Lots of interesting abstracts and cases were submitted for TCTAP 2022. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-136
Retroperitoneal Haemorrhage in Tortuosity: When Nightmare Comes Late
By Muhammad Bachtiar Rahmat, Doni Firman, Suko Adiarto, Amir Aziz Alkatiri, Arwin Saleh Mangkuanom
Presenter
Muhammad Bachtiar
Authors
Muhammad Bachtiar Rahmat1, Doni Firman2, Suko Adiarto2, Amir Aziz Alkatiri2, Arwin Saleh Mangkuanom2
Affiliation
Budhi Asih General Hospital, Indonesia1, National Cardiovascular Center Harapan Kita, Indonesia2,
View Study Report
TCTAP C-136
ENDOVASCULAR - Complications
Retroperitoneal Haemorrhage in Tortuosity: When Nightmare Comes Late
Muhammad Bachtiar Rahmat1, Doni Firman2, Suko Adiarto2, Amir Aziz Alkatiri2, Arwin Saleh Mangkuanom2
Budhi Asih General Hospital, Indonesia1, National Cardiovascular Center Harapan Kita, Indonesia2,
Clinical Information
Patient initials or Identifier Number
YS
Relevant Clinical History and Physical Exam
Female, 64 years old, has chief complaint of easily fatigue during moderate activity. She had history of Inferior STEMI four months prior to recent admission, underwent primary PCI in RCA with 3VD. CAD risk factors: Hypertension and Dyslipidemia. Blood pressure 170/75 mmHg, heart rate 58 bpm, oxygen saturation 99% room air.
Relevant Test Results Prior to Catheterization
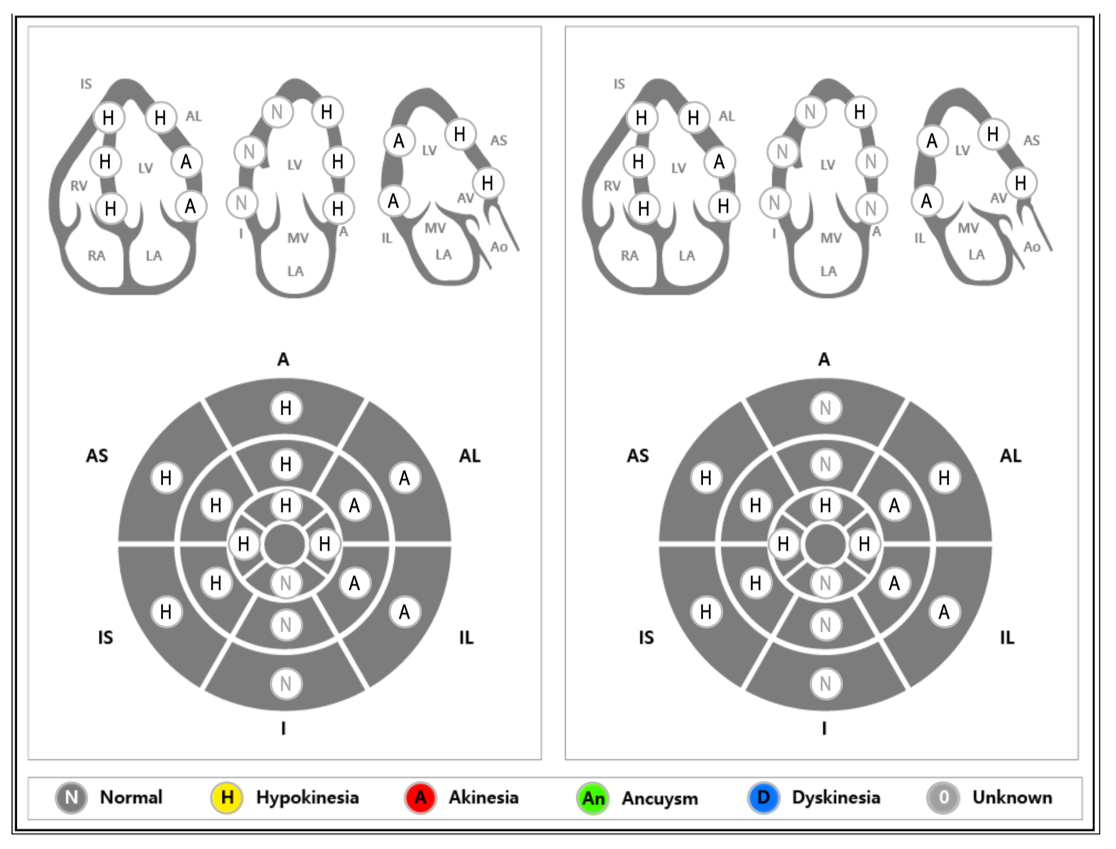
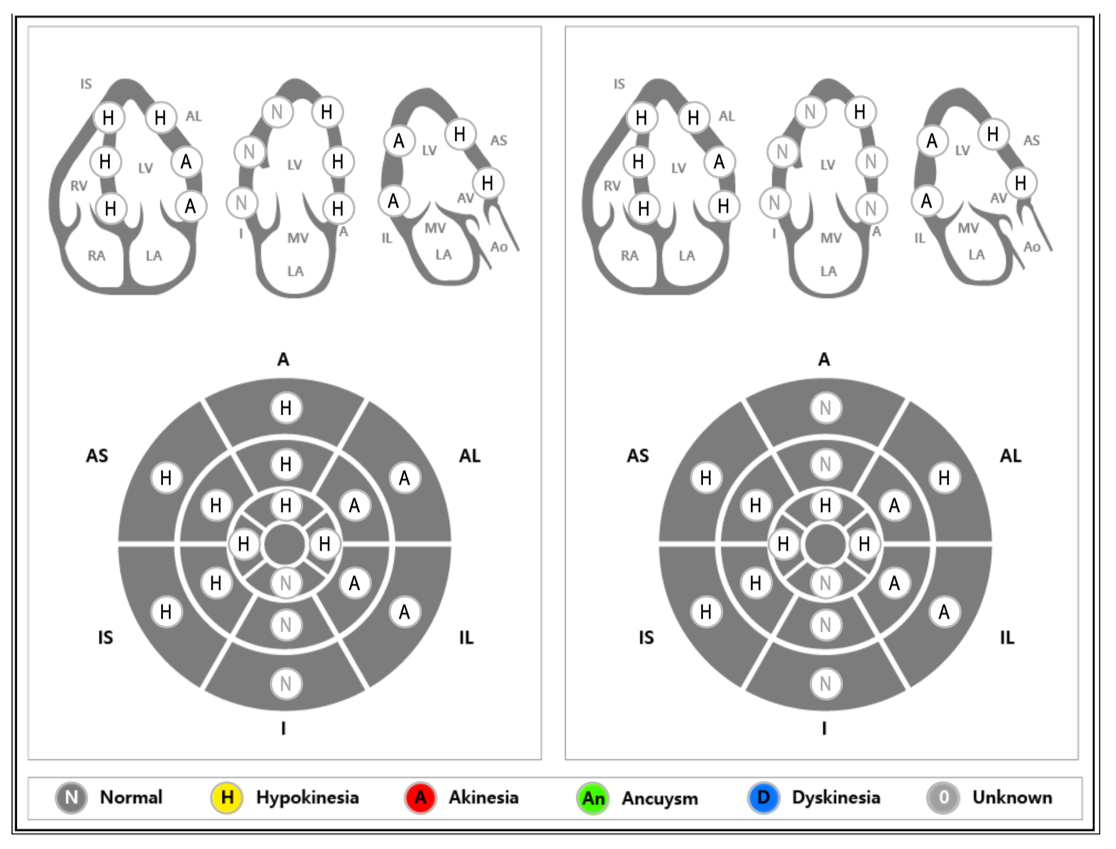
ECG showed inferior Q waves with inverted T waves at anterolateral and inferior. Echo revealed EF 37% with preserve RV function, abnormal LV diastolic function (grade I) with normal LA pressure, akinetic wall motion at basal to mid anterolateral and inferolateral, hypokinetic at basal to mid anterior, anteroseptal and inferoseptal. Dobutamine Stress Echo (DSE) was performed and there was biphasic phenomenon at basal to mid anterior segment, confirming viability of LAD teritory.

 Echo2.mp4
Echo2.mp4

Relevant Catheterization Findings
