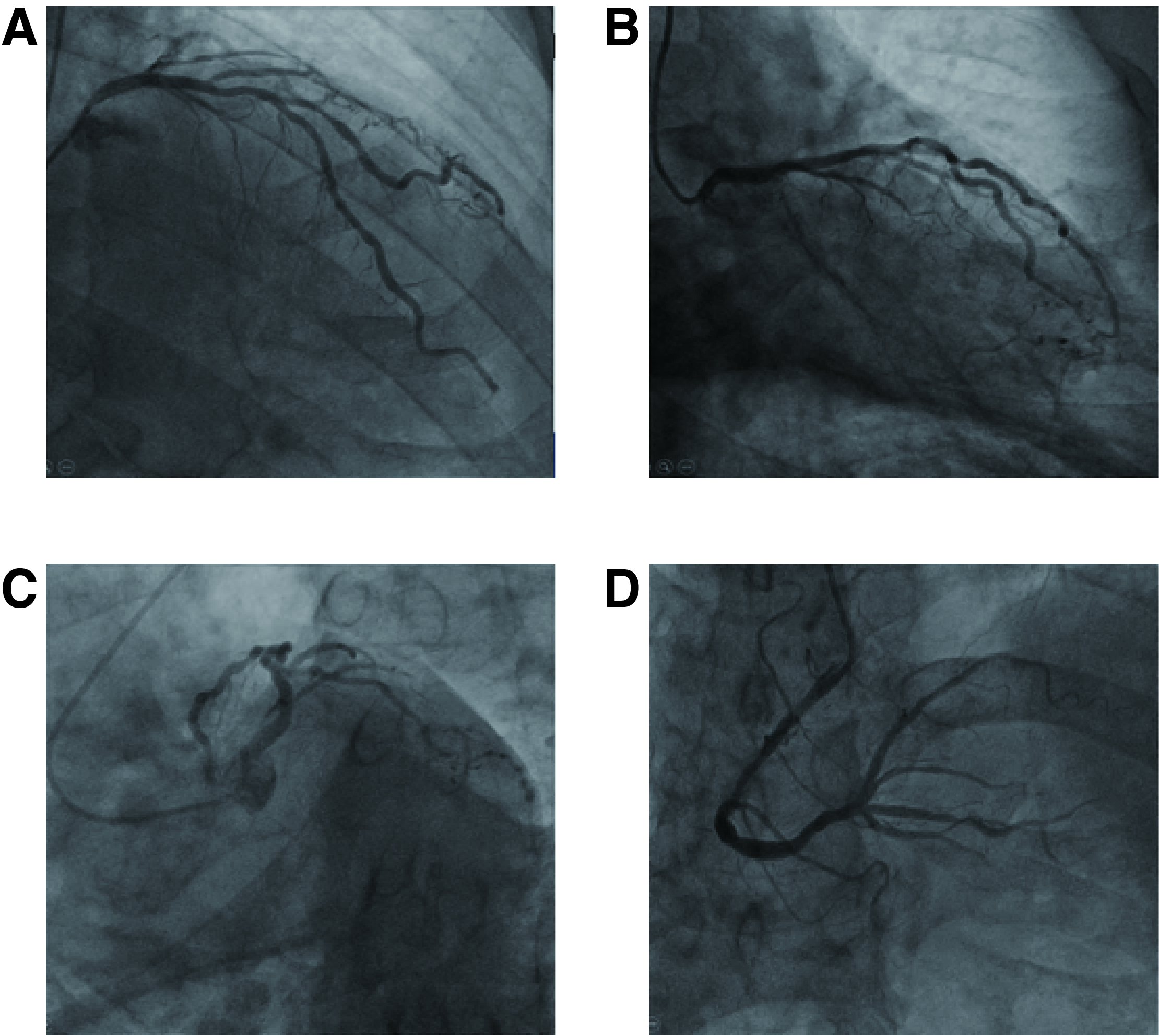
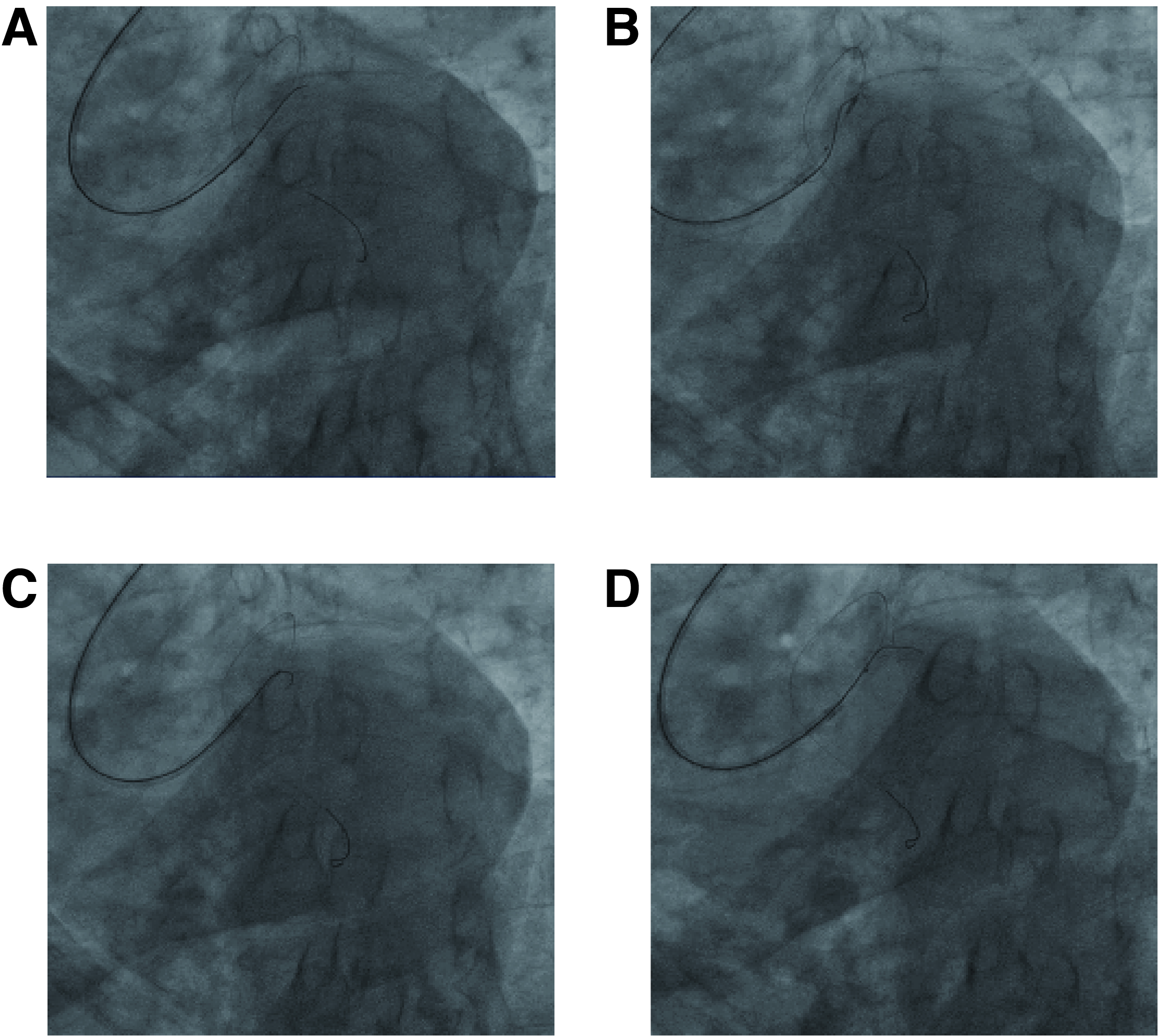
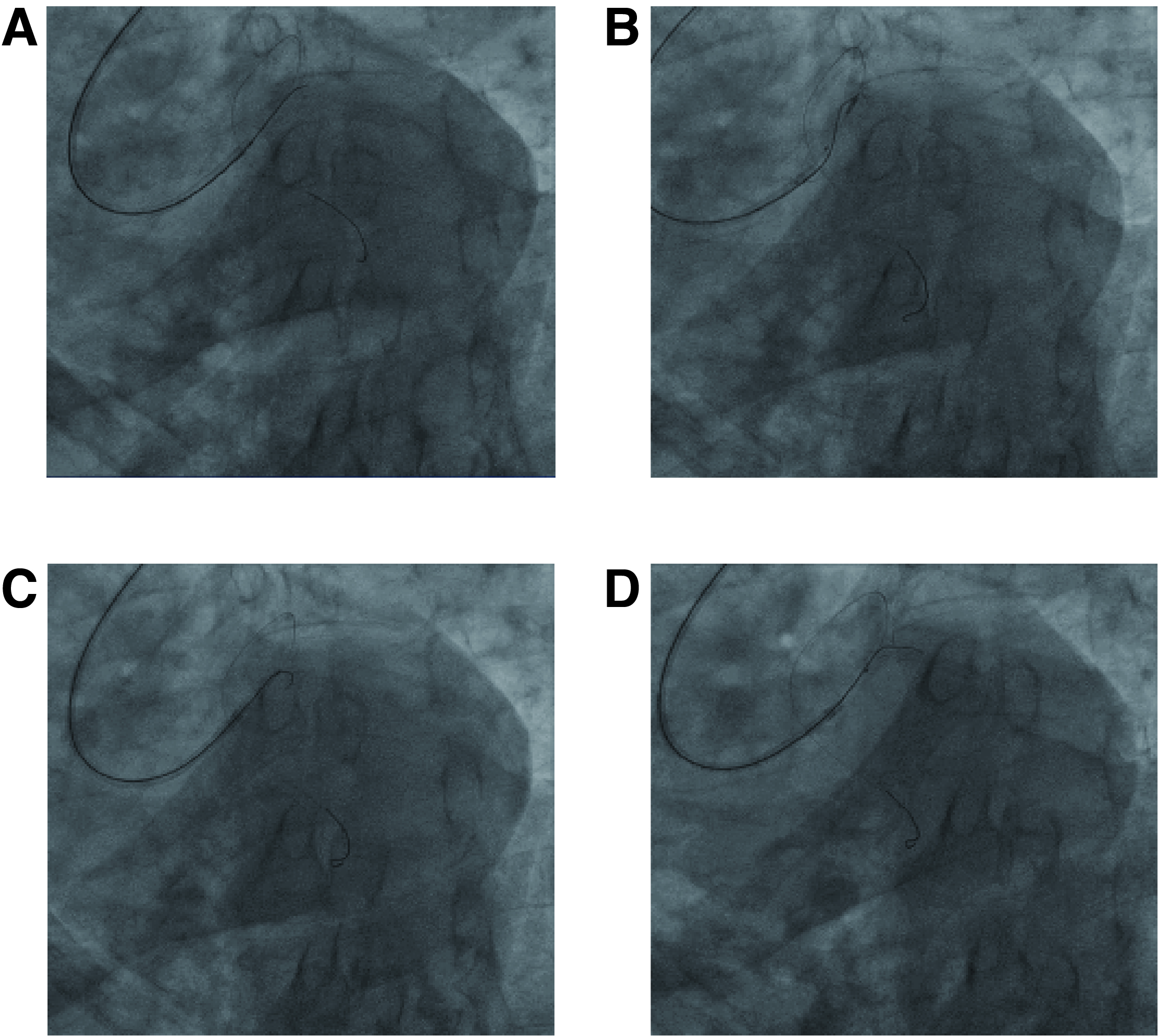
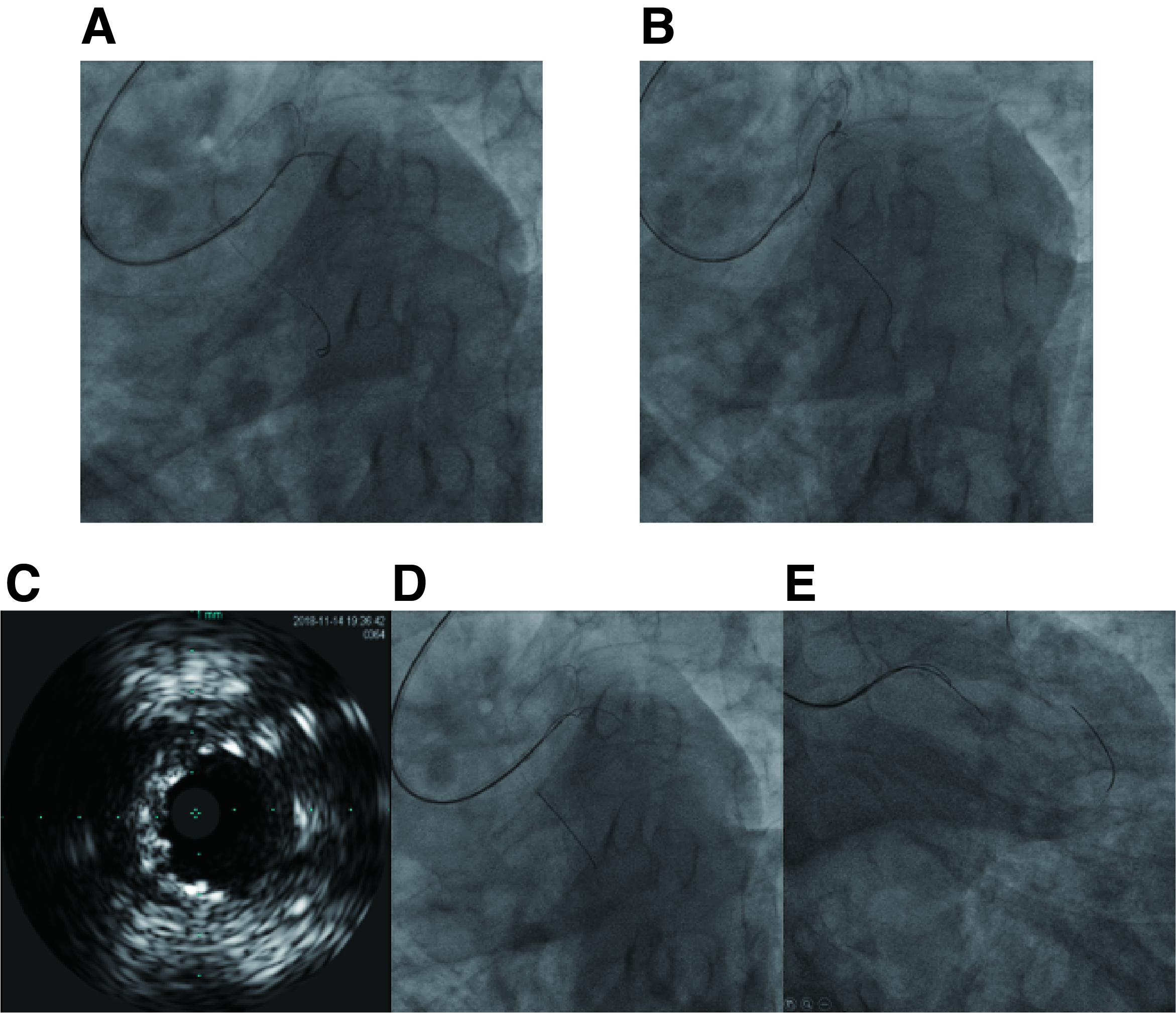
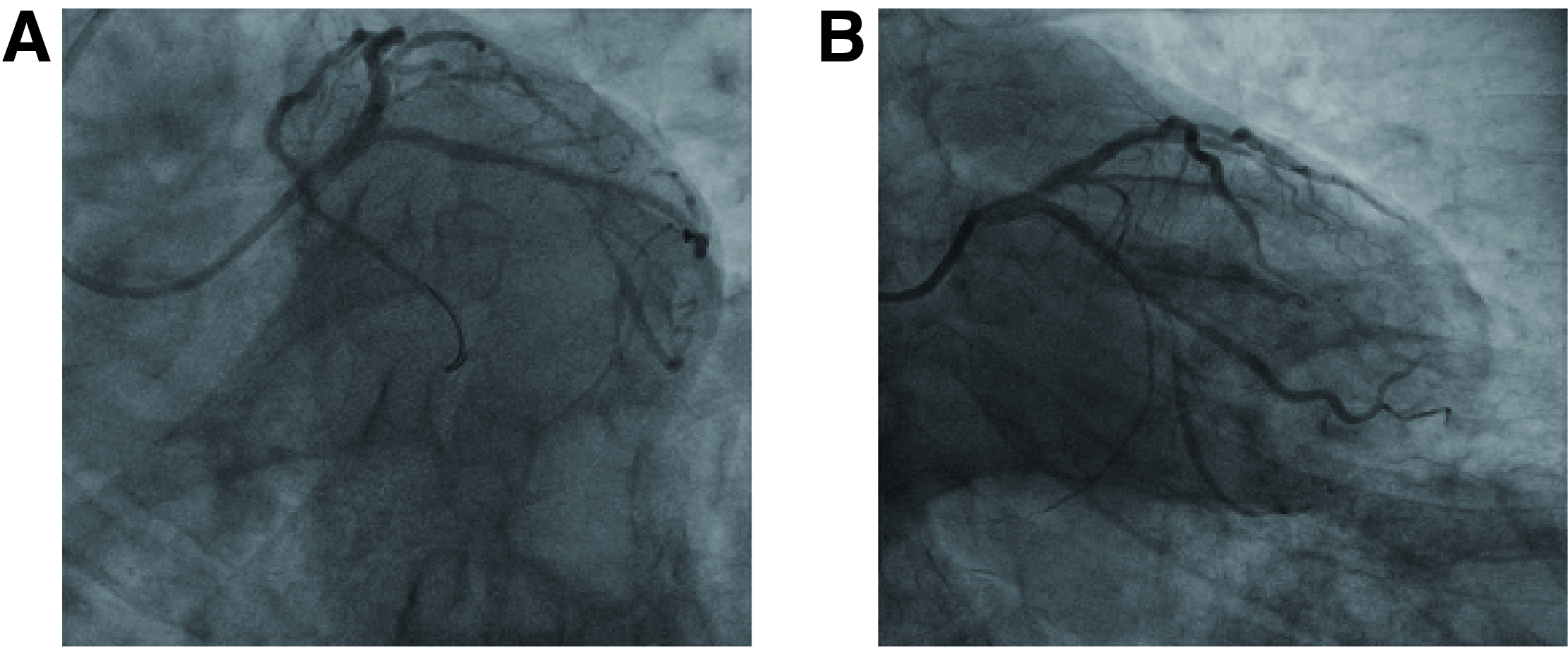
The left coronary system was engaged with EBU 3.5-6F guiding catheter. A BMW universal wire was advanced to distal LAD. Under