Lots of interesting abstracts and cases were submitted for TCTAP 2022. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-011
ST-Elevation STEMI With High Thrombus Burden
By Vicknesan Kulasingham, Gurudevan Mahadevan, Tee Choon Keong, Heng Shee Kim, Adelyn Nisha Henry, Kumutha Gobal, Azrina Abdul Kadir, Kim Fong Ng
Presenter
Vicknesan Kulasingham
Authors
Vicknesan Kulasingham1, Gurudevan Mahadevan2, Tee Choon Keong2, Heng Shee Kim2, Adelyn Nisha Henry2, Kumutha Gobal2, Azrina Abdul Kadir3, Kim Fong Ng2
Affiliation
Ministry of Health Malaysia, Malaysia1, Sultanah Aminah Hospital, Malaysia2, KPJ Bandar Dato Onn Specialist Hospital, Malaysia3,
View Study Report
TCTAP C-011
CORONARY - Acute Coronary Syndromes (STEMI, NSTE-ACS)
ST-Elevation STEMI With High Thrombus Burden
Vicknesan Kulasingham1, Gurudevan Mahadevan2, Tee Choon Keong2, Heng Shee Kim2, Adelyn Nisha Henry2, Kumutha Gobal2, Azrina Abdul Kadir3, Kim Fong Ng2
Ministry of Health Malaysia, Malaysia1, Sultanah Aminah Hospital, Malaysia2, KPJ Bandar Dato Onn Specialist Hospital, Malaysia3,
Clinical Information
Patient initials or Identifier Number
Mr TKS
Relevant Clinical History and Physical Exam
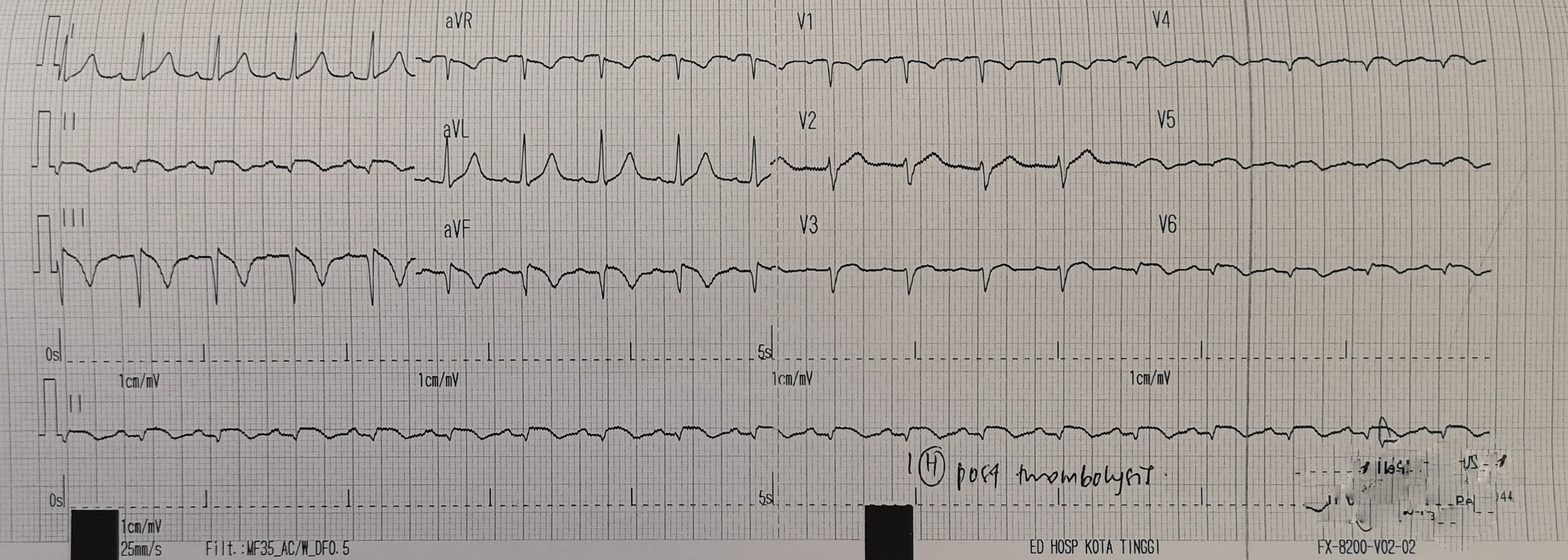
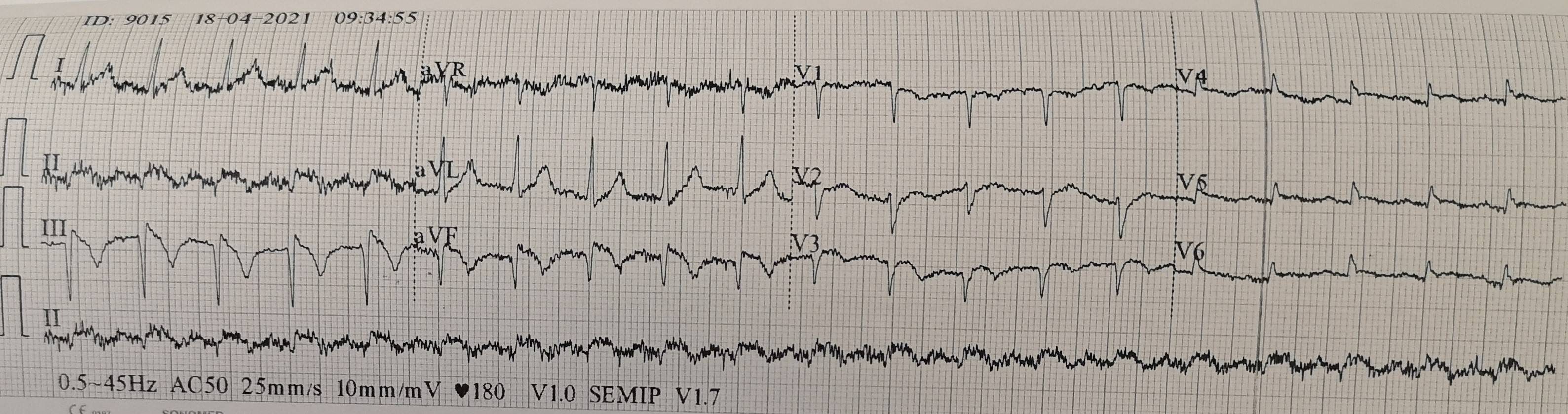
