Lots of interesting abstracts and cases were submitted for TCTAP 2022. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-006
Emergency Complex Left Main Bifurcation PCI in a Case of NSTEMI With Pulmonary Edema and Cardiogenic Shock: Should We Strive for Angiographic Perfection in Unfavorable Anatomy?
By Vipin Thomachan, Ali Shamsi, Ahmed Siddiqui, Gohar Jamil
Presenter
Vipin Thomachan
Authors
Vipin Thomachan1, Ali Shamsi1, Ahmed Siddiqui1, Gohar Jamil1
Affiliation
Tawam Hospital, United Arab Emirates1,
View Study Report
TCTAP C-006
CORONARY - Acute Coronary Syndromes (STEMI, NSTE-ACS)
Emergency Complex Left Main Bifurcation PCI in a Case of NSTEMI With Pulmonary Edema and Cardiogenic Shock: Should We Strive for Angiographic Perfection in Unfavorable Anatomy?
Vipin Thomachan1, Ali Shamsi1, Ahmed Siddiqui1, Gohar Jamil1
Tawam Hospital, United Arab Emirates1,
Clinical Information
Patient initials or Identifier Number
SM
Relevant Clinical History and Physical Exam
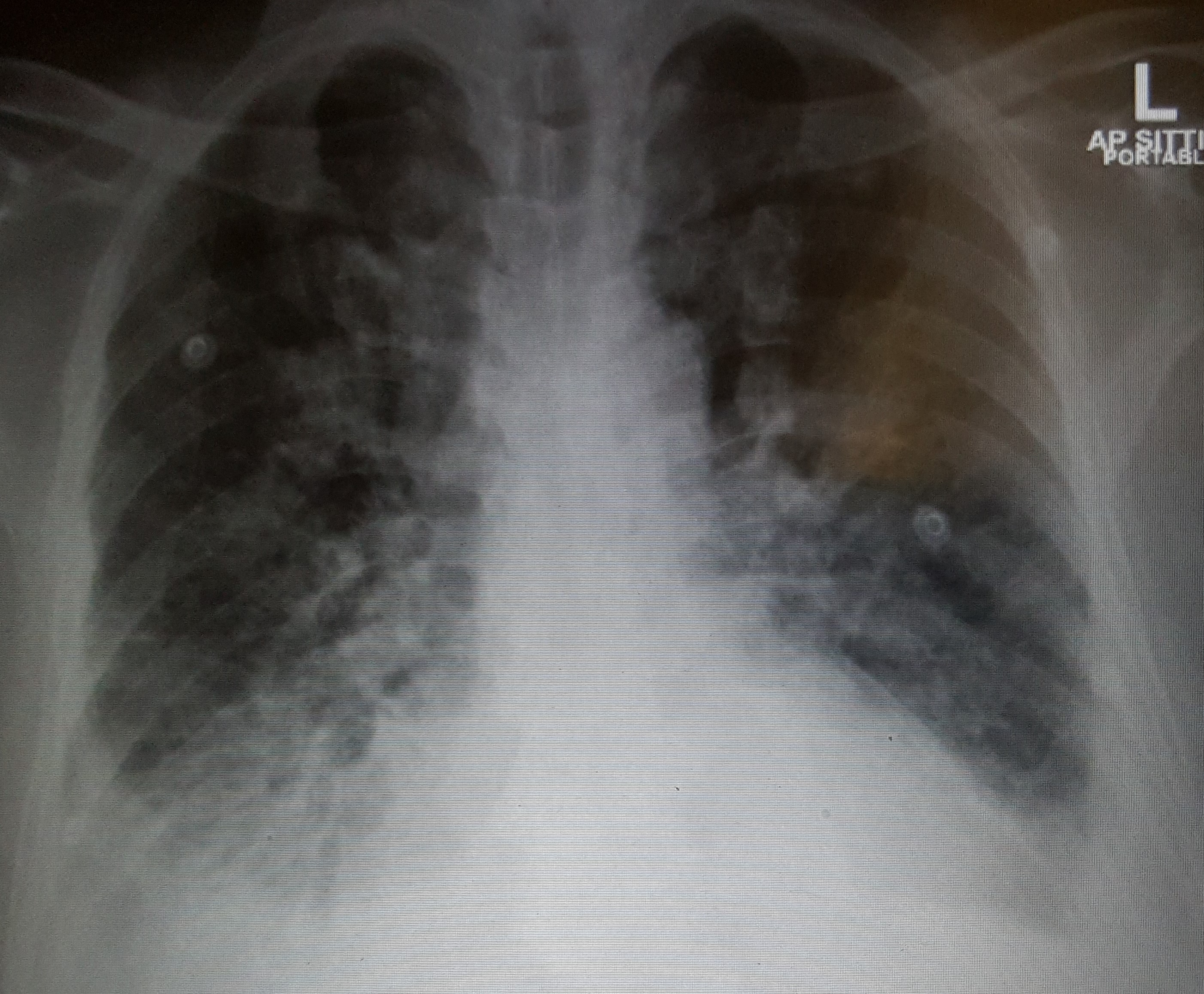
This 77-year-old male patient presented to ED with complaints of dyspnea,cough and chest discomfort of 3 days duration which worsened on the day ofadmission. He has a known case of hypertension, diabetes, dyslipidemia,bronchial asthma and CAD with history of coronary intervention in the remotepast, the details of which were not available.
