Lots of interesting abstracts and cases were submitted for TCTAP 2022. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-107
Retrieval of a Broken Rotawire on the Aortic Cusp Using Combined Twisting Wire Technique, Microsnare and Patient’s Cough
By Sakolwat Montrivade, Anuruck Jeamanukoolkit
Presenter
Sakolwat Montrivade
Authors
Sakolwat Montrivade1, Anuruck Jeamanukoolkit1
Affiliation
Police General Hospital, Thailand1,
View Study Report
TCTAP C-107
CORONARY - Complications
Retrieval of a Broken Rotawire on the Aortic Cusp Using Combined Twisting Wire Technique, Microsnare and Patient’s Cough
Sakolwat Montrivade1, Anuruck Jeamanukoolkit1
Police General Hospital, Thailand1,
Clinical Information
Patient initials or Identifier Number
JN
Relevant Clinical History and Physical Exam
A 75-year-old man with type 2 diabetes, hypertension, dyslipidemia and chronic kidney disease on regular hemodialysis presented with intradialytic hypotension with chest discomfort and exertional dyspnea in the past month. His blood pressure was 110/58 mmHg and HR of 85/min. Chest was clear on auscultation and cardiovascular exam showed normal S1S2 with soft systolic murmur at the left parasternal border.
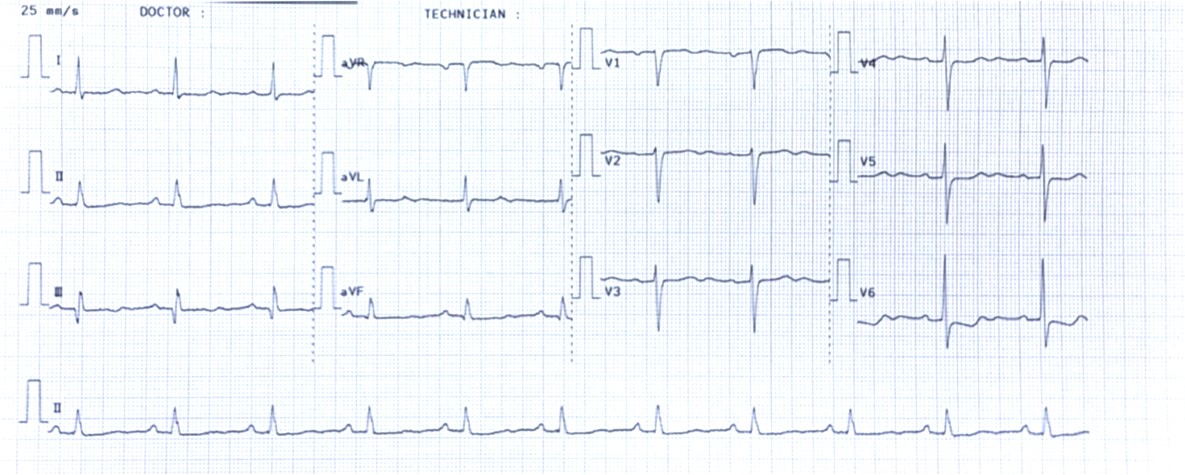

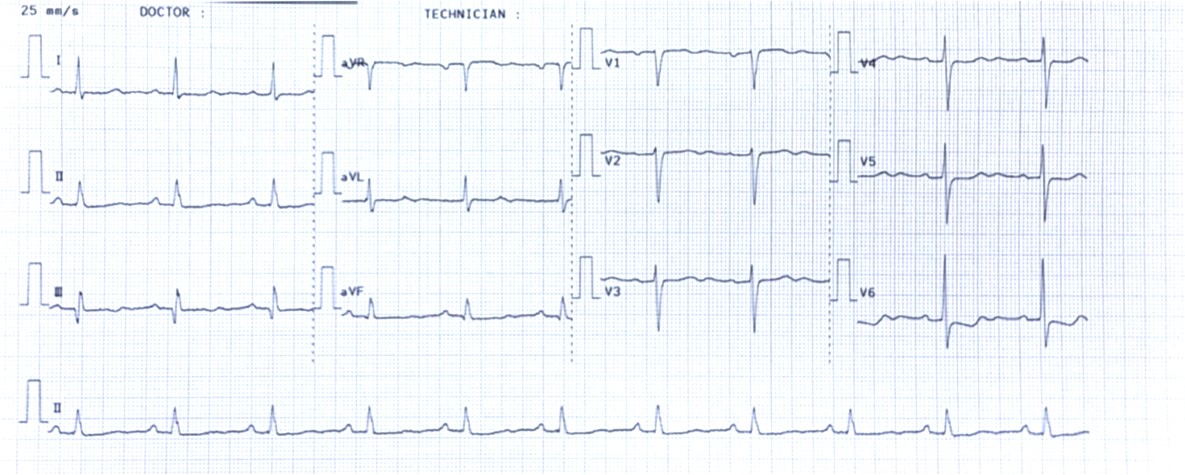

Relevant Test Results Prior to Catheterization
EKG revealed sinus rhythm with ST depression in V4-6 leads and echocardiography showed concentric LV hypertrophy with normal LVEF of 55%, no regional wall motion abnormalities, mild MR and mild TR.