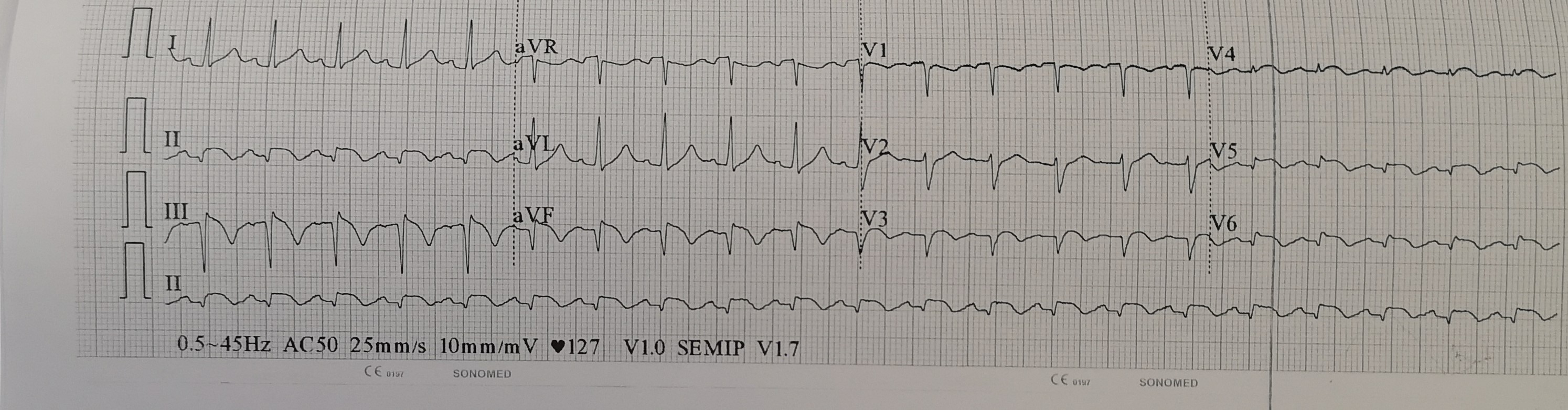
40-year-old gentleman with hypertension and who is a non-smoker presented to a district hospital with typical left sided chest pain for 2 days. There was no failure or infective symptoms. Upon arrival to hospital, patient is alert and conscious. Hemodynamically stable. There were no clinical signs of heart failure. ECG at district hospital showed ST elevation over inferior-lateral leads and he was given thrombolysis. There was no resolution post-thrombolysis and he was referred to us for rescue PCI.
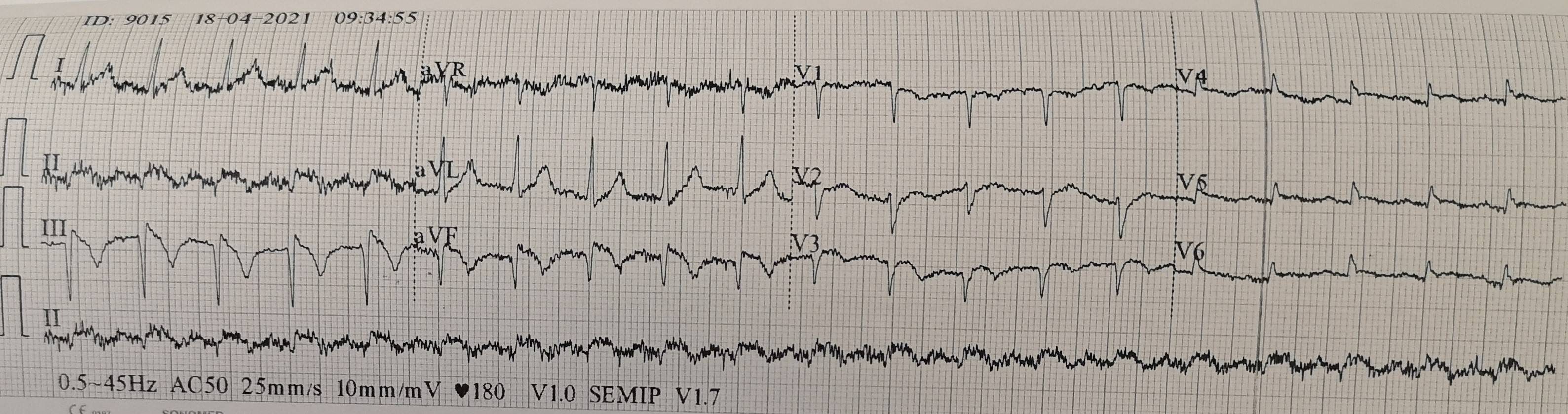
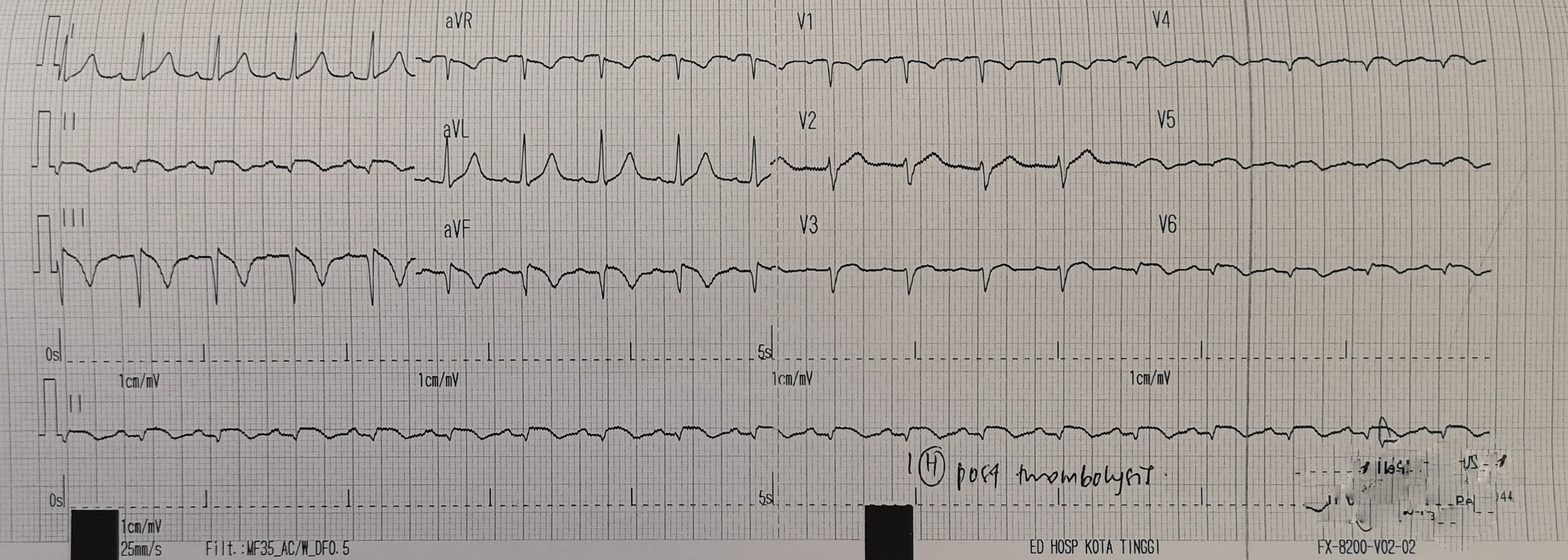
