Lots of interesting abstracts and cases were submitted for TCTAP 2022. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-030
Ten Years Survival Benefit and Appropriateness of Surgical or Percutaneous Revascularization Based on Individual Predicted All-Cause Mortality in Patients With Complex Coronary Artery Disease
By Patrick W. Serruys, Chao Gao, Scot Garg, Yoshinobu Onuma, David R. Holmes, Marie-Claude Morice, Friedrich Wilhelm Mohr, Michael J. Mack
Presenter
Patrick W. Serruys
Authors
Patrick W. Serruys1, Chao Gao2, Scot Garg3, Yoshinobu Onuma1, David R. Holmes4, Marie-Claude Morice5, Friedrich Wilhelm Mohr6, Michael J. Mack7
Affiliation
University of Galway, Ireland1, Xijing Hospital, China2, Royal Blackburn Hospital, United Kingdom3, Mayo Clinic, USA4, CERC, France5, Herzzentrum Universitaet Leipzig, Germany6, Baylor University Medical Center, USA7
View Study Report
TCTAP A-030
Bifurcation/Left Main Diseases and Intervention
Ten Years Survival Benefit and Appropriateness of Surgical or Percutaneous Revascularization Based on Individual Predicted All-Cause Mortality in Patients With Complex Coronary Artery Disease
Patrick W. Serruys1, Chao Gao2, Scot Garg3, Yoshinobu Onuma1, David R. Holmes4, Marie-Claude Morice5, Friedrich Wilhelm Mohr6, Michael J. Mack7