PCI was performed from femoral access due to planned rotational atherectomy (RA). Angiography revealed right common iliac tortuosity, and coronary angiography showed normal LM, heavy calcification with 80-90% stenosis at LAD mid part, and 90% stenosis at LCx right before OM1 branch.
 iliac.mp4
iliac.mp4
 LAD.mp4
LAD.mp4
 LCx.mp4
LCx.mp4
Interventional Management
Procedural Step
We did femoral access PCI but encountered difficulty when canulating LCA, so we changed into long femoral sheath (7F, 25 cm) but still didn't pass through the tortuossegment, so we changed to longer femoral sheath (7F, 60 cm). We performed rotational atherectomy with 1.75 burr size followed by predilation with NC scoring balloon2.5x20 mm (20 atm) at proximal to mid LAD. Stenting was done with DES 3.5x24 mm at mid part dan DES 3.5x28 mm at proximal part with good result. Patient was hemodinamically stable during procedure with no significant symptom. During observation at the recovery room, patient complained abdominal discomfort, looked pale and diaphoretic. Blood pressure dropped to 70/50 mmHg, fluid resuscitation was done with additional vasopressor. Echo was performed but with unremarkable result. Abdominal USG showed free fluid at perivesica and hepatorenal recess indicating retroperitoneal haemorrhage. Patient was sent to cathlab immediately to performed angiography and revealed there was perforation at right common iliac artery. Balloon tamponade was done with Mustang balloon 6.0x60 mm at proximal tear, followed by implantation of S&G Biotech INC bifurcated stent graft 10x40 mm. Angiography evaluation showed good result without residual perforation. Haemoglobin dropped to 9.4 from 13, PRC tranfusion was given. Patient continuously improved and get discharged after 5 days.
 perforation.mp4
perforation.mp4
 stent graft.mp4
stent graft.mp4
 final result.mp4
final result.mp4
Case Summary
Retroperitoneal haemorrhage is rare yet disastrous complication that need prompt treatment to prevent further deterioration. In dealing with tortuosity, we need additional tools (e.g long sheath, stiff guidewire or even vascular cover stent or surgical backup in case of complication) to avoid complication.