He was tachypneic with respiratory rate 38/min, SpO2 86%, HR 111 bpm, BP91/61 mm Hg.
He had bilateral rhonchi with crepitation and muffled heart sounds.
He was tachypneic with respiratory rate 38/min, SpO2 86%, HR 111 bpm, BP91/61 mm Hg.
He had bilateral rhonchi with crepitation and muffled heart sounds.
Relevant Test Results Prior to Catheterization
ECG showed sinus tachycardia with diffuse ST-Tchanges in inferolateral leads and poor R progression in anterior leads.
Blood investigations revealed acute kidney injury on CKD, elevated cardiactroponin and NT-proBNP.
Sodium 136mmol/L
Potassium 3.7mmol/L
Creatinine 187micromol /L
Urea 12.8mmol/L
eGFR 33mL/min/1.73m2
Hb 12.2gm/dL
Troponin 9.43micrg/L
NT-pro BNP 10388 ng/L
Echo: mid to distal septum, anterior wall and apex akinetic. Apical inferiorand posterolateral wall hypokinetic.
Blood investigations revealed acute kidney injury on CKD, elevated cardiactroponin and NT-proBNP.
Sodium 136mmol/L
Potassium 3.7mmol/L
Creatinine 187micromol /L
Urea 12.8mmol/L
eGFR 33mL/min/1.73m2
Hb 12.2gm/dL
Troponin 9.43micrg/L
NT-pro BNP 10388 ng/L
Echo: mid to distal septum, anterior wall and apex akinetic. Apical inferiorand posterolateral wall hypokinetic.
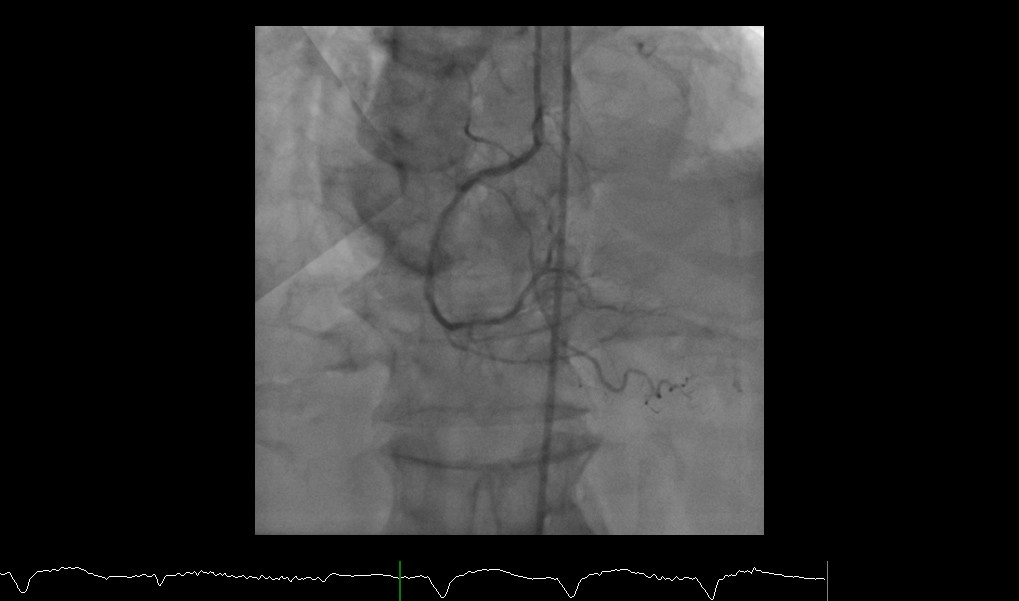
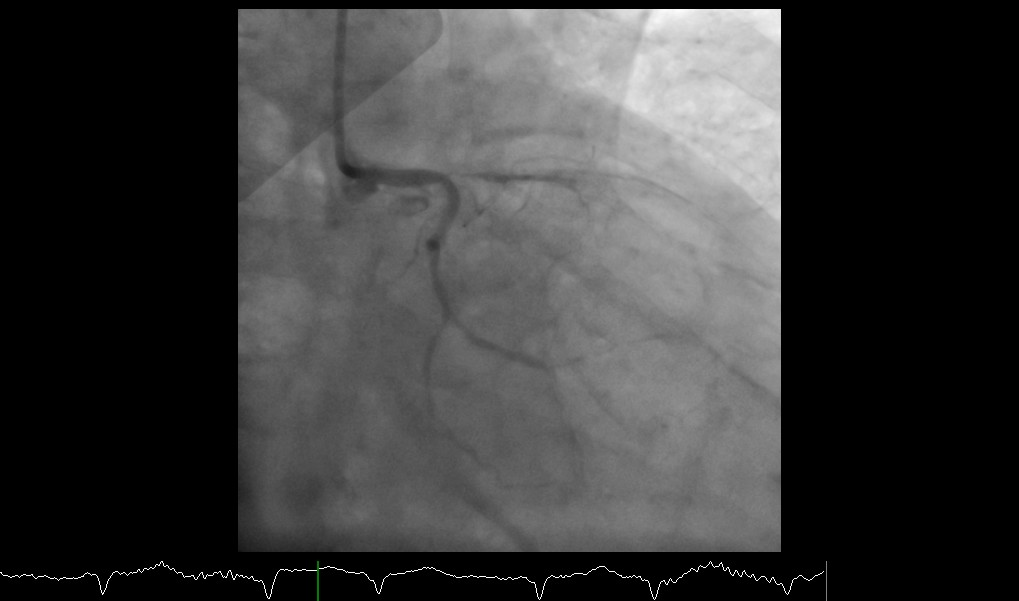
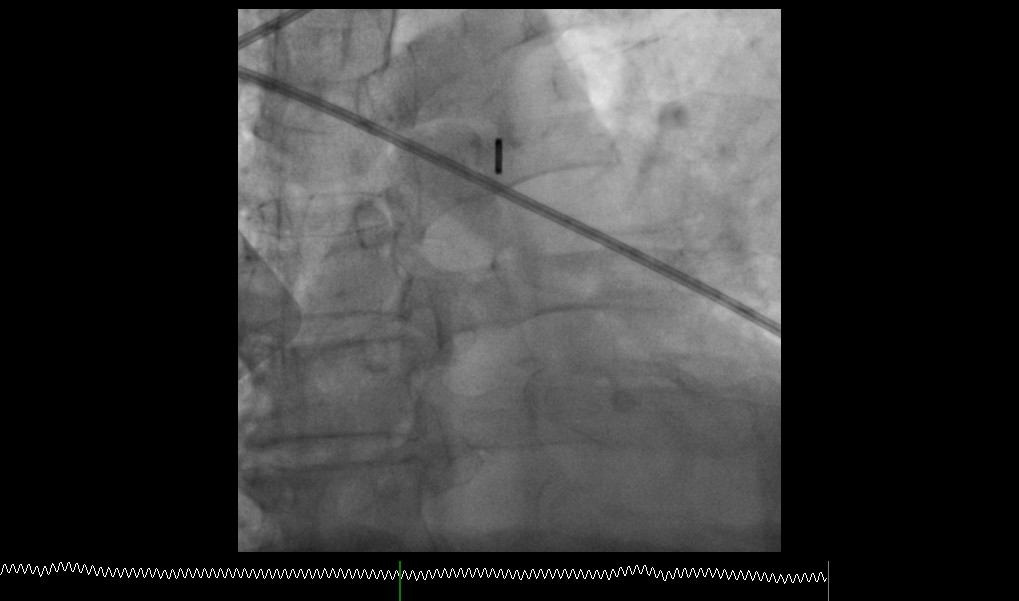
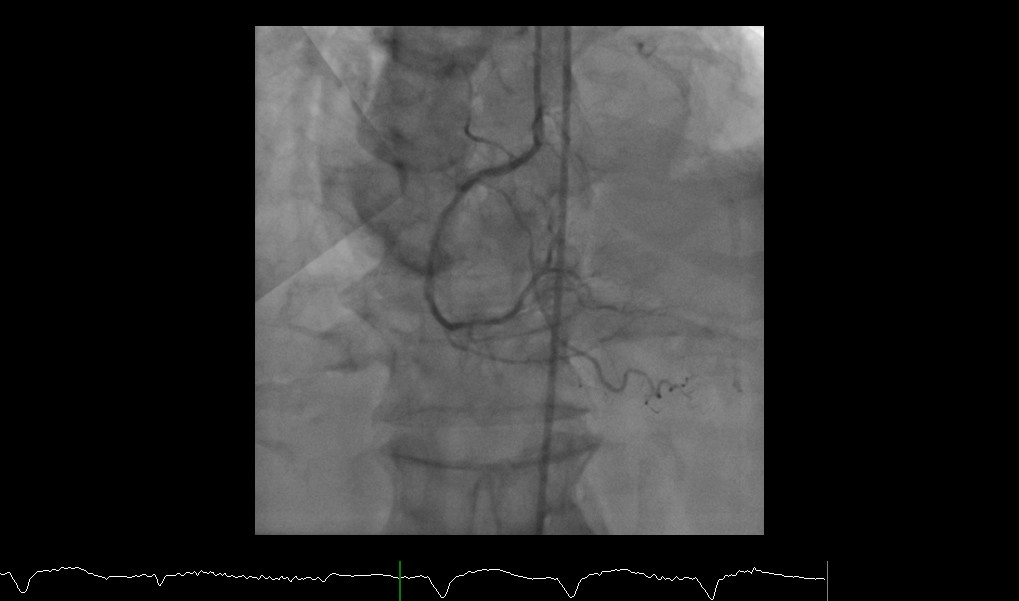
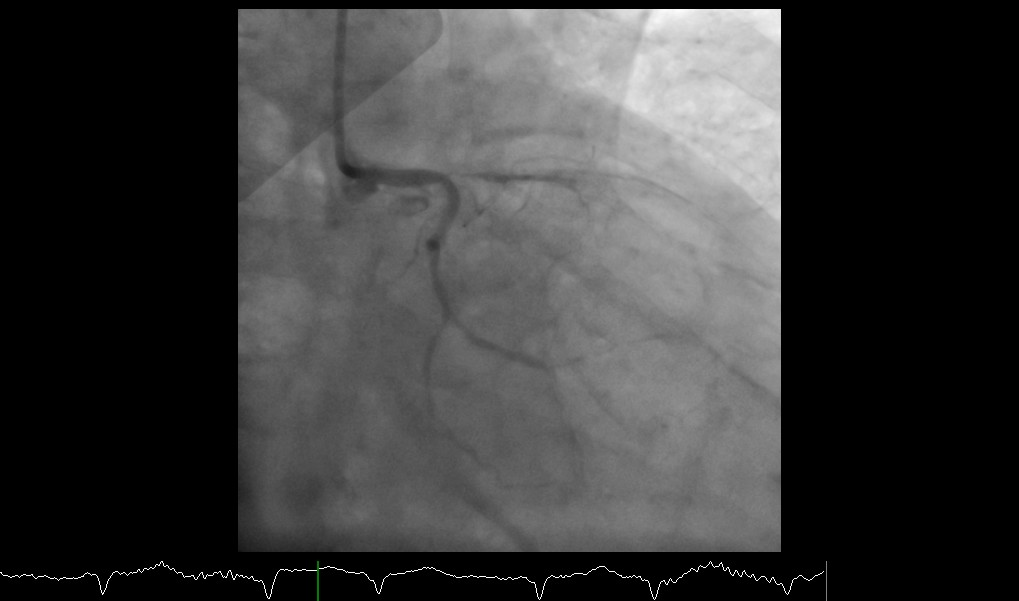