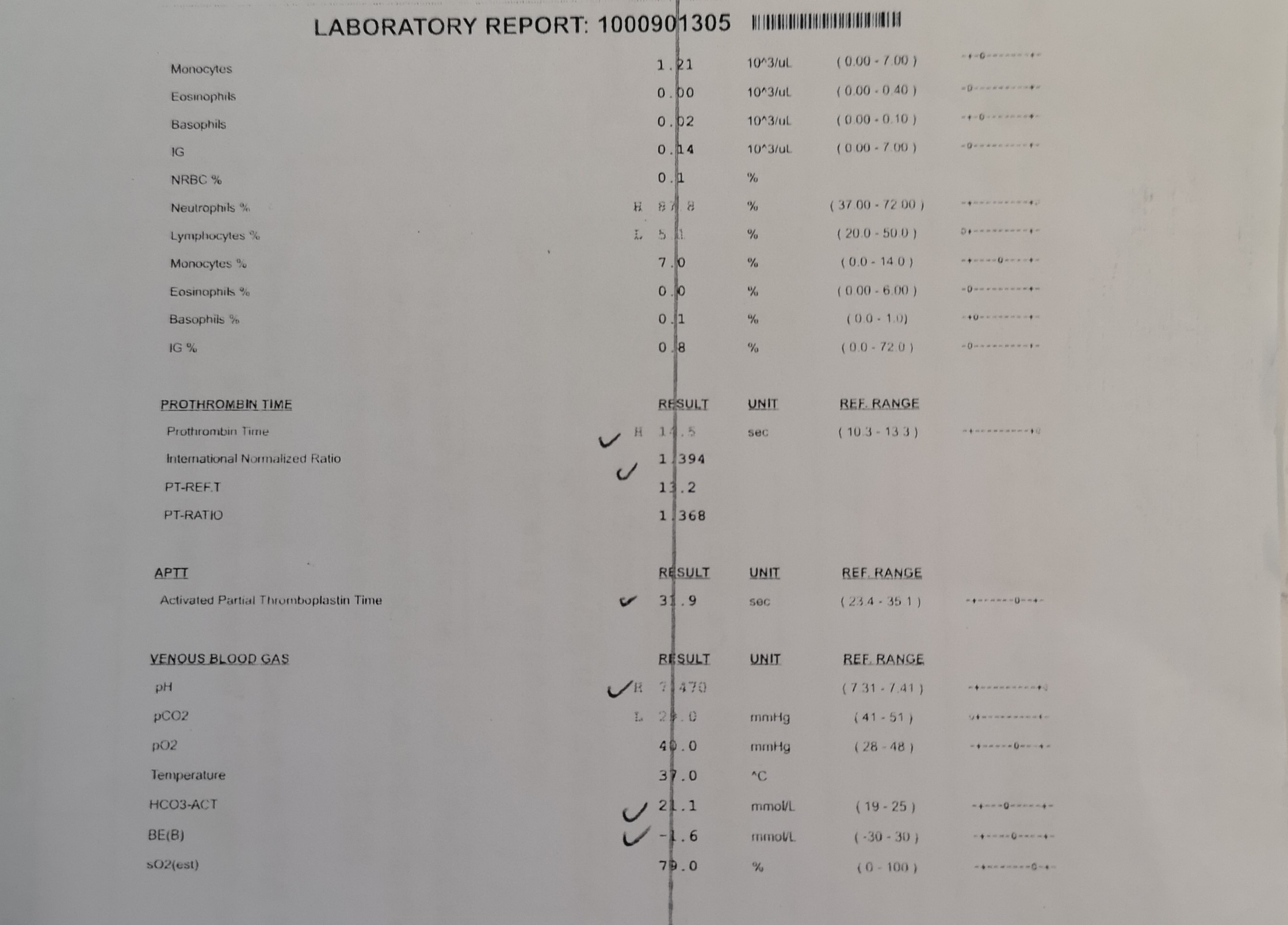
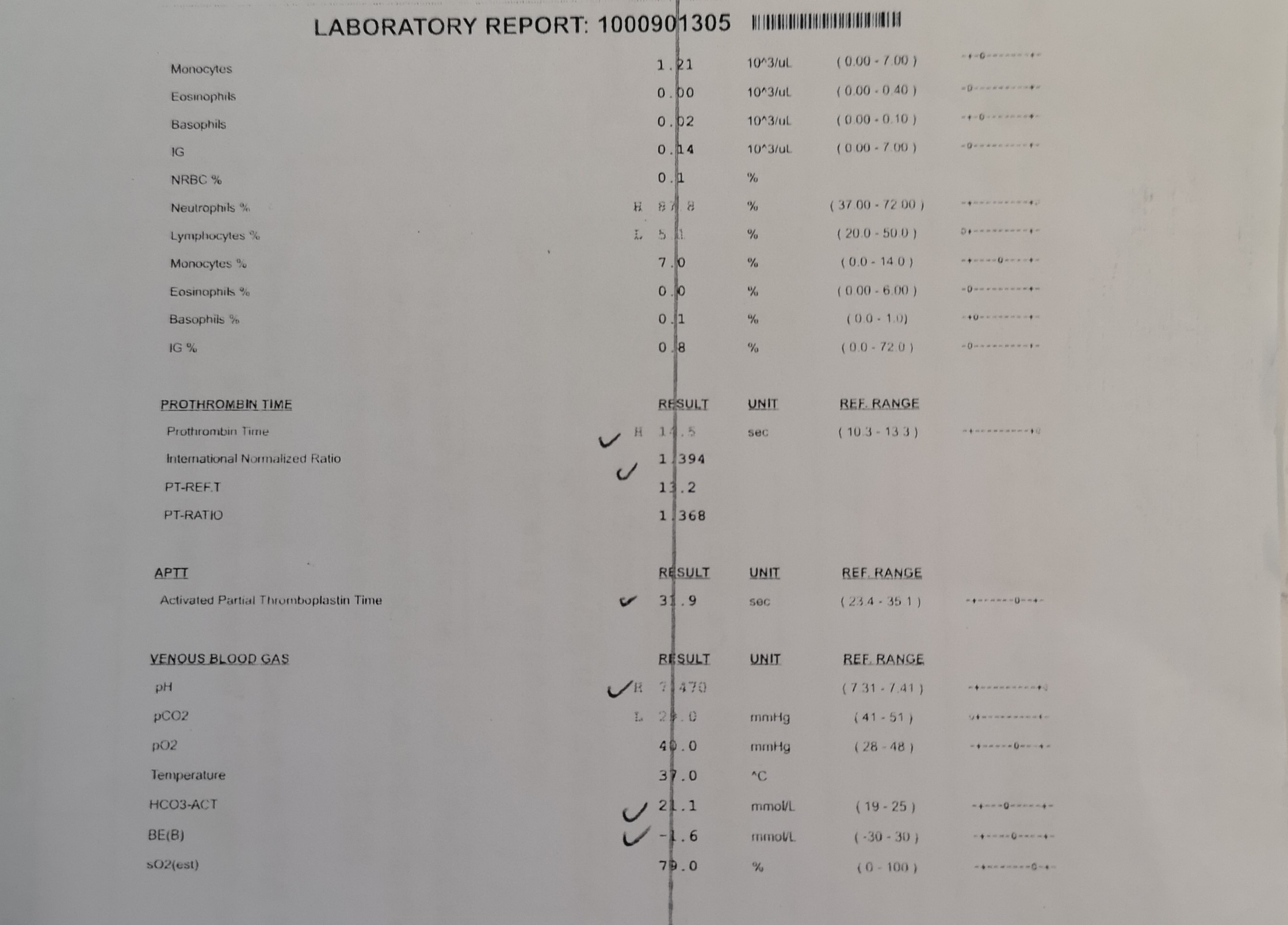
Relevant Test Results Prior to Catheterization
Hb 15.9 g/dl, wbc 17x10^3/uL, CK 2870U/L, Troponin T 5360 ng/dl, urea 3.9 mmol/L, creatinine 148 micromol/LEchocardiography: LVEF 40-45%, basal to apical inferoseptal hypokinesiaCXR: clear lung fields


Relevant Catheterization Findings
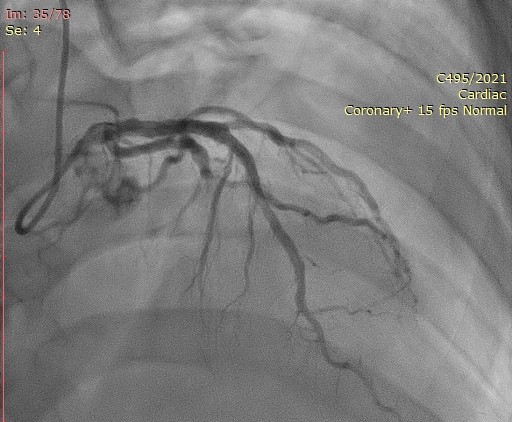
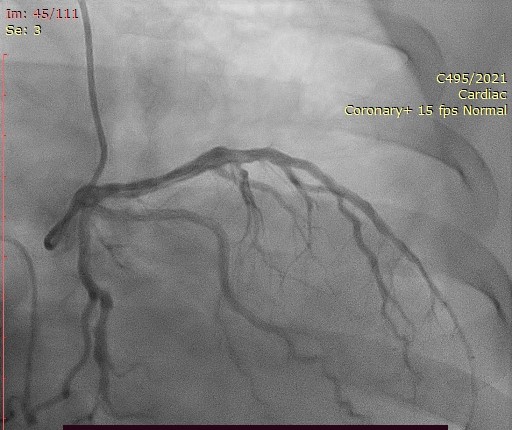
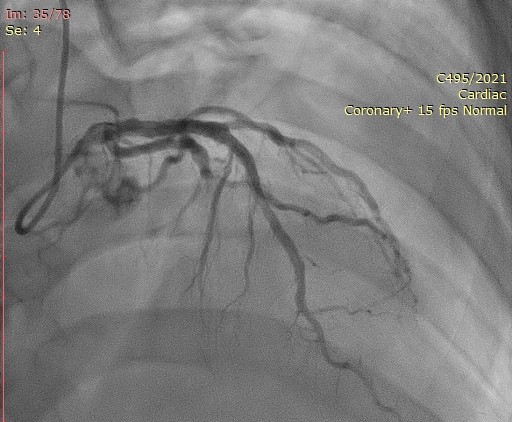
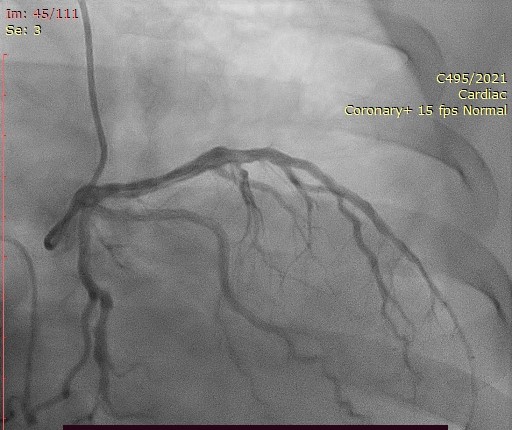
Acute total occlusion proximal RCA. Proximal LAD 30-40%, D1 30%. Left circumflex artery was normal.
