Lots of interesting abstracts and cases were submitted for TCTAP 2022. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-039
Double Trouble: Complex Left Main Bifurcation With Ostial LAD Chronic Total Occlusion (CTO)
By Azrina Abdul Kadir, Yu Ying Ong, Heng Shee Kim, Vicknesan Kulasingham, Doreen Sumpat, Hou Tee Lu
Presenter
Azrina Abdul Kadir
Authors
Azrina Abdul Kadir1, Yu Ying Ong2, Heng Shee Kim3, Vicknesan Kulasingham4, Doreen Sumpat5, Hou Tee Lu3
Affiliation
KPJ Bandar Dato Onn Specialist Hospital, Malaysia1, Sultan Idris Shah Serdang Hospital, Malaysia2, Sultanah Aminah Hospital, Malaysia3, Ministry of Health Malaysia, Malaysia4, Universiti Malaysia Sabah, Malaysia5,
View Study Report
TCTAP C-039
CORONARY - Bifurcation/Left Main Diseases and Intervention
Double Trouble: Complex Left Main Bifurcation With Ostial LAD Chronic Total Occlusion (CTO)
Azrina Abdul Kadir1, Yu Ying Ong2, Heng Shee Kim3, Vicknesan Kulasingham4, Doreen Sumpat5, Hou Tee Lu3
KPJ Bandar Dato Onn Specialist Hospital, Malaysia1, Sultan Idris Shah Serdang Hospital, Malaysia2, Sultanah Aminah Hospital, Malaysia3, Ministry of Health Malaysia, Malaysia4, Universiti Malaysia Sabah, Malaysia5,
Clinical Information
Patient initials or Identifier Number
Mrs S
Relevant Clinical History and Physical Exam
We described a 65-year old lady, who has underlying type 2 diabetes mellitus, hypertension, chronic kidney disease (CKD) and ischaemic heart disease with two previous admissions for non-ST elevation myocardial infarction(NSTEMI) and Unstable angina in other hospital. Unfortunately, she was admitted again with Unstable angina to our centre.
Relevant Test Results Prior to Catheterization
Her ECG showed widespread ST depressions with ST elevation in AVR. She has preserved left ventricular ejection fraction (LVEF) of 60-65% with no regional motion abnormalities. Her Creatinine was 138 umol/l (eGFR 47ml/min).
Relevant Catheterization Findings
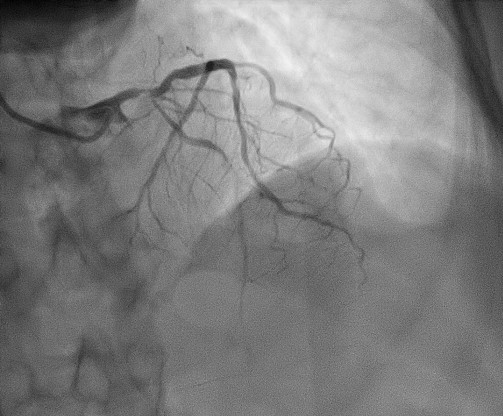
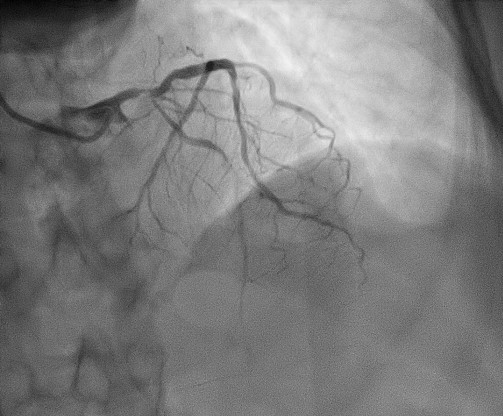
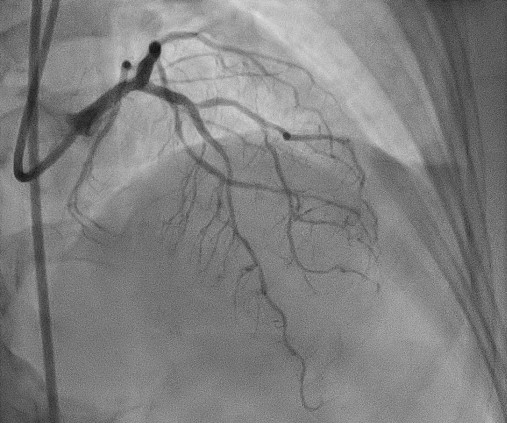
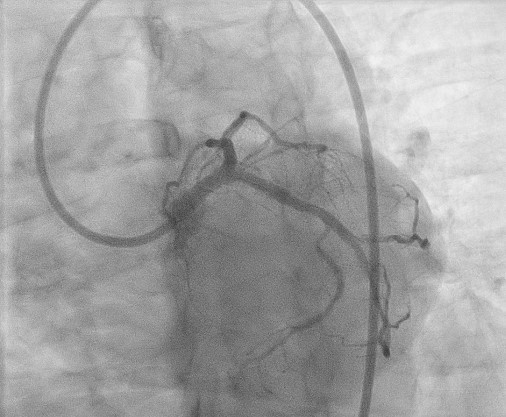
Coronary angiogram showed two vessel disease with bifurcation left main (LM) disease 70% stenosis, ostial LAD chronic total occlusion (CTO), Ostial LCX 80% stenosis(medina 1,1,1), diffuse proximal to mid LAD 80-90% stenosis, proximal RCA 20% stenosis, with collaterals to LAD seen from the RCA. She was referred to Cardiothoracic team for coronary artery bypass graft (CABG) but deemed unsuitable due to poor target vessels.