Relevant Catheterization Findings
Patient was brought for diagnostic CAG which revealed three-vessel disease.LM: No significant stenosis.
LAD: Heavily calcified proximal to mid LAD with 80% stenosis proximal and mid LAD.
LCx: 70% stenosis proximal LCx.
RCA: 100% CTO ostial RCA receiving collateral from LAD. Heavily calcified, very long and highly tortuous CTO segment.Patient refused CABG. Attempting PCI CTO RCA was failed and eventually deemed not possible for PCI.
PCI LAD with rotational atherectomy for symptom relief was planned.
 PrePCI LAD AP cranial.wmv
PrePCI LAD AP cranial.wmv
 PrePCI RCA LAO.wmv
PrePCI RCA LAO.wmv
 PrePCI Spider.wmv
PrePCI Spider.wmv
LAD: Heavily calcified proximal to mid LAD with 80% stenosis proximal and mid LAD.
LCx: 70% stenosis proximal LCx.
RCA: 100% CTO ostial RCA receiving collateral from LAD. Heavily calcified, very long and highly tortuous CTO segment.Patient refused CABG. Attempting PCI CTO RCA was failed and eventually deemed not possible for PCI.
PCI LAD with rotational atherectomy for symptom relief was planned.
Interventional Management
Procedural Step
Right femoral access was obtained using 6Fr sheath. LCA was engaged with XB3.5, 6Fr catheter and the LAD lesions were crossed with Sion Blue wire in FineCross microcatheter then exchanged to Rotawire Floppy. Rotational atherectomy was performed using Rota Burr 1.5 mm, 180,000 rpm for 5 rounds. Rota Burr was removed using dynaglide mode. There was an unintentional wire prolapse while activating dynaglide mode and subsequently caused wire fracture and dislodgement to distal LAD. Further balloon pre-dilation and stenting