Interventional Management
Procedural Step
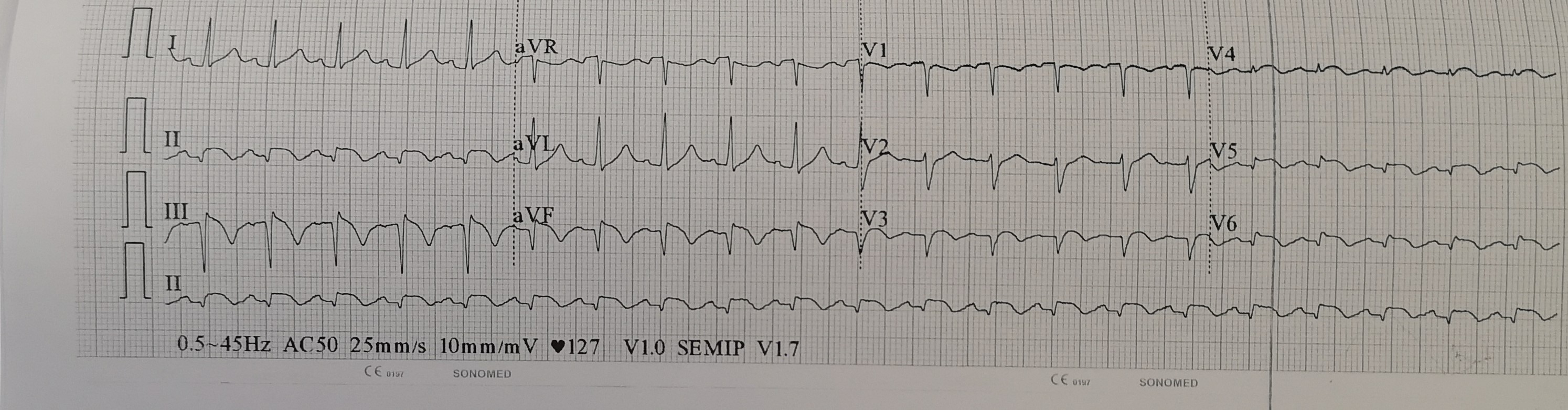
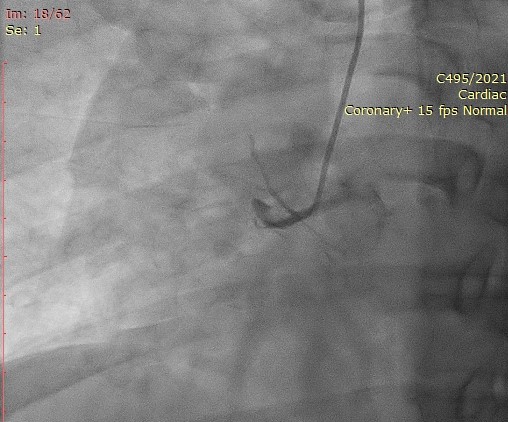
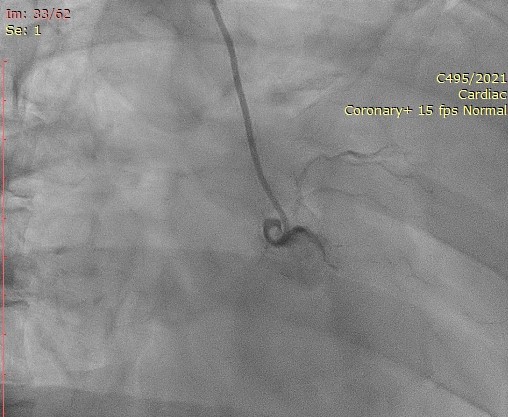
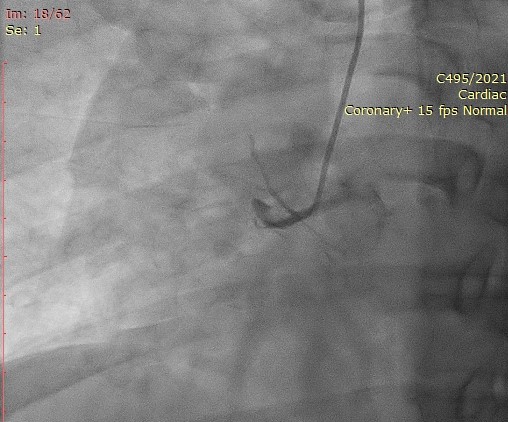
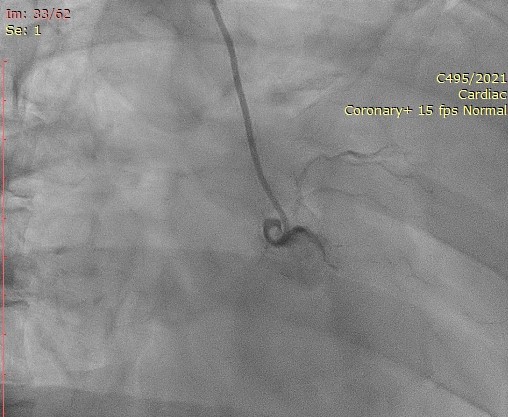
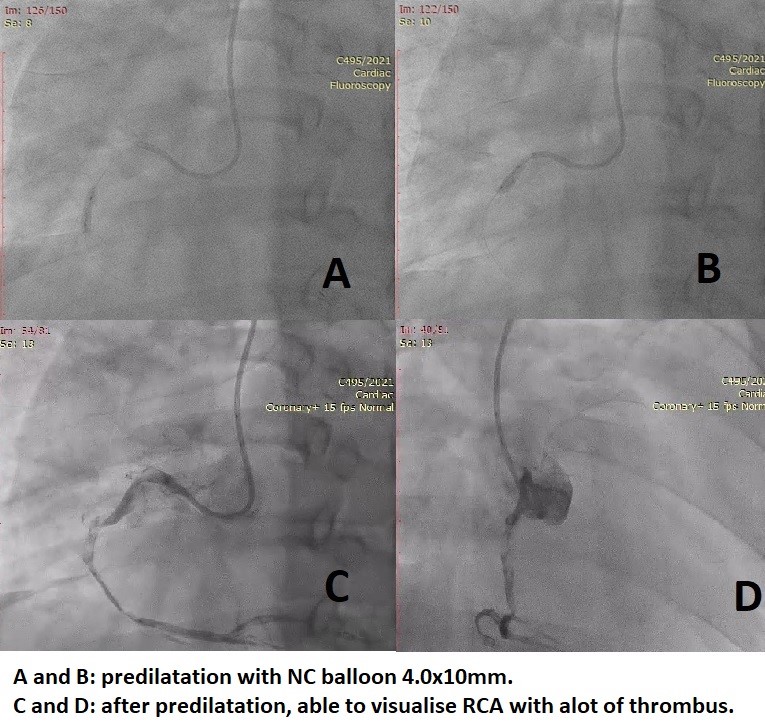
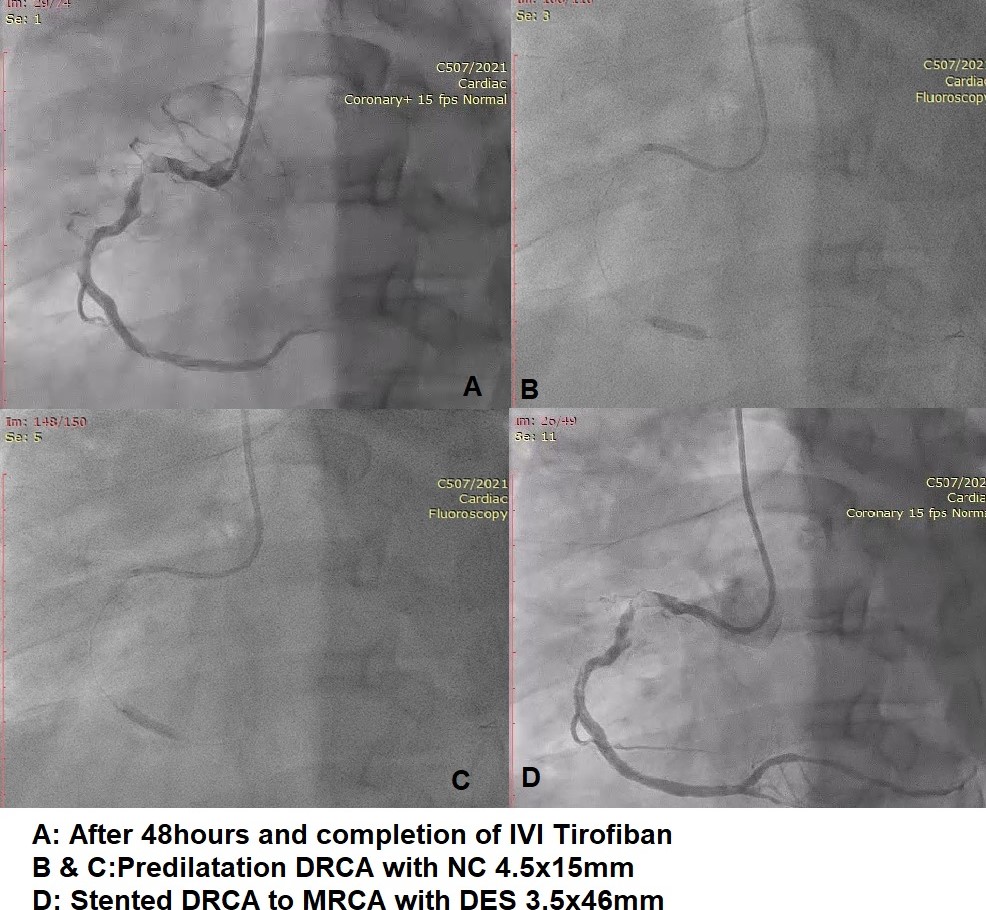
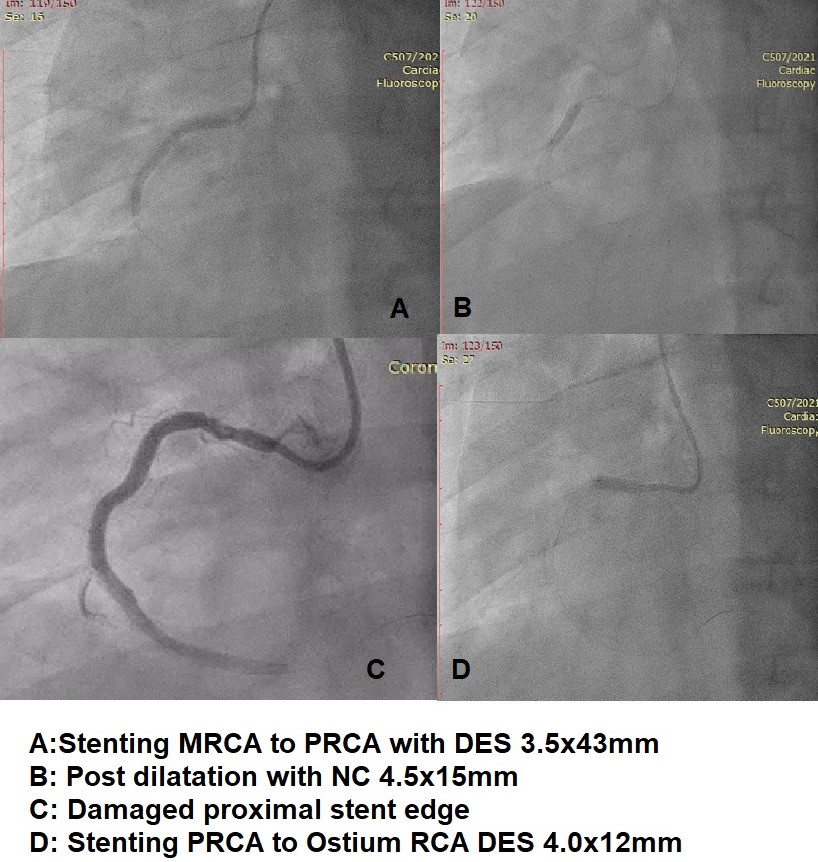
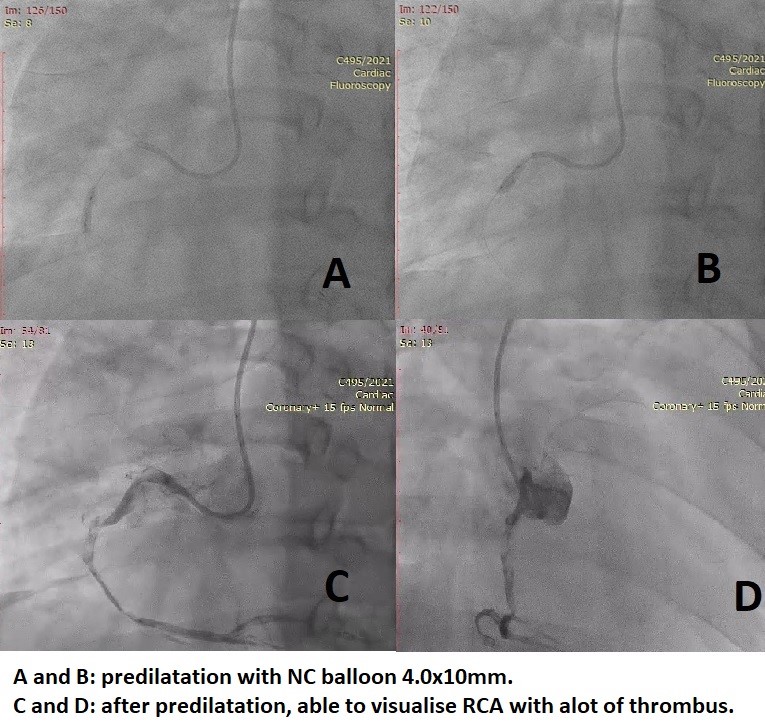
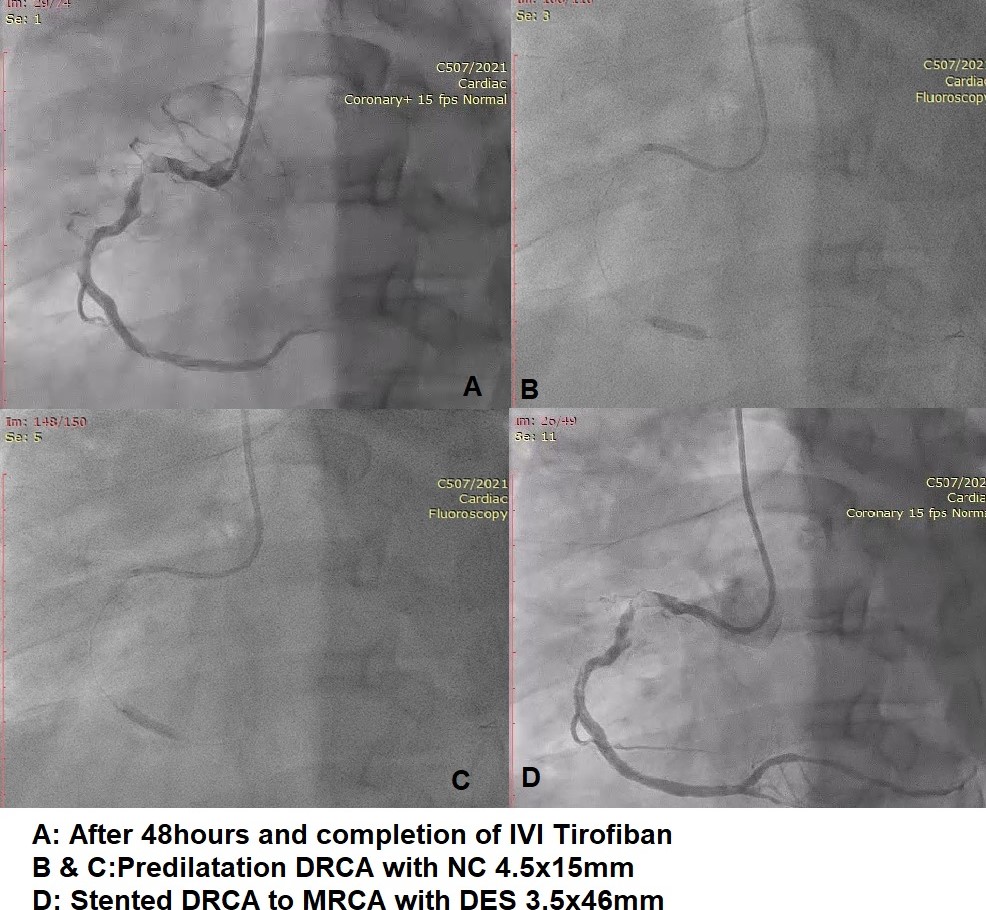
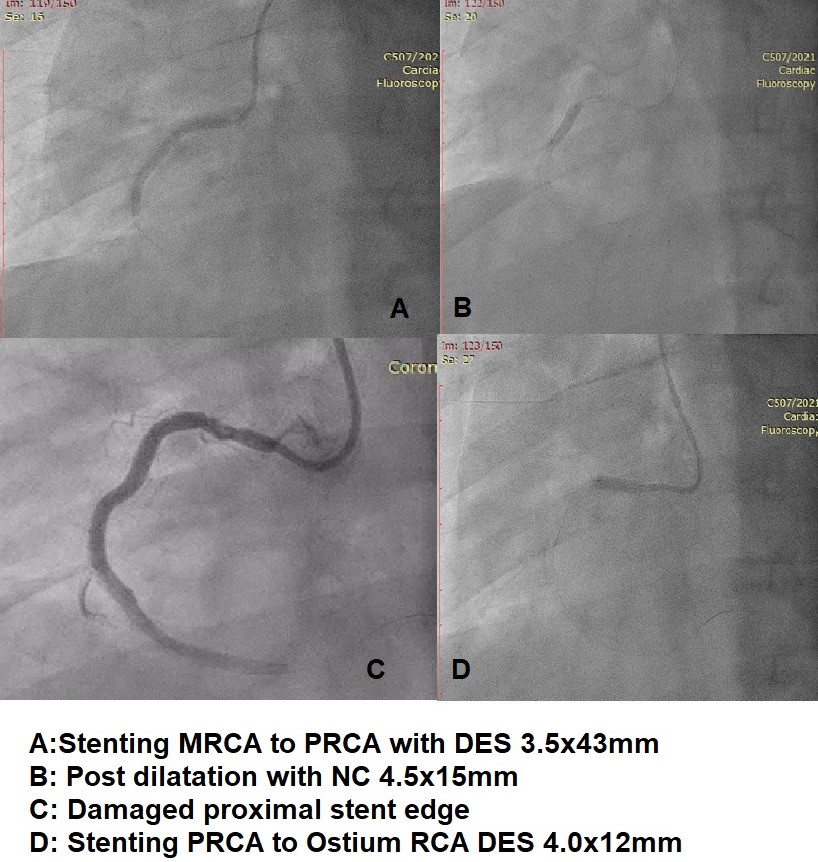