University of Galway, Ireland1, Xijing Hospital, China2, Royal Blackburn Hospital, United Kingdom3, Mayo Clinic, USA4, CERC, France5, Herzzentrum Universitaet Leipzig, Germany6, Baylor University Medical Center, USA7
Background
To compare the observed and individual predicted mortalities according to the SYNTAX score II 2020 (SSII-2020) in the all-comers SYNTAX population, and retrospectively assess the appropriateness of revascularization with percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG) in patients with three vessel disease (3VD) and/or left main disease (LMCAD).
Methods
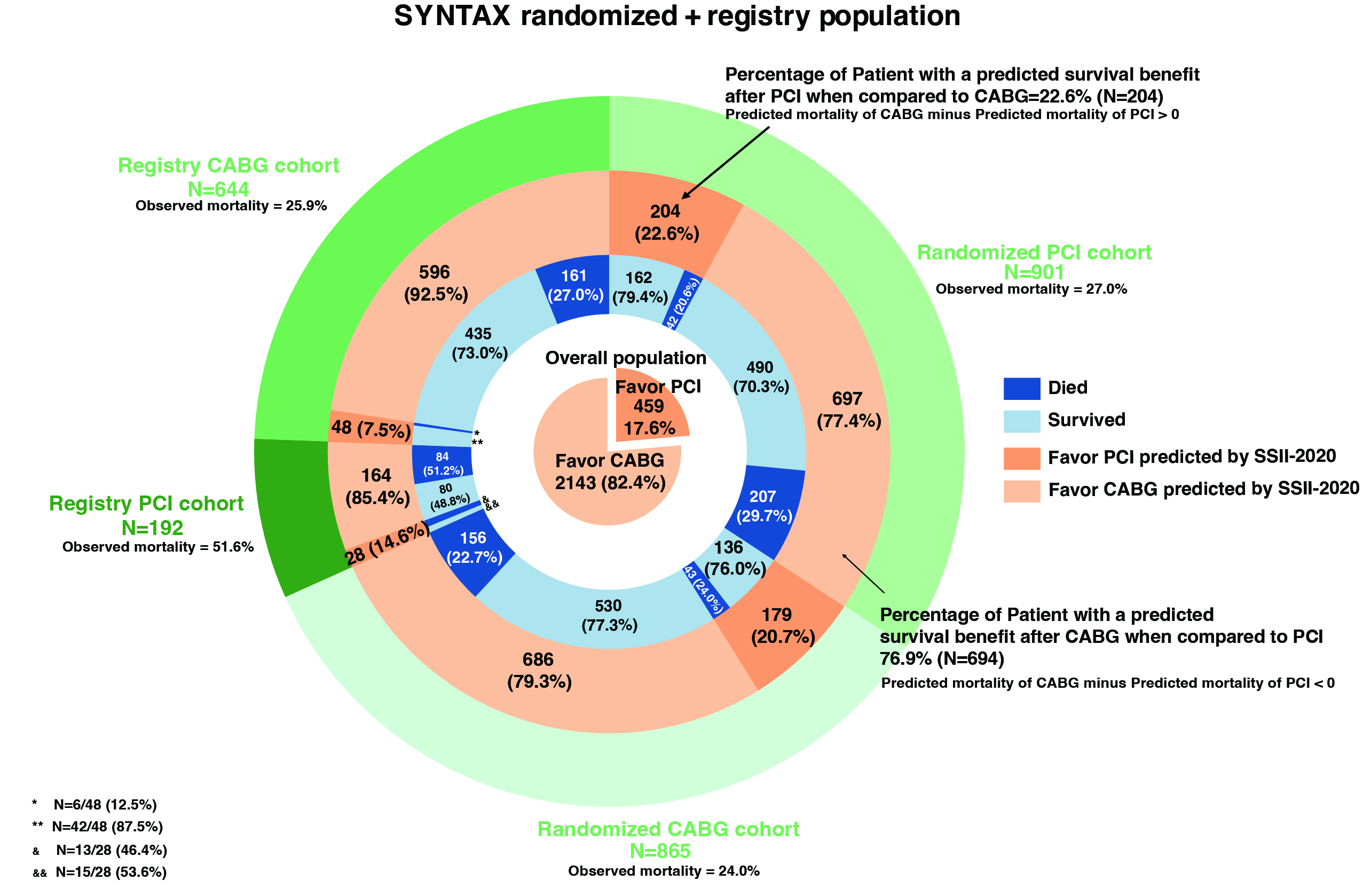
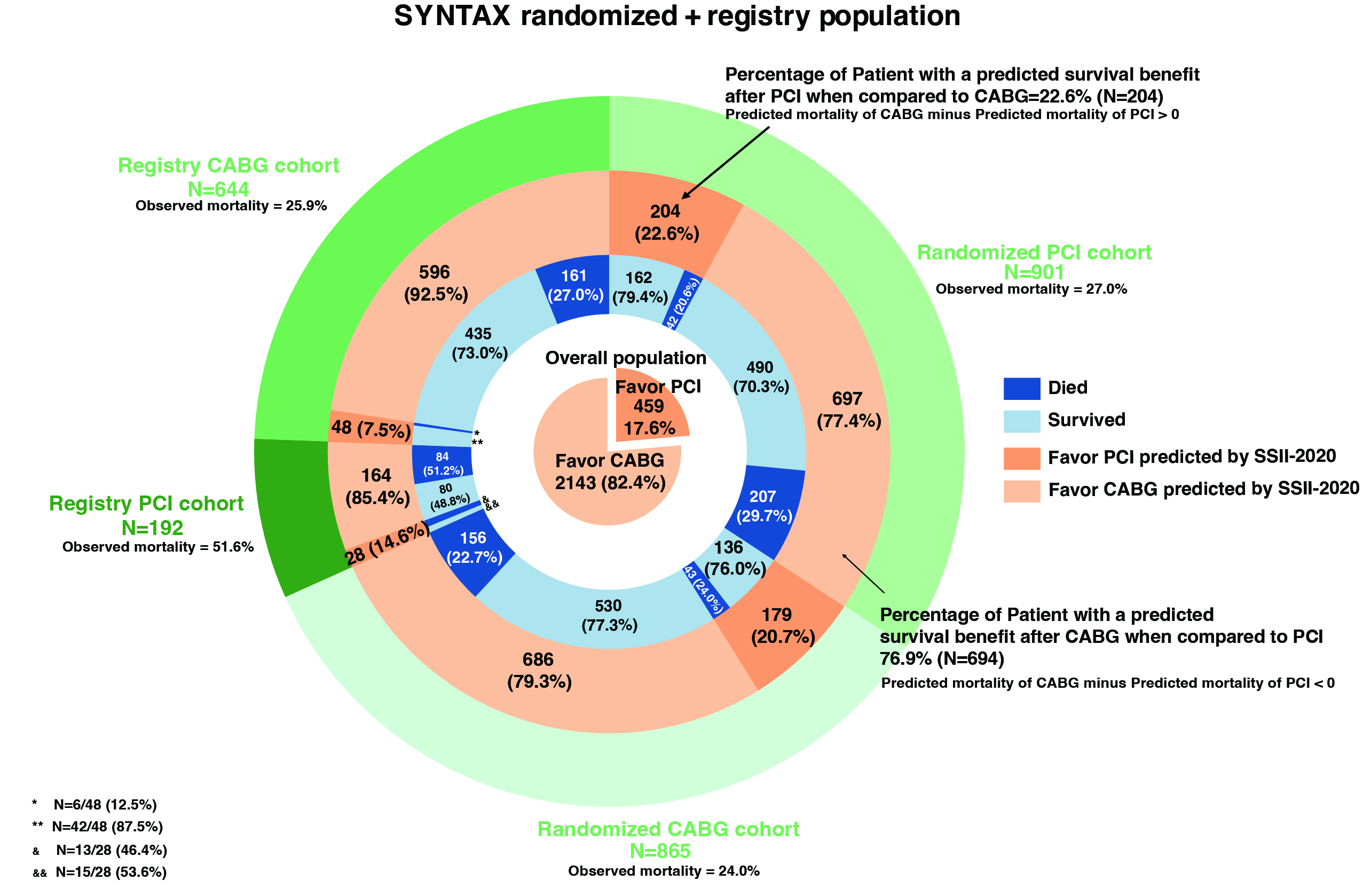
Internal and external validation of the SSII-2020 to predict 10-year all-cause death was performed in the respective randomized and registry SYNTAX populations. Differences in individual predicted mortalities following CABG or PCI were ranked and displayed with the observed mortalities. The proportions of screened patients deriving a survival benefit from CABG or PCI were determined retrospectively.
Results
A total of 2602 participants (as-treated population) were included in the randomized and registry cohorts. In the randomized cohort, all-cause mortality at 10 years, as an average treatment effect, was 23.8% (199/865) with CABG and 28.6% (249/901) with PCI, with a differential survival benefit of 4.6% (95% CI: 0.58% to 8.7%, log-rank p value=0.023). In the CABG and PCI registries, mortalities were 27.8% (167/644) and 55.4% (99/192), respectively. Calibration and discrimination of the SSII-2020 was helpful in CABG and PCI patients in the randomized and registry cohorts. In the PCI registry, the SSII-2020 underestimated mortality since specific comorbidities that entail high mortality are not included in the formula (C-index: 0.72, intercept: 0.38, slope: 0.66), whilst in the CABG registry, it predicted mortality with a helpful calibration and discrimination (C-index: 0.70, intercept: 0.00, slope: 0.76). The proportions of patients with a predicted survival benefit following CABG and PCI were respectively 78.3% (1383/1766) and 21.7% (383/1766) in the randomized cohort, and 82.4% (2143/2602) and 17.7% (459/2602) in the whole SYNTAX trial population.
Conclusion
In the randomized and registery cohort of this all-comers population with 3VD and/or LMCAD, there was reasonable agreement between the individual predicted and observed mortalities after CABG or PCI, such that the predicted 10-year survival benefit might be helpful in determining the appropriateness of each modality of revascularization.