Lots of interesting abstracts and cases were submitted for TCTAP 2022. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-051
Early and Long-Term Outcome of Intravascular Ultrasonography-Guided Primary Percutaneous Coronary Intervention in ST-Elevation Myocardial Infarction: A Network Meta-Analysis
By Gusti Ngurah Prana Jagannatha, Nikita Toding Labi, Ketut Angga Aditya Putra Pramana, Yusra Pintaningrum
Presenter
Gusti Ngurah Prana Jagannatha
Authors
Gusti Ngurah Prana Jagannatha1, Nikita Toding Labi2, Ketut Angga Aditya Putra Pramana3, Yusra Pintaningrum3
Affiliation
Udayana University, Indonesia1, Sam Ratulangi University, Indonesia2, Mataram University, Indonesia3
View Study Report
TCTAP A-051
Imaging: Intravascular
Early and Long-Term Outcome of Intravascular Ultrasonography-Guided Primary Percutaneous Coronary Intervention in ST-Elevation Myocardial Infarction: A Network Meta-Analysis
Gusti Ngurah Prana Jagannatha1, Nikita Toding Labi2, Ketut Angga Aditya Putra Pramana3, Yusra Pintaningrum3
Udayana University, Indonesia1, Sam Ratulangi University, Indonesia2, Mataram University, Indonesia3
Background
Several studies have shown that intravascular ultrasonography (IVUS) guidance provide a good long-term outcome in patients with acute myocardial infarction. However, because IVUS use is associated with delay in revascularization time, the addition of IVUS in primary percutaneous coronary intervention (PPCI) of ST-elevation myocardial infarction (STEMI) patients is still unclear regarding the benefit.
Methods
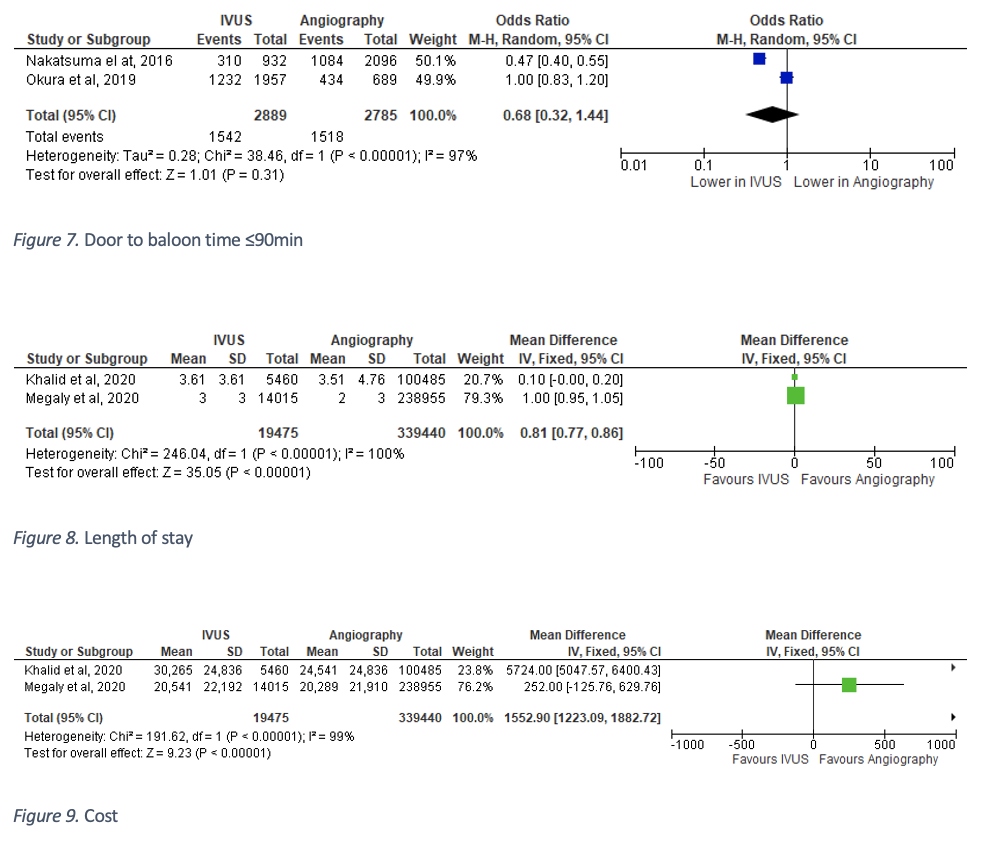
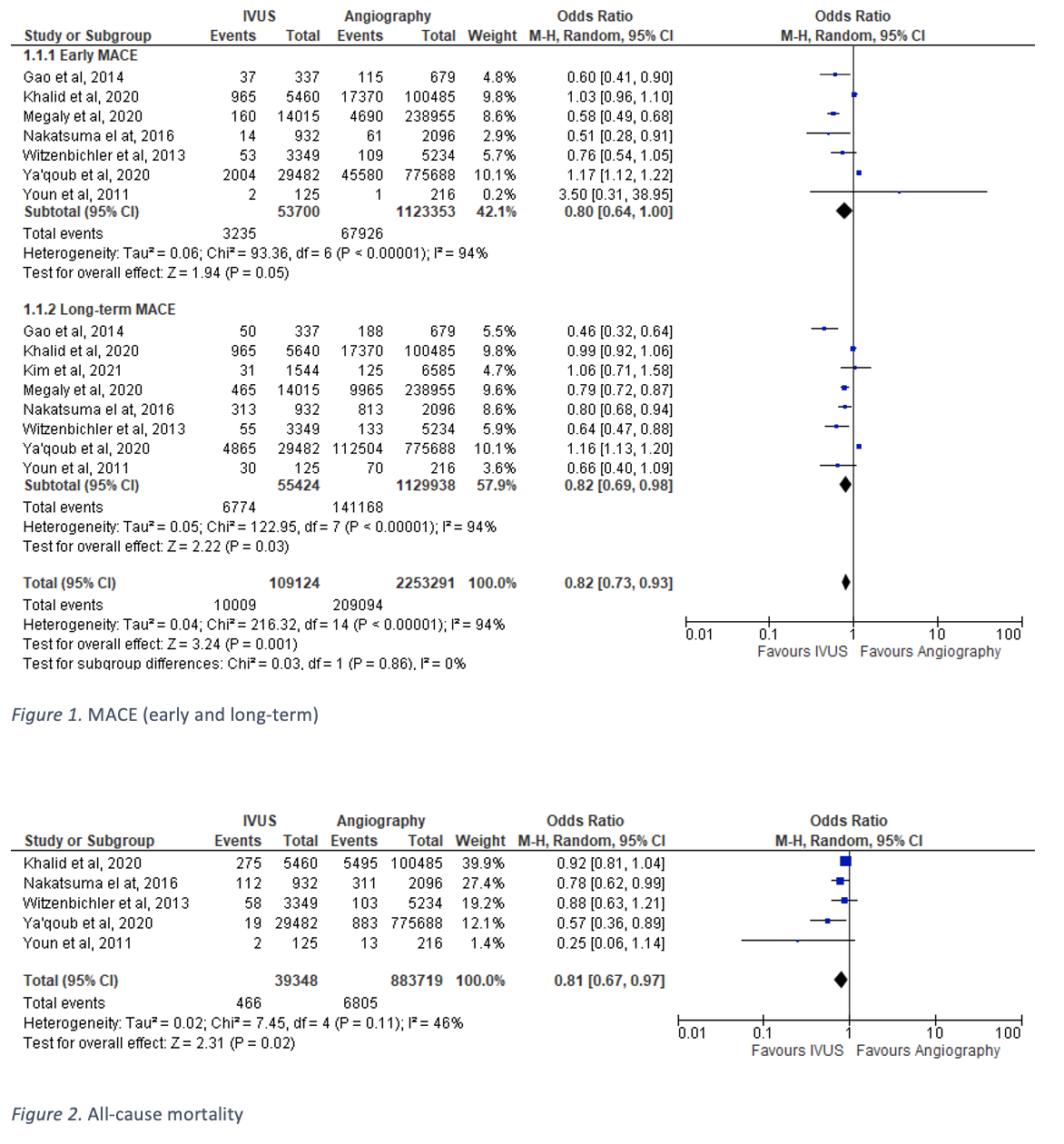
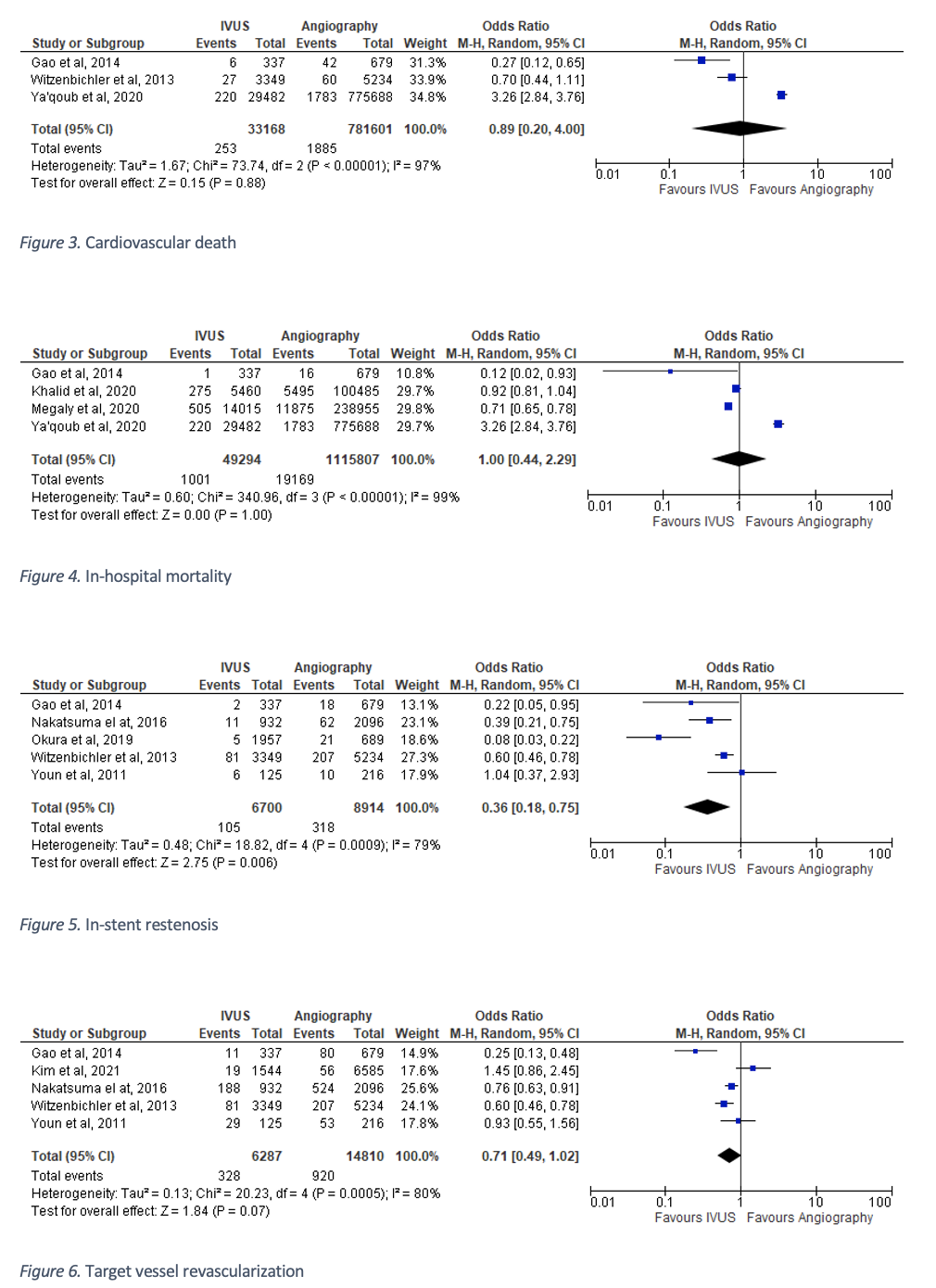
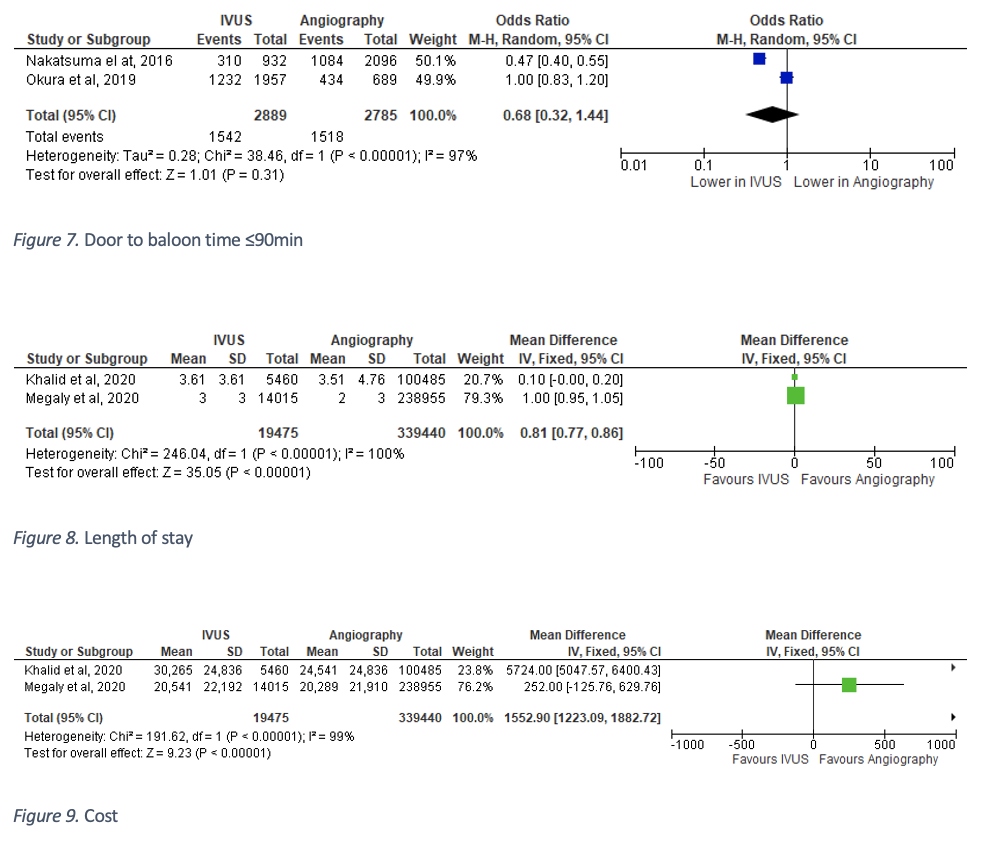
