Lots of interesting abstracts and cases were submitted for TCTAP 2022. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-101
Lost and Found
By David Yong, Beni Isman Rusani, Shaiful Azmi Yahaya
Presenter
David Yong
Authors
David Yong1, Beni Isman Rusani1, Shaiful Azmi Yahaya1
Affiliation
National Heart Institute, Malaysia1,
View Study Report
TCTAP C-101
CORONARY - Complications
Lost and Found
David Yong1, Beni Isman Rusani1, Shaiful Azmi Yahaya1
National Heart Institute, Malaysia1,
Clinical Information
Patient initials or Identifier Number
MNMK
Relevant Clinical History and Physical Exam
Presenting a case of a 84 year old gentleman with background history of hypertension and recent covid-19 infection. Following discharge from covid-19 pneumonia, he presented to our centre on 7/7/2021 for persistent chest pain. Clinical examination showed stable vital signs BP 124/63mmHg with heart rate of 72 beats per minute. There was clinically no signs of heart failure. He was diagnosed with acute coronary syndrome and initiated on treatment.
Relevant Test Results Prior to Catheterization
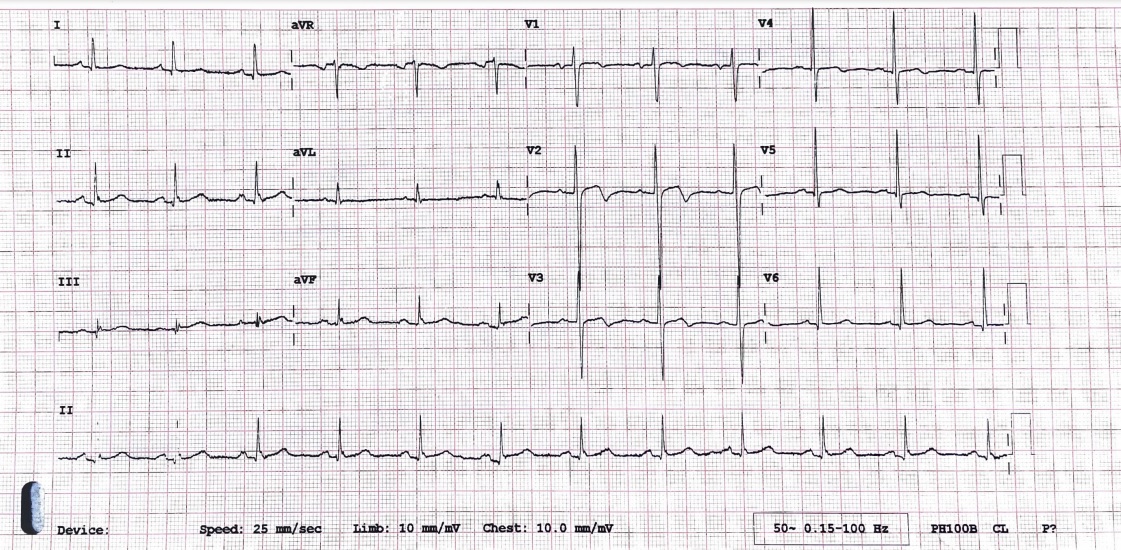
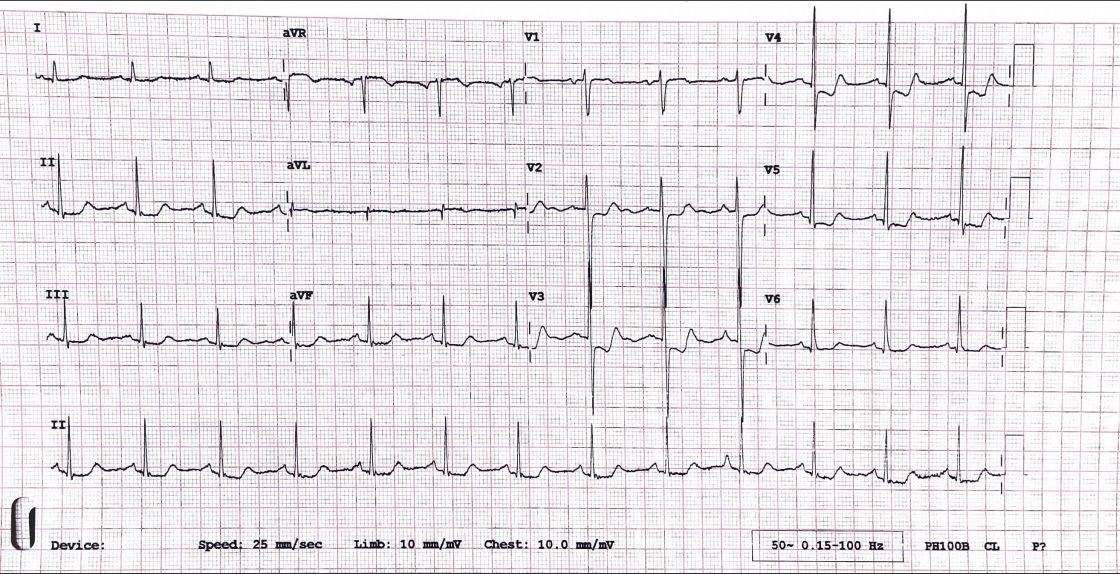
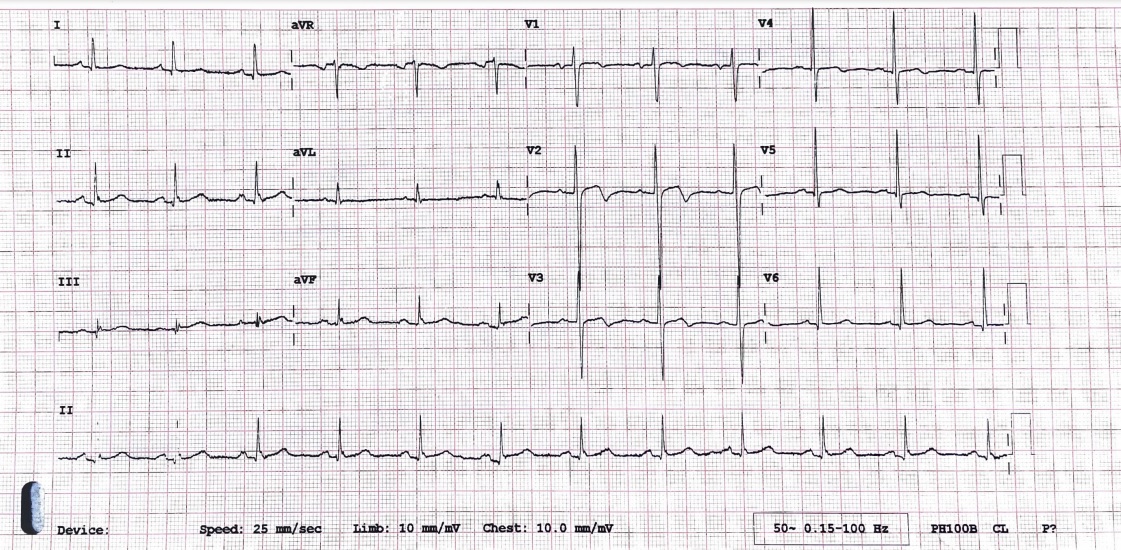
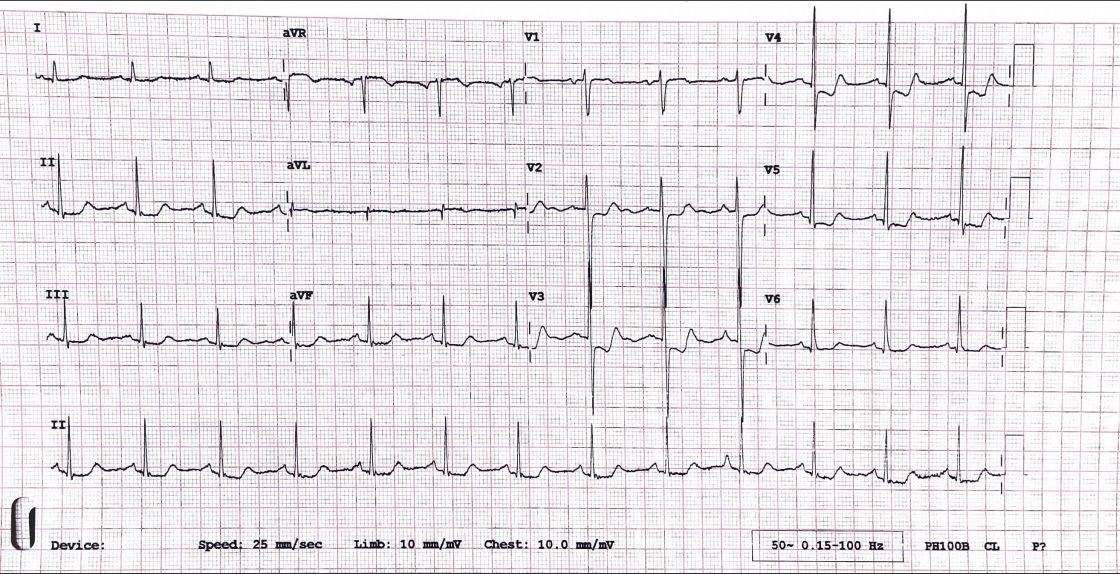
ECG done on day 1 of admission showed biphasic T waves indicative of Wellen Syndrome. Repeated ECG on day 2 of admission showed ST depression over v2-v6. hsTrop- T was marginally elevated at 26pg/ml. Echocardiogram showed normal ejection fraction 55% with no regional wall motion abnormality and mild aortic regurgitation.