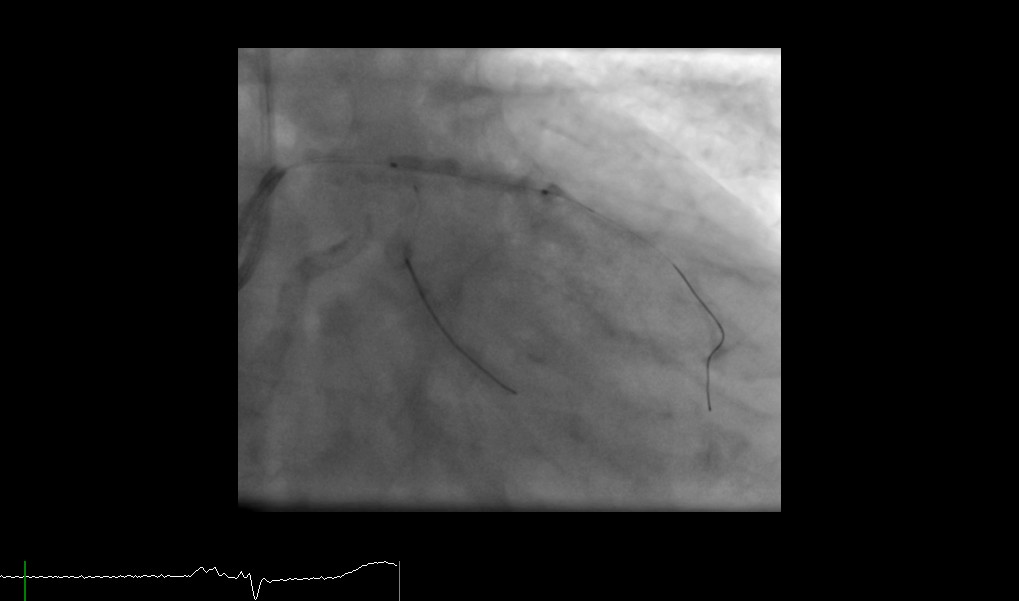
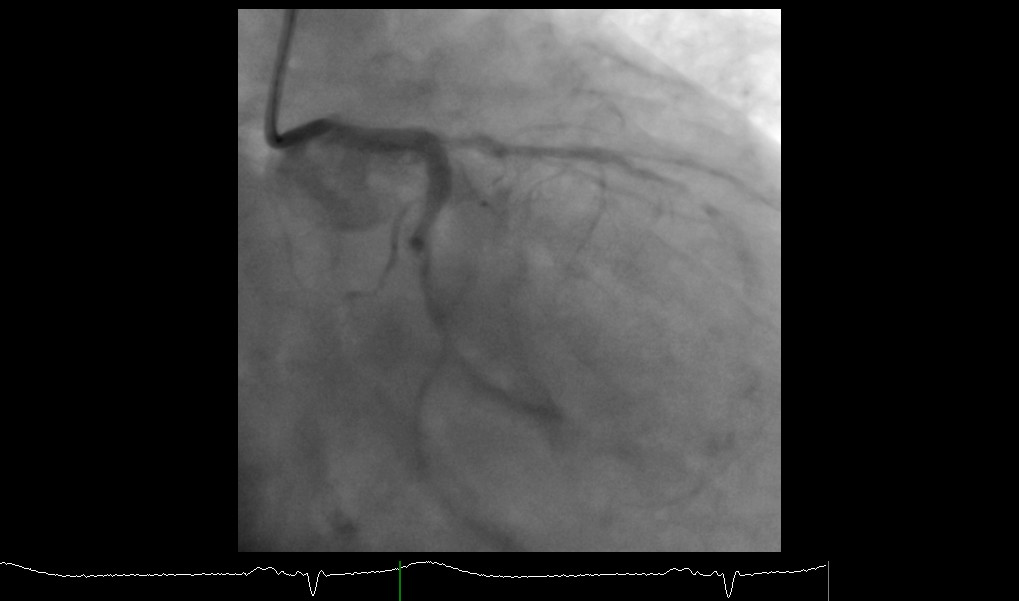
Relevant Catheterization Findings
LMCA: Tapering of distal left main with 60% stenosis.
LAD:
Severe (99%) stenosis of ostioproximal LAD.
Severely calcified vessel throughout.
Severe diffuse tubular stenosis throughout with total occlusion distally.
Diagonals-severe diffuse disease.
LCX:
Severe (95%)ostial stenosis
Moderate to severe stenosis of proximal segment at a sharp bend.