Finecross support, our first few attempts to find entry failed unsurprisingly. The LCX-CTO lesion could not be crossed with one- or two-bend wires. The wires either went into the wrong direction or went right direction but outside stent (Figure 2). We then decided to use the wire that went outside stent as a roadmap and advance another wire with help of IVUS guidance. The “new” wire was advanced slowly with tip-rotation. After another few failed attempts with the second wire went into the inner curve, went outside stent, etc., a Conquest Pro guidewire was finally able used to go through the true lumen. The micro-catheter was then advanced and a BMW wire was exchanged. The LCX lesion was first pre-dilated with Sapphire 1.0*10mm and Sequent 2.5*15mm balloons at 16-20 atm. It was then pre-dilated using a 3.0*13mm Lacross NSE scoring balloon up to 20 atm. After pre-dilation, a Sequent Please 3.0*30mm drug-coated balloon (DCB) was deployed at the LCX lesion at 16 atm for 40 seconds. LAD was dilated by another Sequent Please DCB (3.5*26mm) at 16 atm for 40 seconds. The procedure was finished by post-dilation at LCX and LAD with two Empira 3.5*15mm balloons (24 atm) and a kissing at 14 atm (Figure 3). Angiography re-evaluation showed TIMI 3 flow with no complications, indicating a successful procedure (Figure 4).