Relevant Catheterization Findings
Diagnostic angiogram of the left system showed severe disease at the proximal left circumflex, proximal obtuse marginatum 1 and proximal left anterior descending artery. The right coronary artery was however anomalous and does not originate from the right coronary cusp. While attempting to locate the right coronary artery which we suspect originate from the left coronary cusp, the diagnostic catheter was engaged deeply into the left anterior descending causing dissection and no flow.
 443400 Caudal.avi
443400 Caudal.avi
 443400 deep catheter spider.avi
443400 deep catheter spider.avi
 443400 Caudal slow flow LAD.avi
443400 Caudal slow flow LAD.avi
Interventional Management
Procedural Step
Immediately after the complication occured, the patient developed hypotension due to cardiogenic shock. Intra-aortic balloon pump was inserted via left femoral access and vasopressors were initiated for circulatory support. Left main coronary artery was engaged with EBU 3.5. Inital attempt to wire the left anterior descending (LAD) artery with a Runthrough Floppy wire was unsuccessful and entered the diagonal. A second wire, Sion Blue was used as a parralel wire in an attempt to wire the LAD but was unsuccessful. A FIELDER XT-A was used to wire the LAD successfully into the distal true lumen. A semi-compliant 2.5/15 balloon was used to dilate the dissection flap area at nominal pressure. Post balloon dilation, flow down the LAD was re-established. A DES 3.5/28 was deployed at the proximal LAD. Post dilation with non-compliant balloon was performed up to 18atm for stent optimisation. Post procedure patient hemodynamics improved and we were able to off the balloon pump and vasopressor support. Subsequently, a MSCT coronary was performed confirming the right coronary artery originating from the left coronary cusp. However, it was small and non-dominant, thus a decision for optimal medical therapy was taken and no further invasive coronary intervention was performed for this patient.
 443400 wire with soft wire spider.avi
443400 wire with soft wire spider.avi
 443400 Fielder wiring.avi
443400 Fielder wiring.avi
 443400 Spider final.avi
443400 Spider final.avi
Case Summary
Iatrogenic coronary artery dissection during catheterization is one of the major complication seen during such procedures. In our case, the dissection flap has closed the proximal LAD true lumen causing no flow and cardiogenic shock. Adequate cardiac circulatory support should be initiated immediately as was done in our case with vasopressors and intra-aortic balloon pump. Wiring the LAD with soft wire was unsuccessful likely due to the slit like opening of the true lumen caused by the dissection flap. Fielder XT-A designed with a tapered tip and polymer coating was able to navigate the slit opening and cross into the distal true lumen.