Moderate to severe diffuse tubular stenosis of distal LCX, OM1 and OM2.
RCA: Patent stent in proximal RCA.
Moderate diffuse disease throughout; calcified vessel.

LAD:
Severe (99%) stenosis of ostioproximal LAD.
Severely calcified vessel throughout.
Severe diffuse tubular stenosis throughout with total occlusion distally.
Diagonals-severe diffuse disease.
LCX:
Severe (95%)ostial stenosis
Moderate to severe stenosis of proximal segment at a sharp bend.
Moderate to severe diffuse tubular stenosis of distal LCX, OM1 and OM2.
RCA: Patent stent in proximal RCA.
Moderate diffuse disease throughout; calcified vessel.

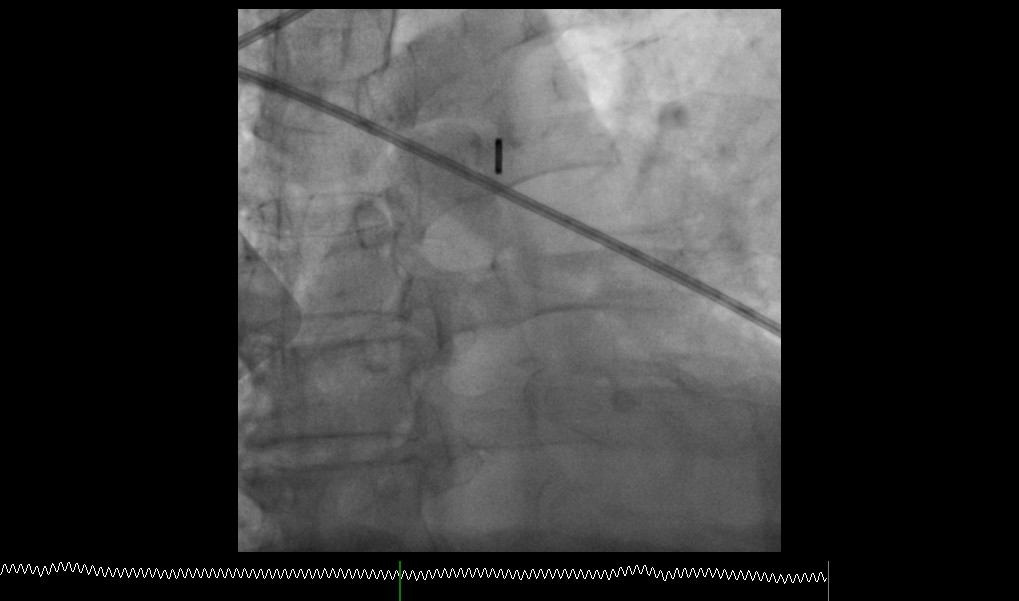
Interventional Management
Procedural Step
PCI - Left main to LAD(POBA&DEB) and left main to LCX with DES:
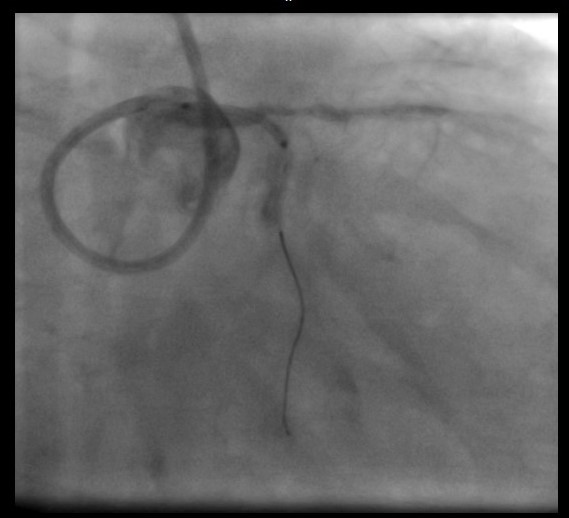