We performed a systematic search in databases (PubMed, ScienceDirect, ProQuest, and Cochrane Library) for studies comparing IVUS-guided and angiography-guided PPCI in STEMI. Review Manager 5.4 was utilized to compute the summary of odds ratios (OR), mean differences (MD), and 95% CI for the outcomes. Our outcomes of interest are all-cause mortality, cardiovascular death, early and long-term major adverse cardiovascular events (MACE), in-hospital mortality, in-stent restenosis (ISR), target vessel revascularization (TVR), door-to-baloon time <90 minutes, length of stay, and cost.
Results
We identified ten observational studies involving 1,192,060 STEMI patients. Pooled analysis showed that IVUS-guided PPCI significantly reduced all-cause mortality [OR 0.81 (95% CI 0.67, 0.97; p=0.02; I2=46%)], early MACE [OR 0.80 (95% CI 0.64, 1.00; p=0.05; I2=94%)], and long-term MACE [OR 0.82 (95% CI 0.69, 0.98; p=0.03; I2=94%)] compared with angiography-guided PPCI, but there was no significant difference in cardiovascular death [OR 0.89 (95% CI 0.20, 4.00; p=0.88; I2=97%)] in both groups. The incidence of ISR [OR 0.36 (95% CI 0.18, 0.75; p=0.006; I2=79%)] and TVR [OR 0.71 (95% CI 0.49, 1.02; p=0.07; I2=80%)] were found to be significantly lower in patients with IVUS-guided PPCI group. When assessed in terms of the number of patients who achieved door-to-balloon time ≤90 minutes, there was no significant different in both groups, although the number was higher in angiography-guided PPCI. In line with that result, in-hospital mortality and length of stay were not significantly different in both groups. Significantly higher mean cost is required in IVUS-guided PPCI group.
