Lots of interesting abstracts and cases were submitted for TCTAP 2022. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-163
Do We Need an Alternate Morphologic Classification of Patent Ductus Arteriosus Based on Percutaneous Device Closure Approach?
By Shishir Soni, Bhanu Duggal
Presenter
Shishir Soni
Authors
Shishir Soni1, Bhanu Duggal2
Affiliation
SSH, NSCB Medical College, India1, AIIMS Rishikesh, India2,
View Study Report
TCTAP C-163
STRUCTURAL HEART DISEASE - Congenital Heart Disease (ASD, PDA, PFO, VSD)
Do We Need an Alternate Morphologic Classification of Patent Ductus Arteriosus Based on Percutaneous Device Closure Approach?
Shishir Soni1, Bhanu Duggal2
SSH, NSCB Medical College, India1, AIIMS Rishikesh, India2,
Clinical Information
Patient initials or Identifier Number
20210027018
Relevant Clinical History and Physical Exam
A 14-year-old female, was referred to the tertiary care Centre for the evaluation of the murmur and echocardiography. On physical examination she was found to have a continuous murmur in the second left intercostal space.
Relevant Test Results Prior to Catheterization
Echocardiography revealed 4mm patent ductus arteriosus (PDA) with left to right shunt. Therefore, the patient was planned for the Cath study followed by PDA closure.
Relevant Catheterization Findings
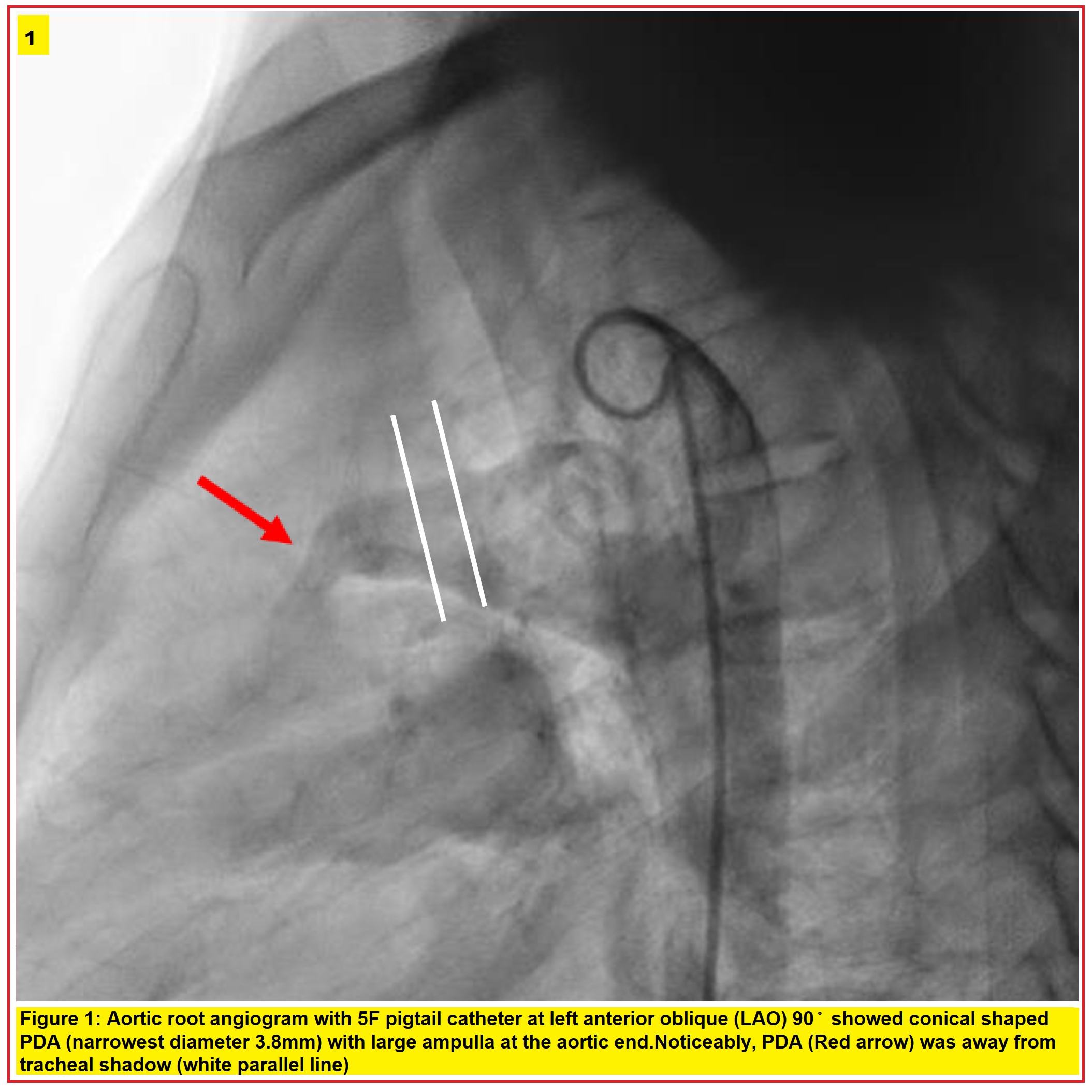
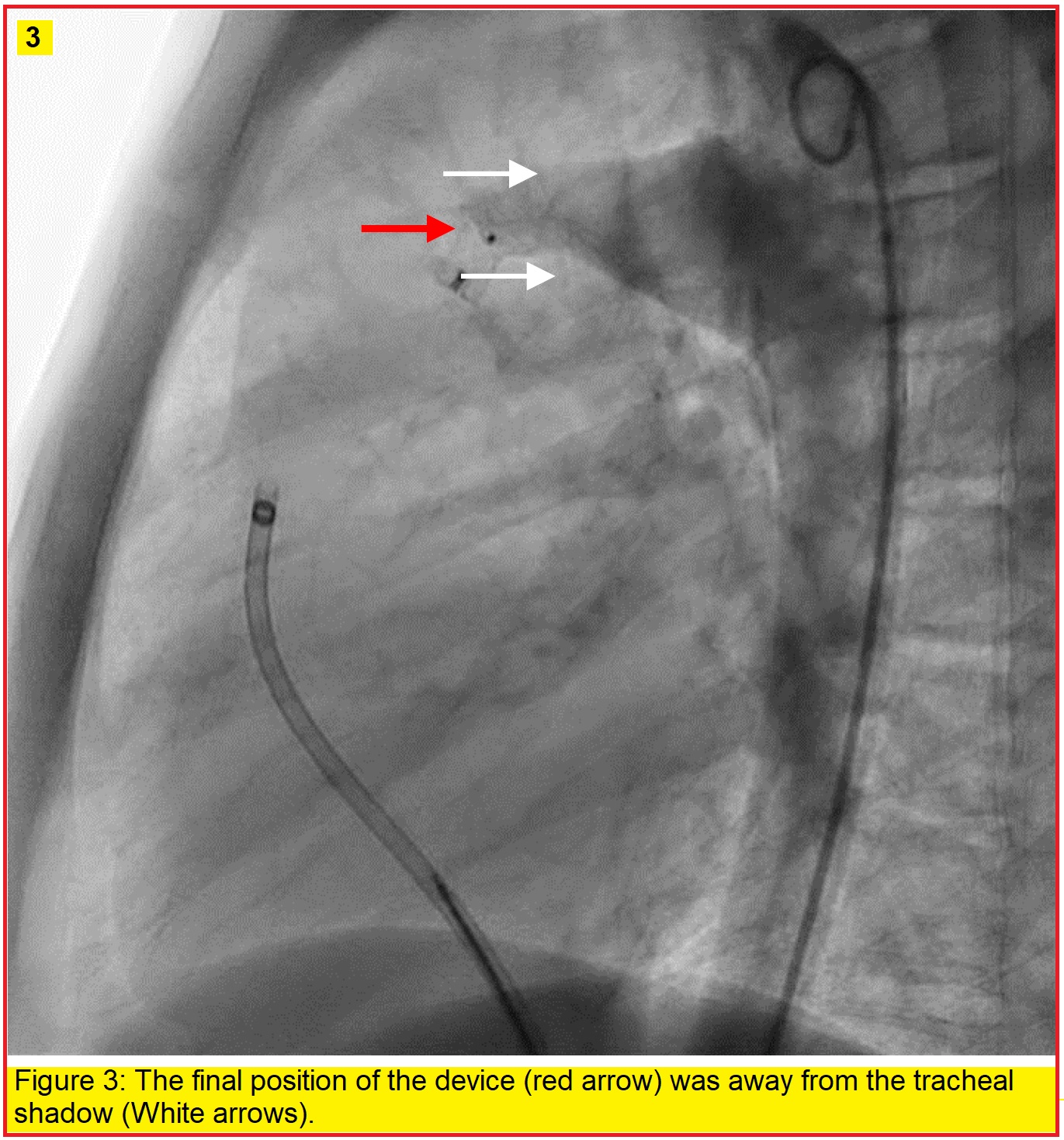
Cath study revealed pulmonary to systemic blood flow ratio (Qp/Qs) of 2.2:1 with pulmonary artery (PA) pressure of 38/18mmHg and Pulmonary Vascular resistance of 3.2 woods unit. Therefore, the patient was advised for PDA device closure. Aortic root angiogram with 5F pigtail catheter at left anterior oblique 900 showed conical shaped PDA (narrowest diameter 3.8 mm) with large ampulla at the aortic end. Noticeably, PDA (Red arrow) was away from tracheal shadow (white parallel line in figure 1).