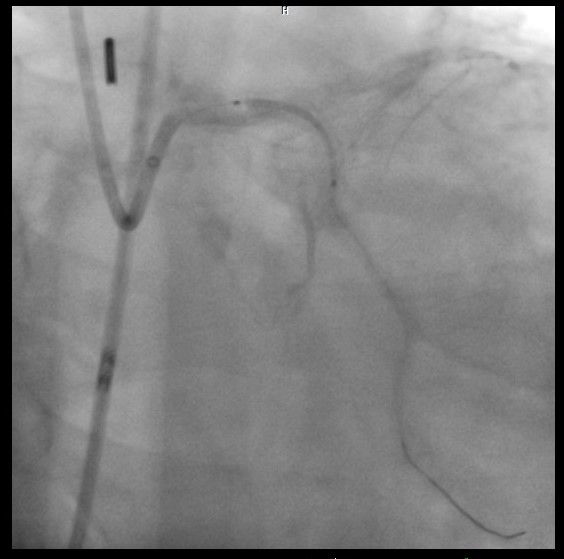
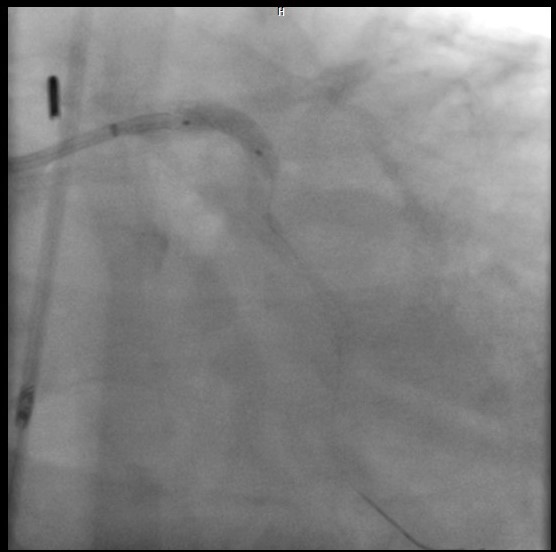
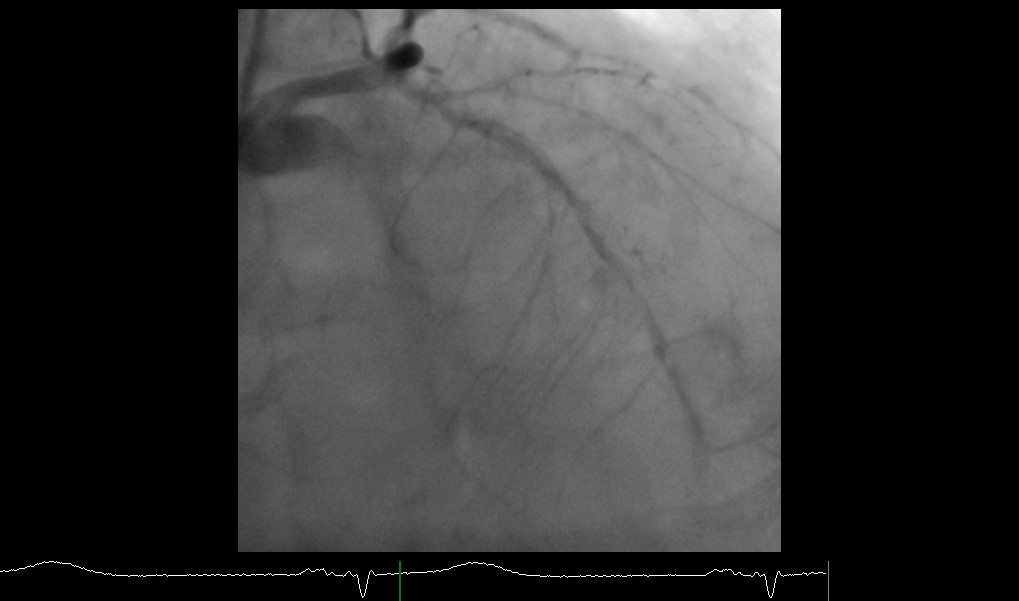
Case Summary
This 76-year-old gentleman who presented with ACS-NSTEMI and pulmonaryedema and impending shock developed VT and cardiogenic shock during CAG. He hadvery unfavorable coronary anatomy with left main bifurcationstenosis, severe diffuse disease with calcification and multiple stentsdeployed in the remote past. We did not strive for angiographic perfection as the main aim was tosave the patient with whatever revascularization possible. Ultimately, hewas revived and resuscitated with cardioversion, IABP,vasopressors and crucial revascularization.Patienthad a protracted course in the hospital with multiorgan failure but gotdischarged after 2 weeks of hospital stay and is on regular follow upnow.