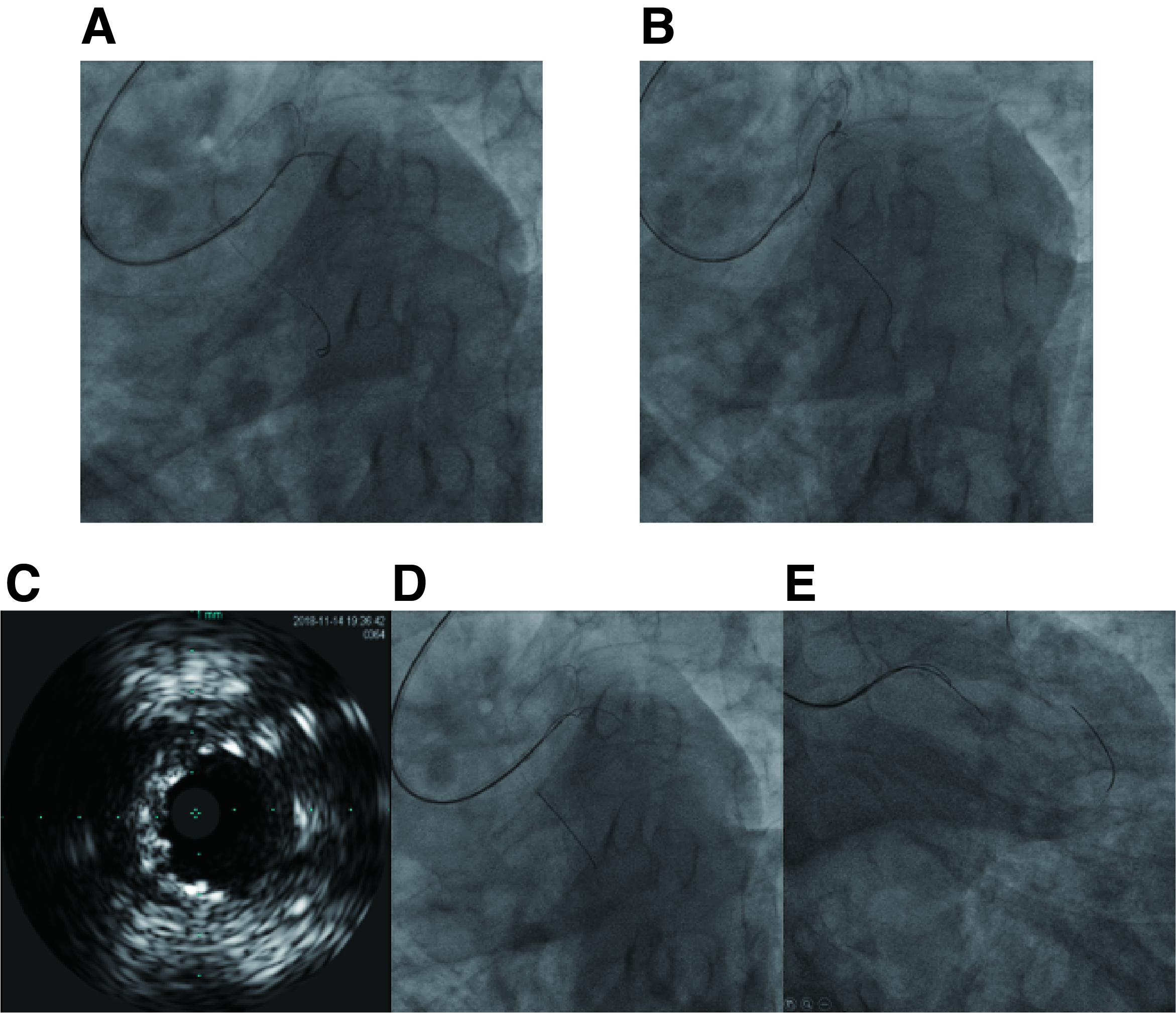
Case Summary
Our successful PCI for this intra-stent LCX-CTO lesion suggests that IVUS-ATS technique might be suitable for these complicated CTO lesions. It could also play a more important role in CTO lesions with inappropriate or failed traditional antegrade or retrograde techniques.