Right radial approach with 6Fr AL0.75 guiding catheter and wired down into PDA with PT2 moderate support wire. After wiring down, managed to see some minimal flow to delineate the RCA. Predilated MRCA to PRCA with NC Rise 4.0x10 mm. Able to visualize RCA better and had thrombus from PRCA to MRCA. Thrombus aspiration done with Thrombuster x3 and able to aspirate multiple red and white clots. Despite aspiration there was still thrombus, IC tirofiban was given slow bolus. Post-tirofiban there were new thrombus formation but with TIMI 3 flow and no dissection. Patient had no chest pain and hemodynamically stable. Decided to continue with tirofiban infusion and re-angio after 48 hours. Angio after 48 hours showed lesser clot. Engaged initially with 6Fr JR4 but due to poor support, changed to AL0.75. Wired down with BMW wire and predilated DRCA to PRCA with NC EUPHORA 4.5x15 mm. Stented DRCA to MRCA with CRE8 EVO 3.5x46 mm. Stented PRCA to MRCA with EUCALIMUS 3.5x43mm and post dilated with NC EUPHORA 4.5x15 mm. Proximal stent edge damaged due to catheter tip injury with slow flow. Stented PRCA to ostium with PROMUS PREMIER 4.0x12 mm and post dilated with the same NC EUPHORA 4.5x15 mm.TIMI 3 flow and no dissection.