Interventional Management
Procedural Step
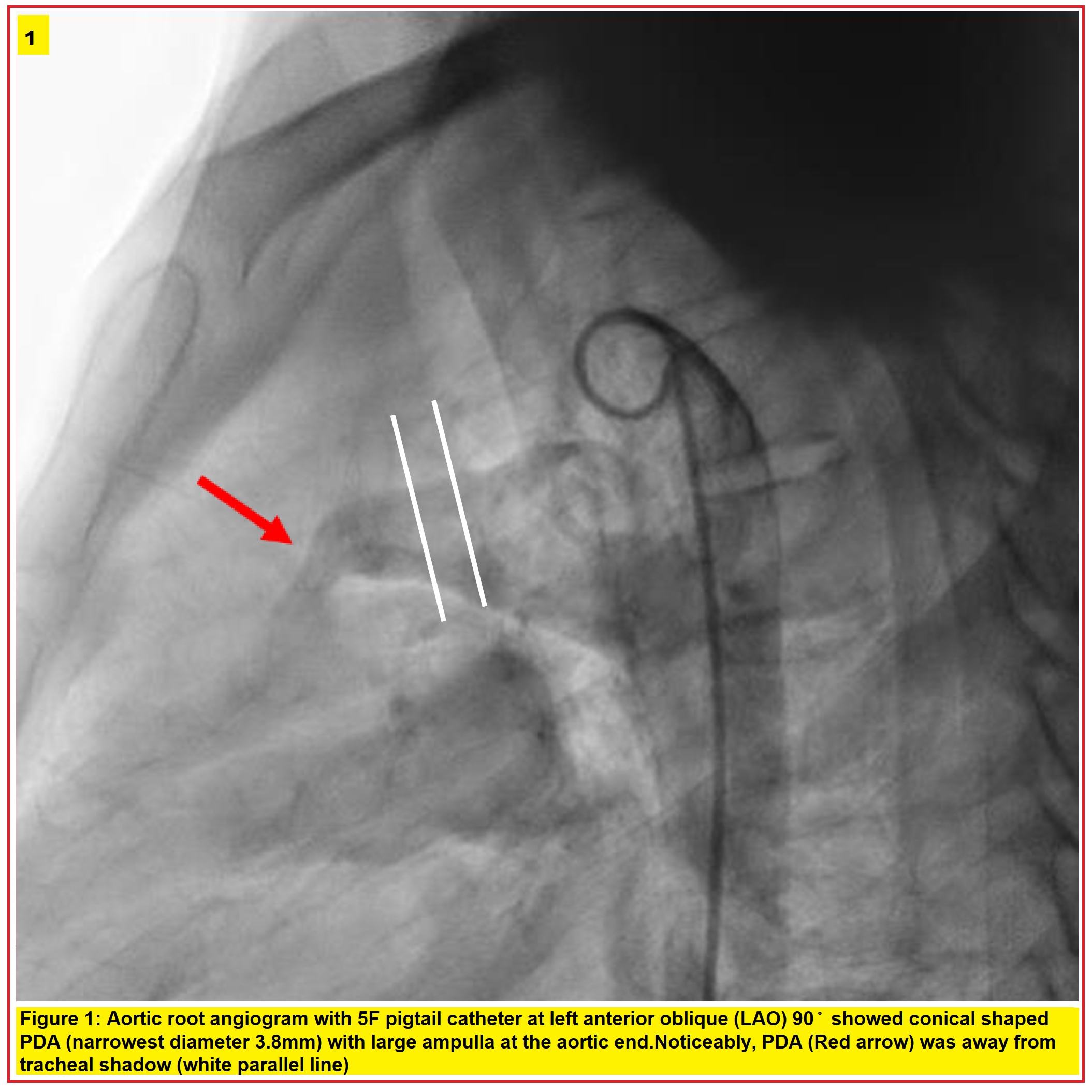
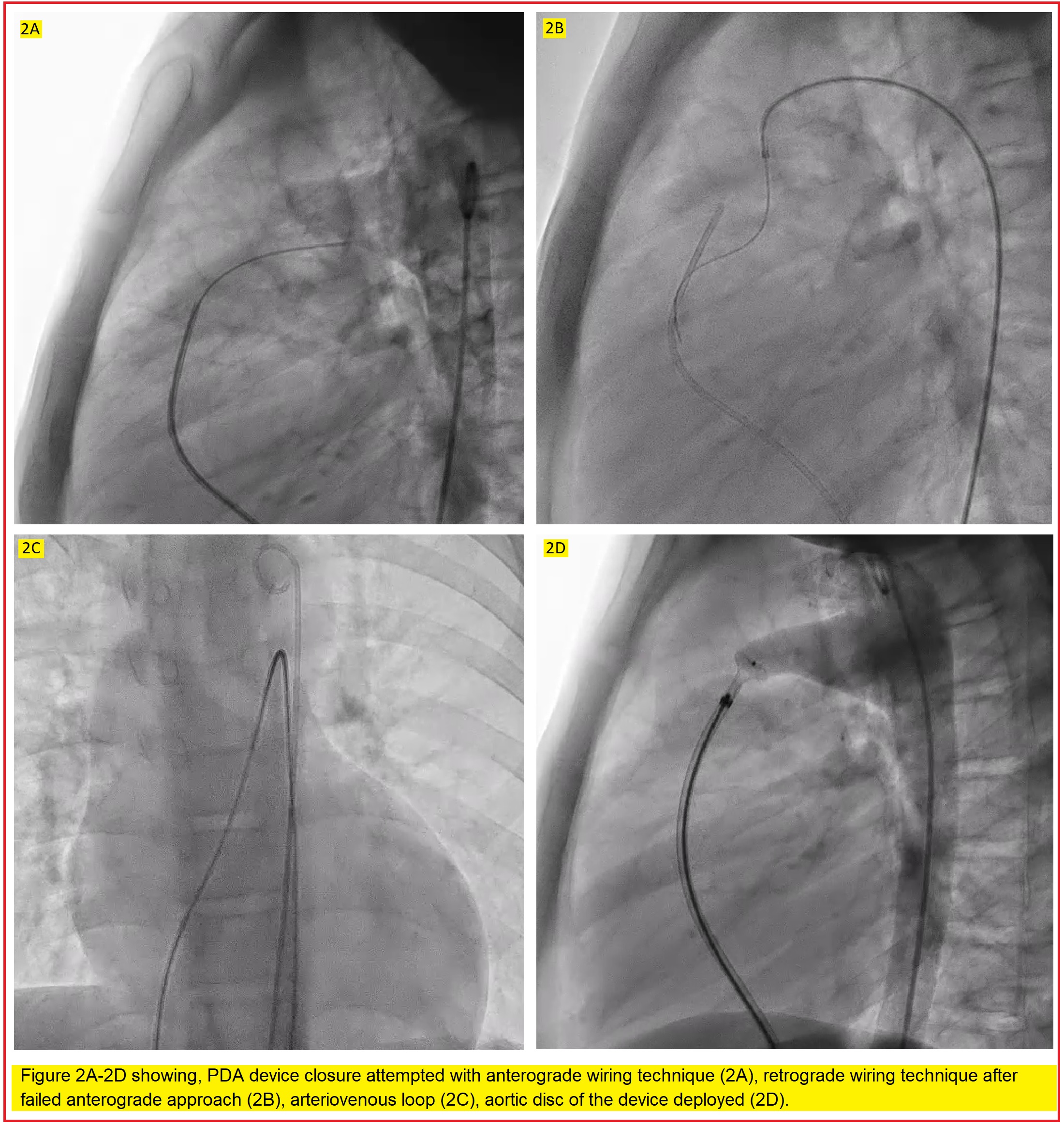
Wire was advanced from the venous end to cross the PDA from pulmonary end; however, it could not be done anterogradely. (Figure 2A) Therefore, it was attempted retrogradely