 MOVIE-0003.wmv
MOVIE-0003.wmv
Interventional Management
Procedural Step
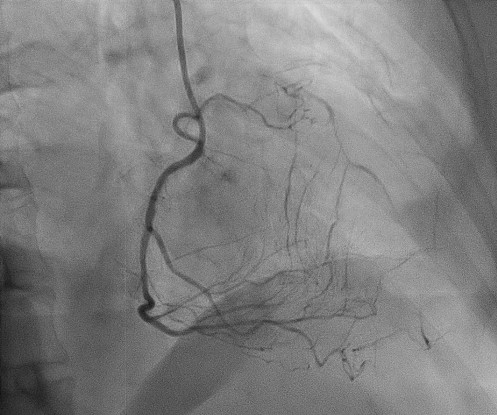
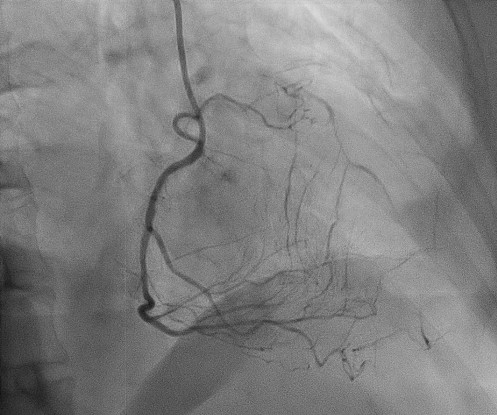
PCI was performed via bilateral femoral approach with 7Fr right femoral artery and 6Fr left femoral artery as contralateral injection. 7Fr EBU 3.0 was engaged to the left system and 6Fr JR4 to the right system. Total of 10,000U intracoronary Heparin and Clopidogrel 300mg given. Attempted to wire ostial LAD with Runthrough floppy but failed and wired to distal LCX instead. Then used Sion wire through microcatheter(MC) Turnpike LP but still unsuccessful and changed to MC Crusade and wired to ramus intermedia with Sion blue but unable to wire to LAD with Fielder XT-R. We then predilated ostial LCX to distal LM with NC 2.0 x 8mm. Then used MC Finecross with CROSS-IT 100 XT wire but still unable to cross and eventually used Gaia Second and successfully managed to cross the lesion. We predilated mid LAD(MLAD) with NC 2.0 x 8 mm and proximal LAD(PLAD) to LM with NC 2.75 x 12 mm. Stented MLAD to PLAD with DES Promus Premier 2.25 x 24 mm and proximal LCX to LM with DES Promus Premier 3.5 x 20 mm. Postdilated MLAD stent with NC 2.0 x 8 mm. Stented PLAD to ostial LM with DES Xience Xpedition 4.0 x 15mm. First kissing balloon inflations(KBI) performed with NC 3.75 x 12 mm in LAD and and NC 3.5 x 12 mm in LCX. POT with NC 4.0 x 8 mm in LM. Rewired to LCX with difficulty with Fielder XT-R and second KBI done with similar previous balloon profiles (Mini-crush technique). Re-POT LM with NC 4.0 x 8 mm. IVUS performed pre and post-procedure. Final result was good, no dissection and TIMI 3 flow.
 LAD TRUE LUMEN.wmv
LAD TRUE LUMEN.wmv
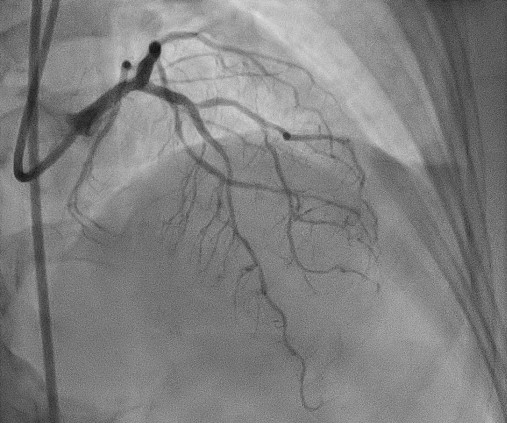
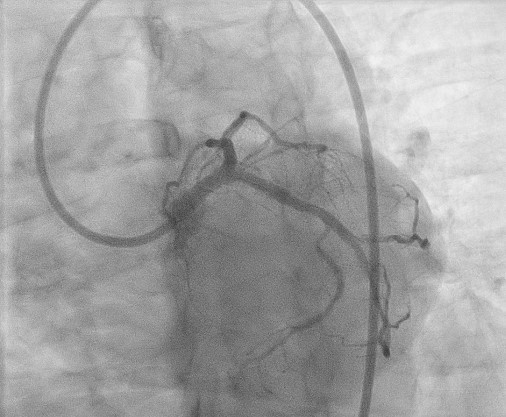
Case Summary
Upfront two-stent strategy of left main bifurcation disease is the preferred strategy for a more complex left main anatomy, especially with DK crush technique due to better long-term outcome as illustrated in DKCRUSH-V study. Unfortunately, we have to modify our strategy to Mini crush technique due to difficult wiring to side branch for the sake of patient's safety due to already high amount of contrast and long procedure time. IVUS guidance in left main PCI is well established and plays an important role in improving long term outcome. CTO did complicate this already complex LM bifurcation PCI and contributed to long procedure and high contrast volume.