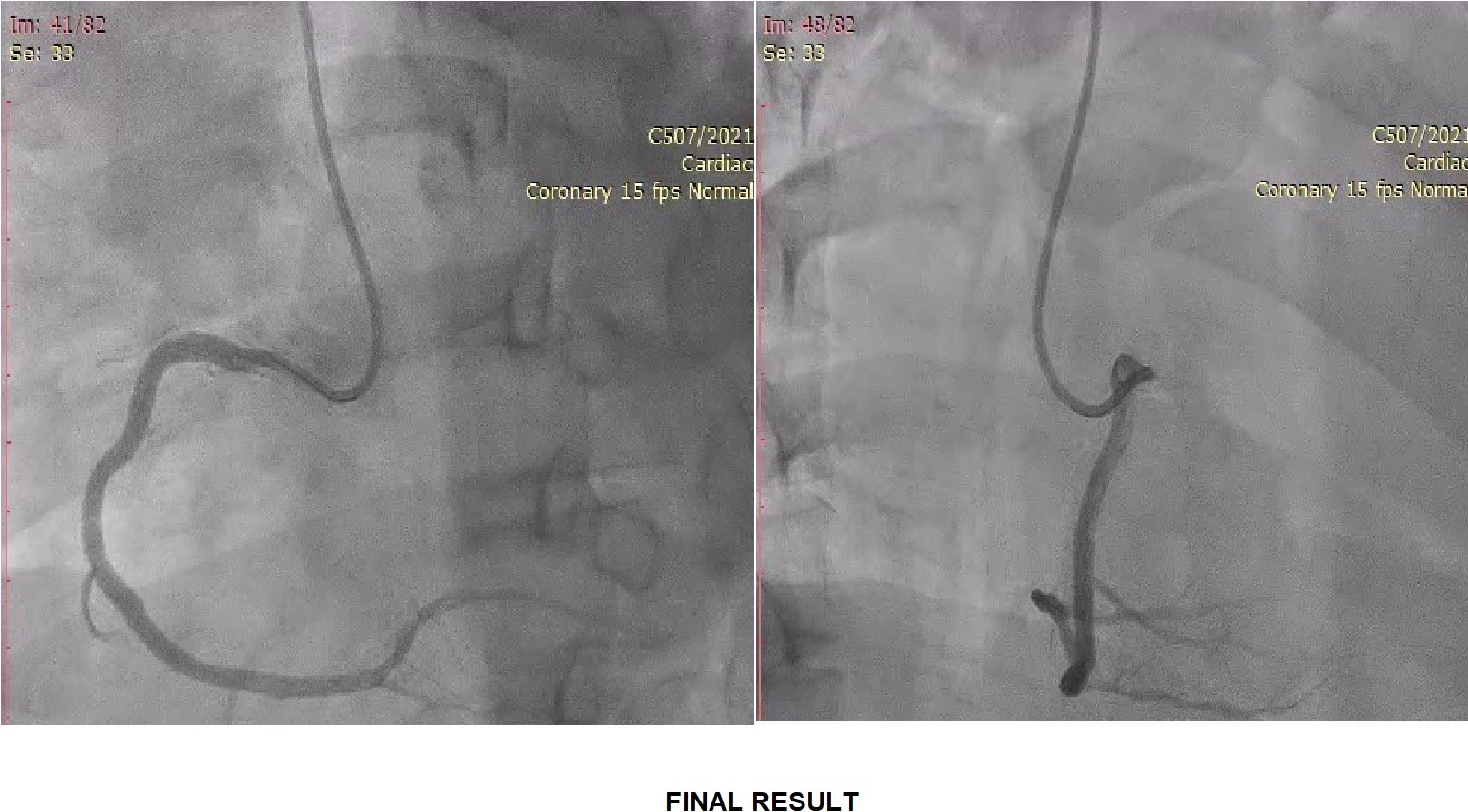

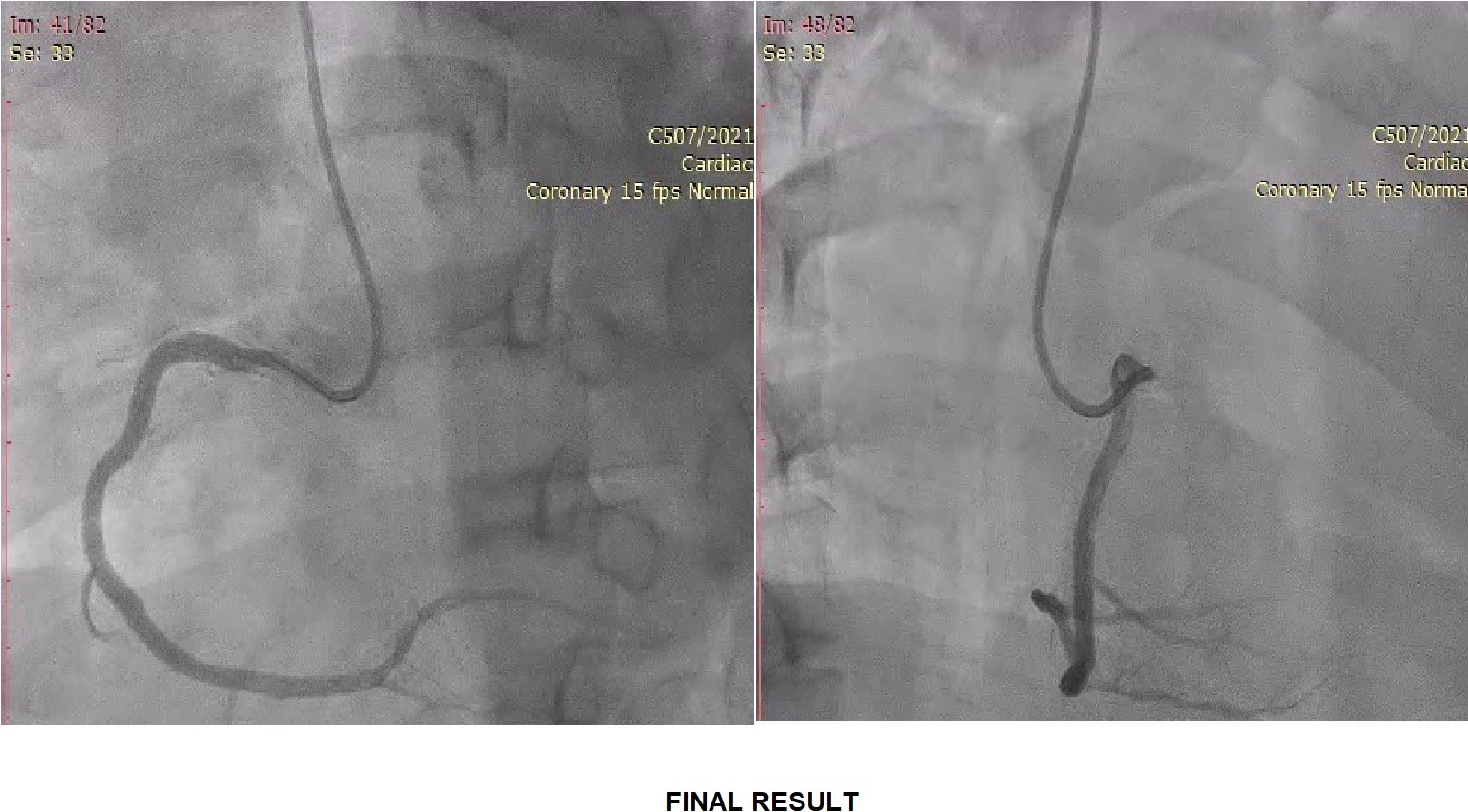
Case Summary
PCI in acute setting as in STEMI there could be high thrombus load in IRA. Stenting in such scenarios would cause the thrombus to migrate proximally or distally leading to slow-flow/no-flow phenomenon, which in turn leads to high mortality. Deferred stenting is preferred strategy in high thrombus burden IRA. By deferring stenting along with parenteral anticoagulant, it allows gradual resorption of thrombus, improvement in TIMI flow to distal vessels and lesser incidence of slow-flow/no-flow phenomenon. The ideal time for deferment is still debatable, ranging from 48-72 hours up till 7 days. Longer deferral time gives more time for thrombus resorption, but it is not practical with longer hospitalization.