of the proximal and mid LAD were done first using EES 3.5 x 18 mm and EES 2.75 x 28 mm with good result. With twisting wire technique using Runthrough NS and Sion Blue wire, the broken Rotawire was moved from distal LAD to LM carina, however, subsequent attempts could not grasp the broken Rotawire due to too large luminal space. Snaring with a 7 mm microsnare was failed and also pulled out the broken Rotawire onto the left coronary cusp of aortic valve. The patient was instructed to cough for multiple times and the wire was bounced back into LM carina. Again using the 7 mm microsnare, the broken Rotawire was successfully removed. Final angiography showed good PCI result without serious complication.
 Rotawire fracture during dynaglide.wmv
Rotawire fracture during dynaglide.wmv
 Microsnare success.wmv
Microsnare success.wmv
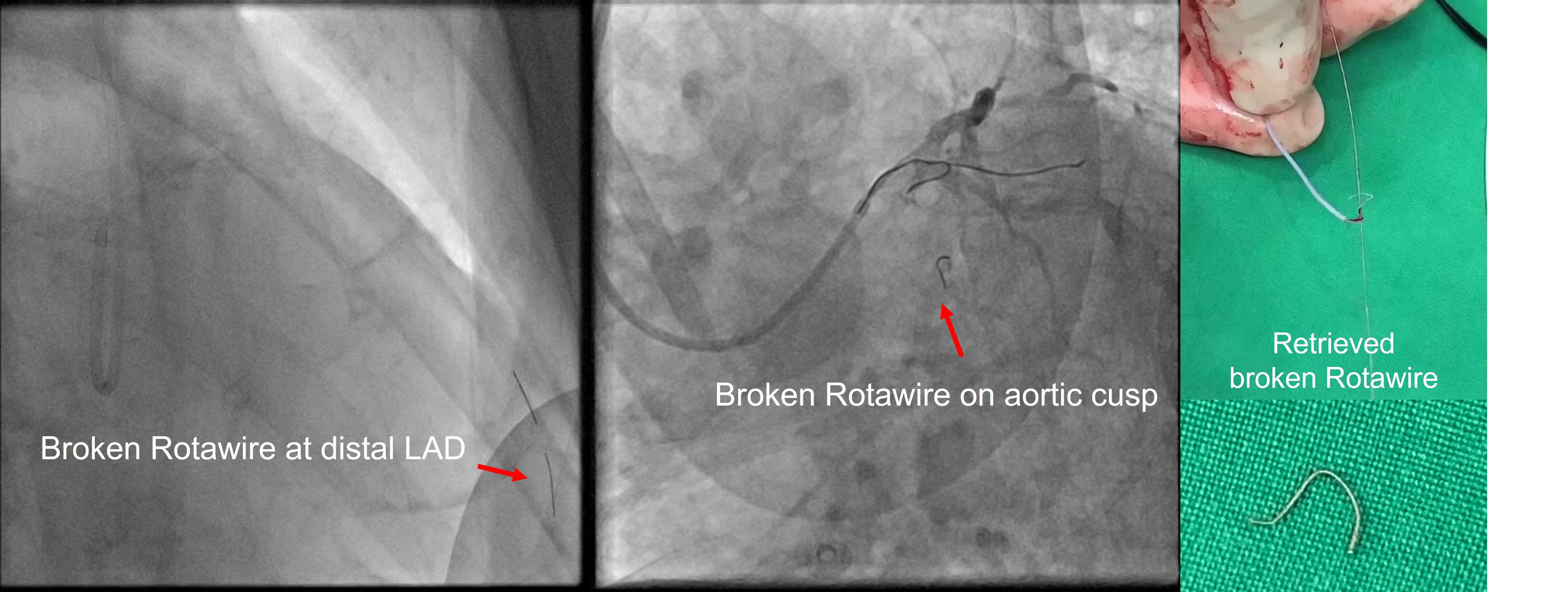
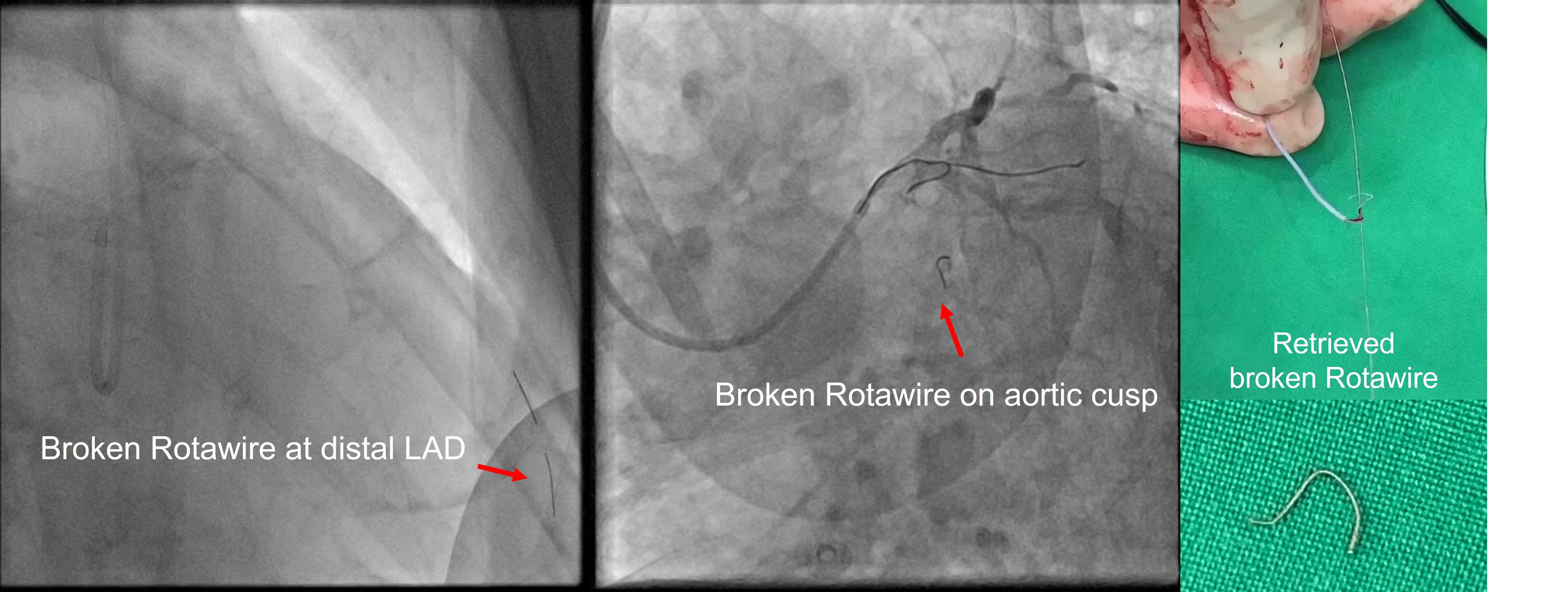
Case Summary
Learning points from our case are as follows:1. Removal of Rota Burr using dynaglide mode needs careful cooperation between the first and second operators not to accidentally prolapse the wire while activating dynaglide mode which will cause wire fracture from rotation of the looped wire.2. Twisting wire technique is easier to retrieve the broken wire fragment from narrow spaces such as distal LAD than large spaces such as left main carina where snaring with microsnare kit is more appropriate.3. If the broken wire fragment is on the aortic cusp, instructing the patient to cough may bring the wire back into LCA. However, the risk of wire embolization to peripheral arteries is unpredictable.