from the arterial end to cross the PDA from aortic side followed by snaring of the pulmonary end of the wire from venous side. It was done successfully to form arteriovenous loop. (Figure 2B,2C). Then 8F device delivery system was advanced from right femoral vein to the inferior vena cava (IVC), right atrium (RA),right ventricle (RV), PA and through the PDA into the aorta. PDA Device (ADO-I, 8F/6F) was passed through the delivery sheath and successfully deployed across the PDA. (Figure 2D) However, the position of the device was away from the tracheal shadow.(Figure 3)
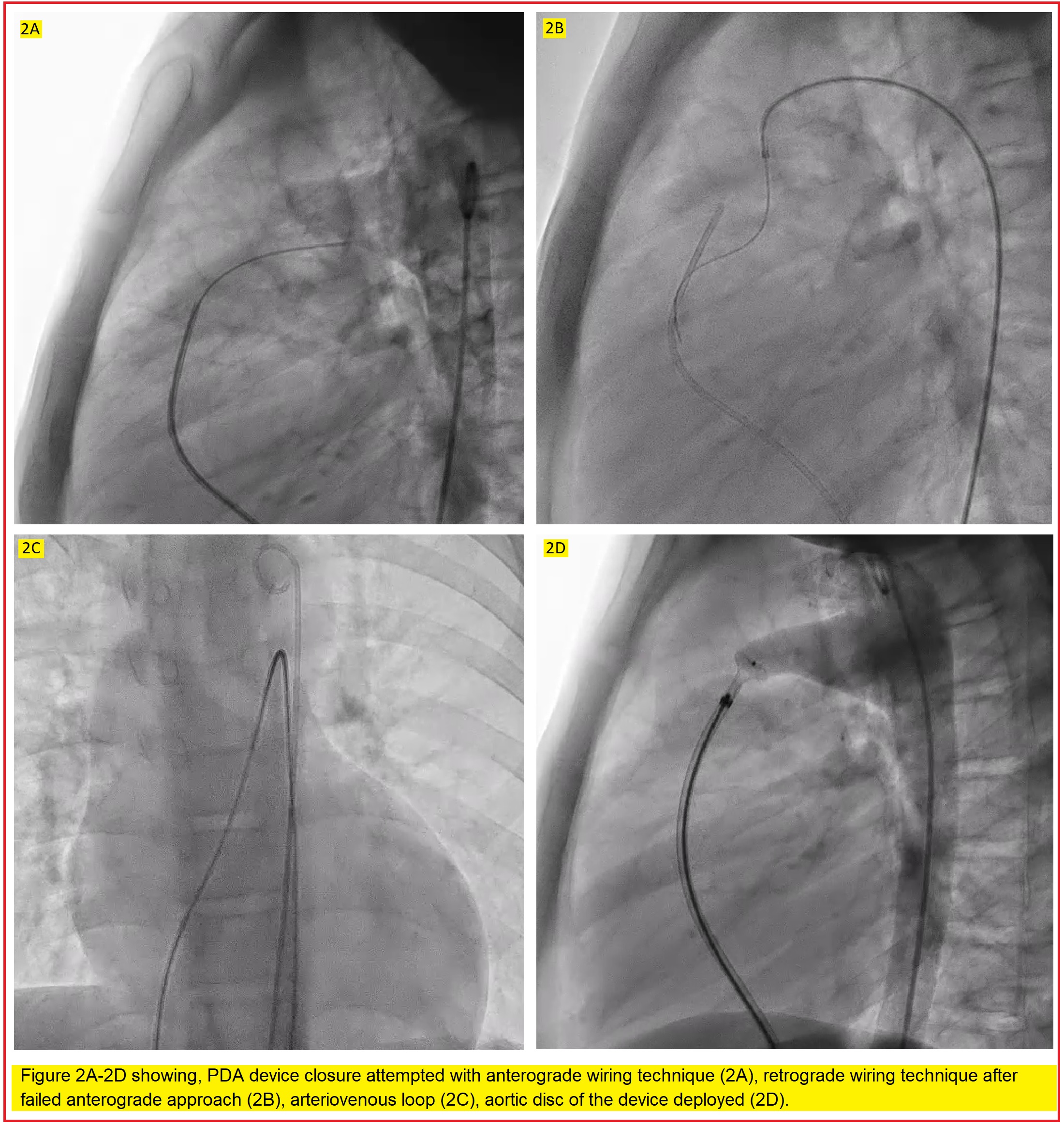
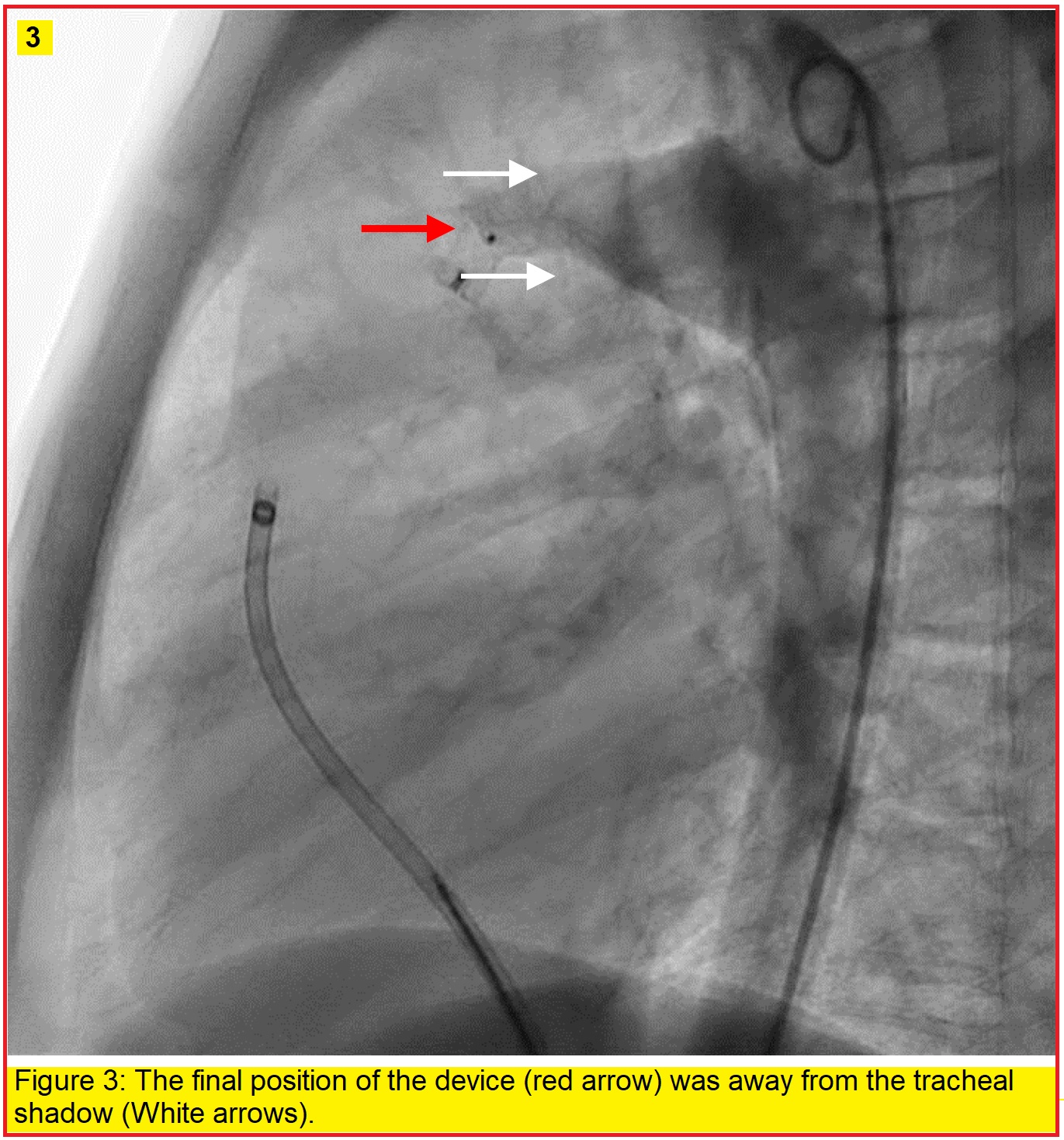
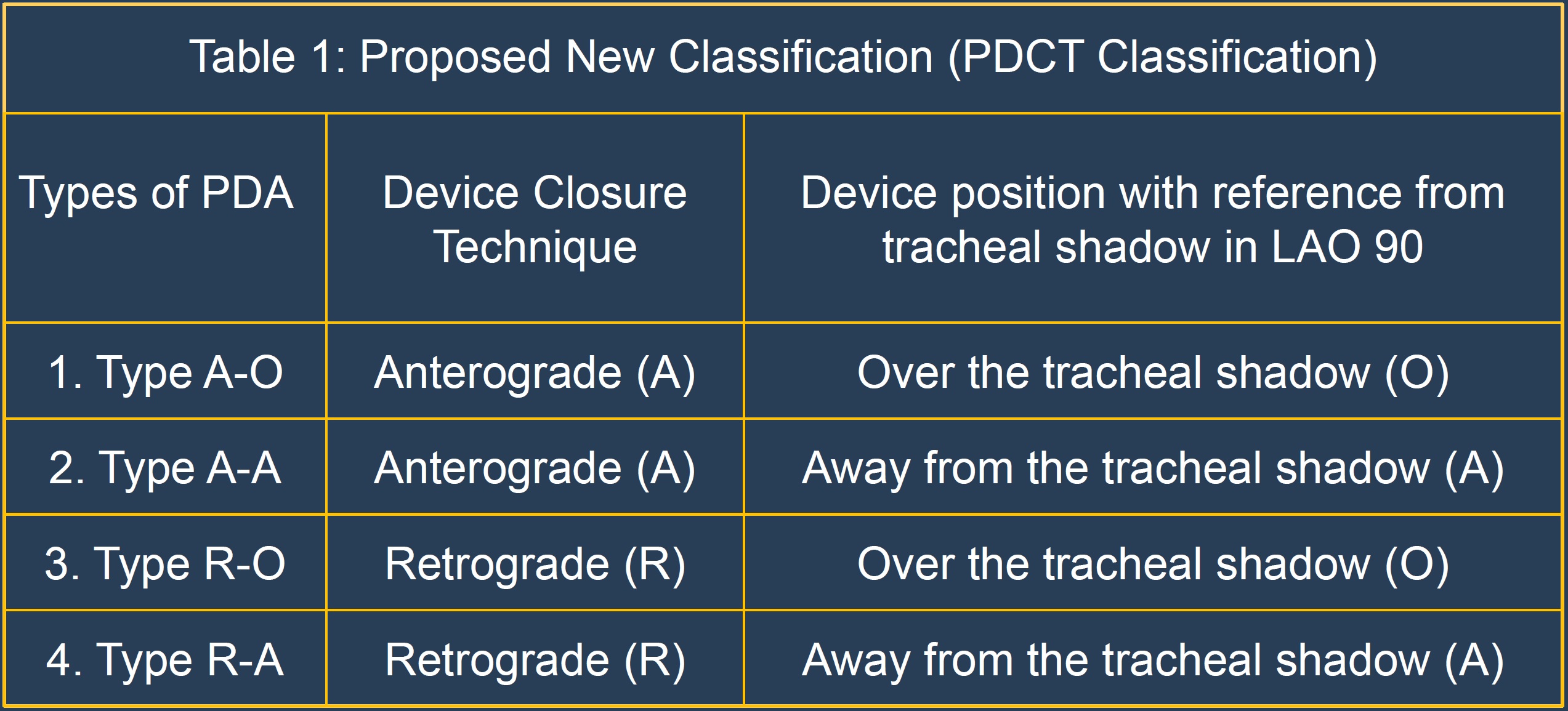
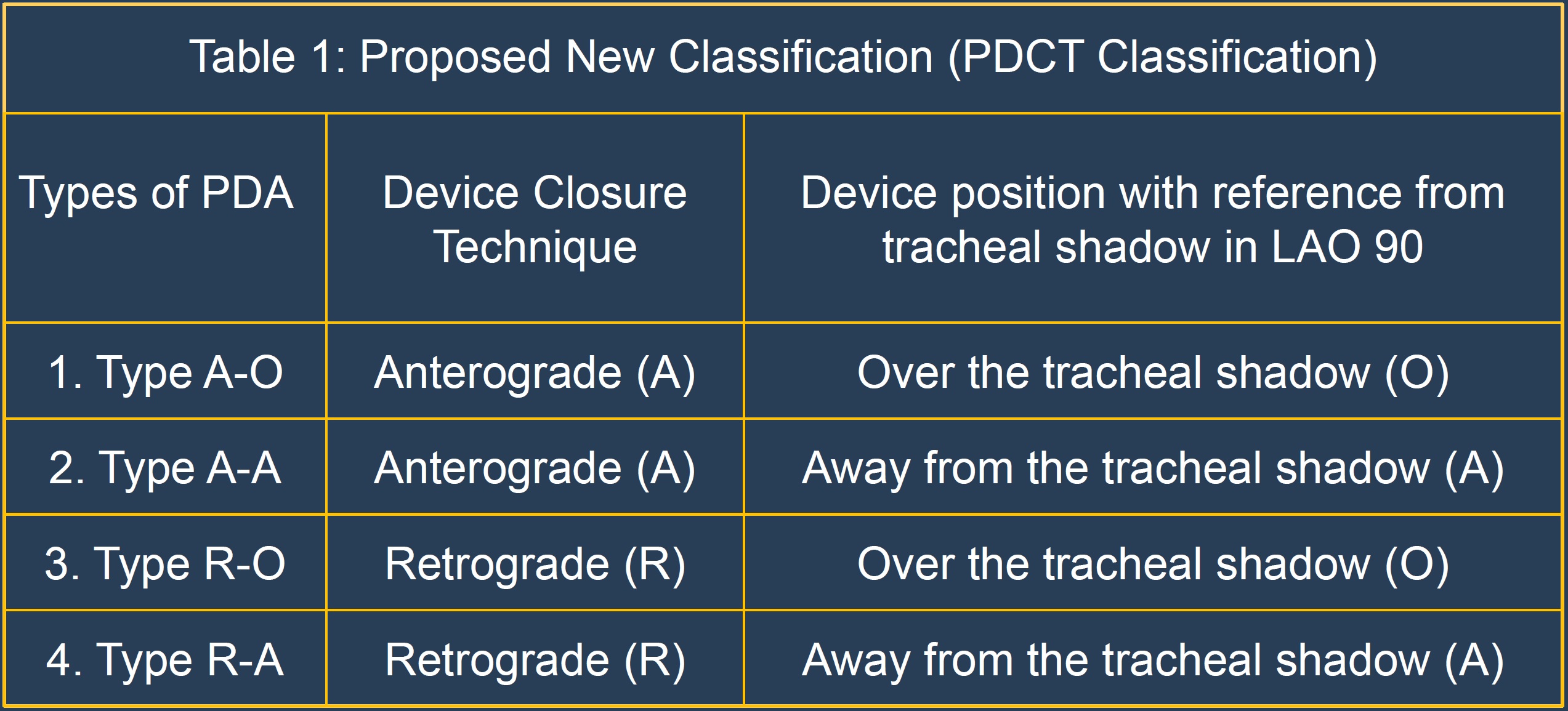
Case Summary
This classification scheme (table 1) will help in providing the data on PDA requiring anterograde/retrograde technique with final device position over or away from the trachea. With such information unnecessary prolonged procedure and radiation exposure in attempting the anterograde technique can be avoided if abnormal anatomy unsuitable for this technique is well anticipated on fluoroscopy and therefore successful device closure can be performed with retrograde technique. Moreover, in such cases, the final position of the device may not be over the tracheal shadow and therefore unnecessary doubts requiring repeated angiogram and fluoroscopy to reassure final device position can be avoided.