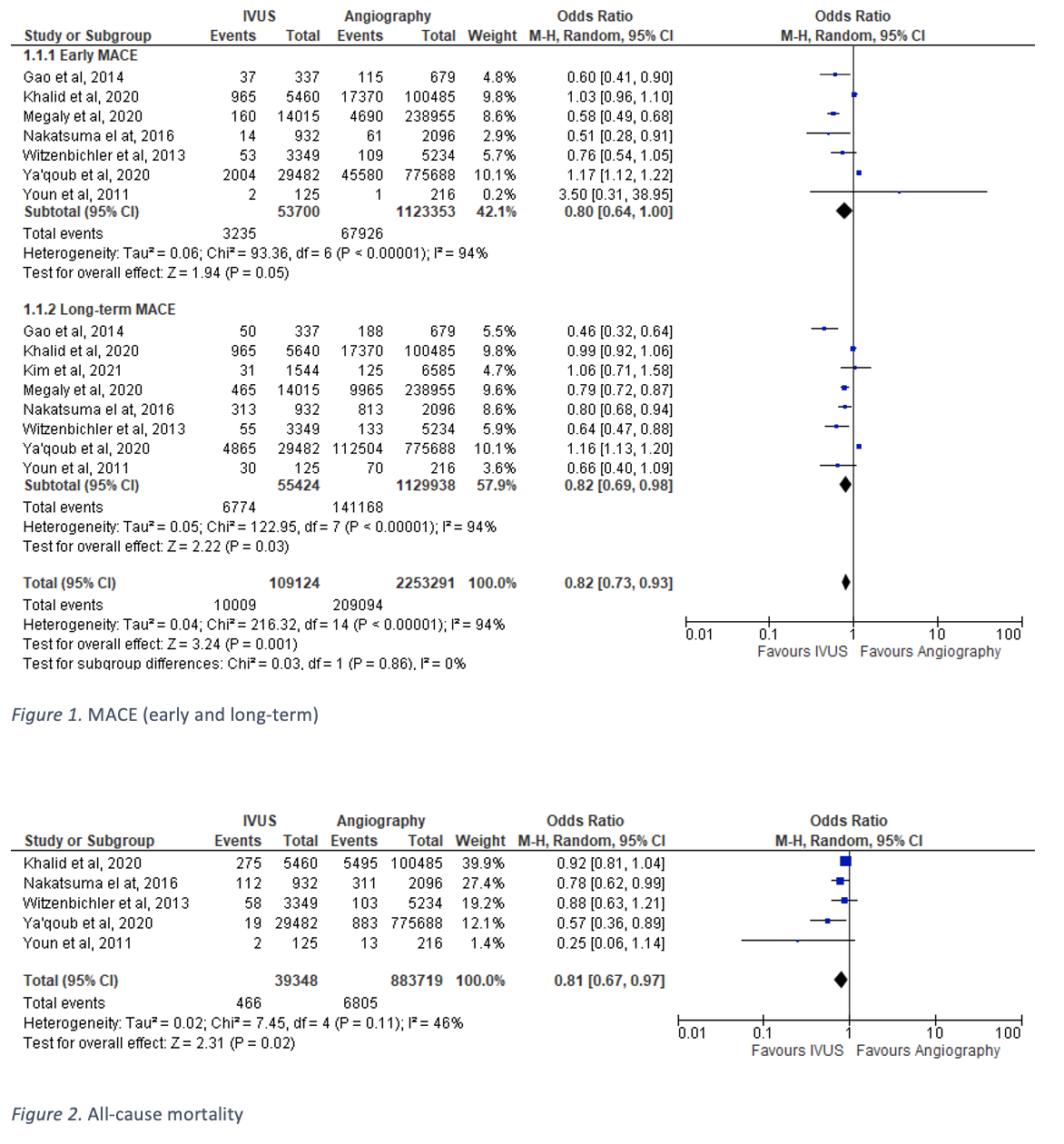
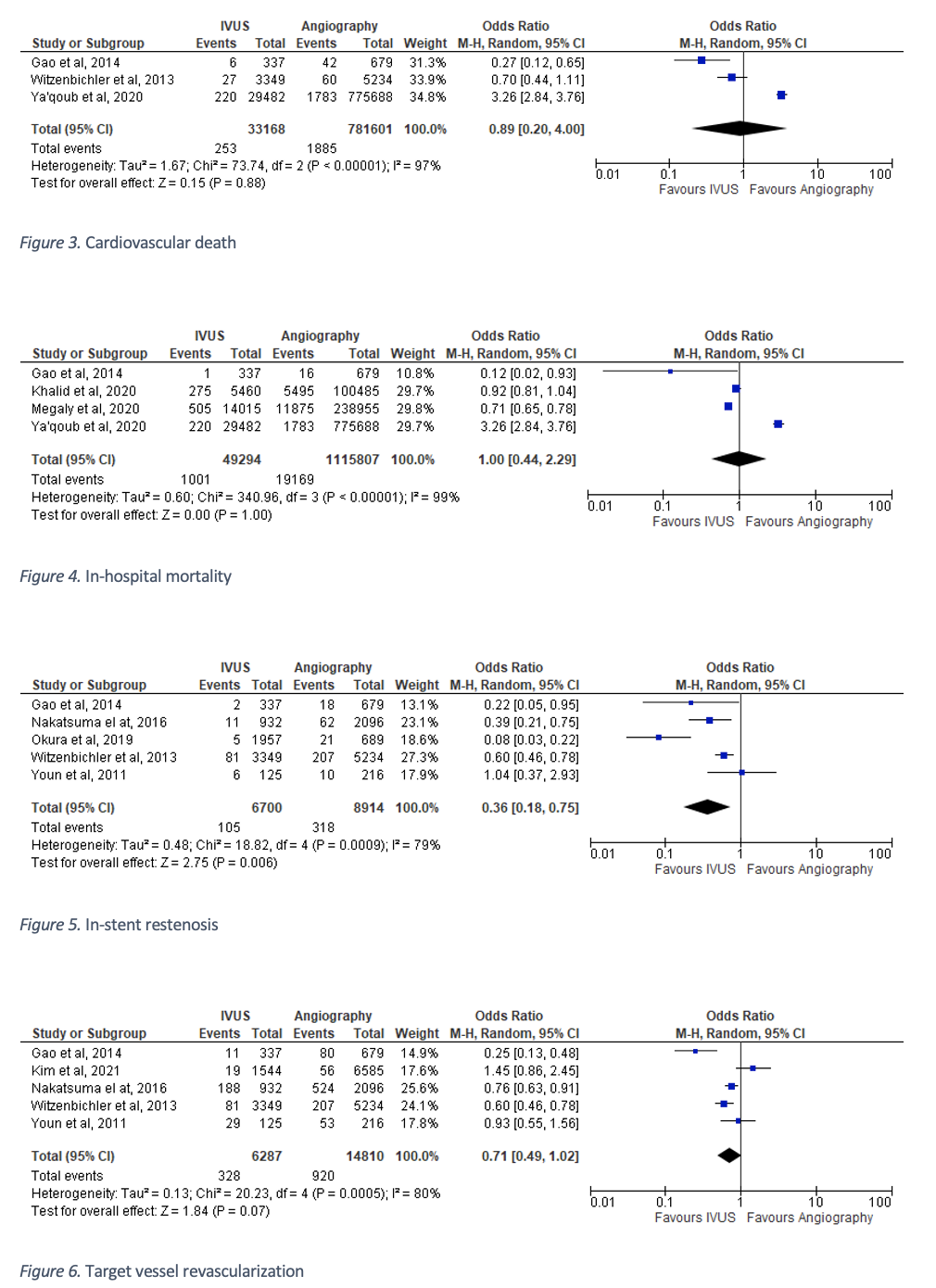
Conclusion
The addition of IVUS in PPCI of STEMI patients was associated with significant reduction of all cause mortality and MACE compared with angiography only guidance. Door-to-balloon time optimization has the potential to provide a desirable outcomes for STEMI patients with this strategy.


