Lots of interesting abstracts and cases were submitted for TCTAP 2022. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-028
Predicted and Observed Mortality at 10-Year in Patients With Bifurcation Lesion in The SYNTAX Trial
By Kai Ninomiya, Patrick W. Serruys, Shinichiro Masuda, Francesco Burzotta, Marie-Claude Morice, Michael J. Mack, David R. Holmes, Yoshinobu Onuma
Presenter
Kai Ninomiya
Authors
Kai Ninomiya1, Patrick W. Serruys2, Shinichiro Masuda2, Francesco Burzotta3, Marie-Claude Morice4, Michael J. Mack5, David R. Holmes6, Yoshinobu Onuma2
Affiliation
Iwate Medical University, Japan1, University of Galway, Ireland2, The Gemelli University Hospital, Italy3, CERC, France4, Medical City Hospital, USA5, Mayo Clinic, USA6
View Study Report
TCTAP A-028
Bifurcation/Left Main Diseases and Intervention
Predicted and Observed Mortality at 10-Year in Patients With Bifurcation Lesion in The SYNTAX Trial
Kai Ninomiya1, Patrick W. Serruys2, Shinichiro Masuda2, Francesco Burzotta3, Marie-Claude Morice4, Michael J. Mack5, David R. Holmes6, Yoshinobu Onuma2
Iwate Medical University, Japan1, University of Galway, Ireland2, The Gemelli University Hospital, Italy3, CERC, France4, Medical City Hospital, USA5, Mayo Clinic, USA6
Background
Percutaneous coronary intervention (PCI) of bifurcation lesions is associated with higher rates of adverse events. Whether coronary artery bypass grafting (CABG) or PCI is a safer revascularization modality for bifurcation lesions remains to be elucidated. The SYNTAX score II 2020 (SSII-2020) can be used to individualize the prediction of all-cause mortality at 10-year after CABG or PCI. The present study is a subgroup analysis of the SYNTAXES, (The SYNTAX Extended Survival, NCT 03417050) an investigator-driven extended 10-year follow-up of the SYNTAX trial; the impact of bifurcation lesions on individual predicted and observed all-cause 10-year mortality was investigated in patients with 3VD and/or LMCAD undergoing PCI or CABG.
Methods
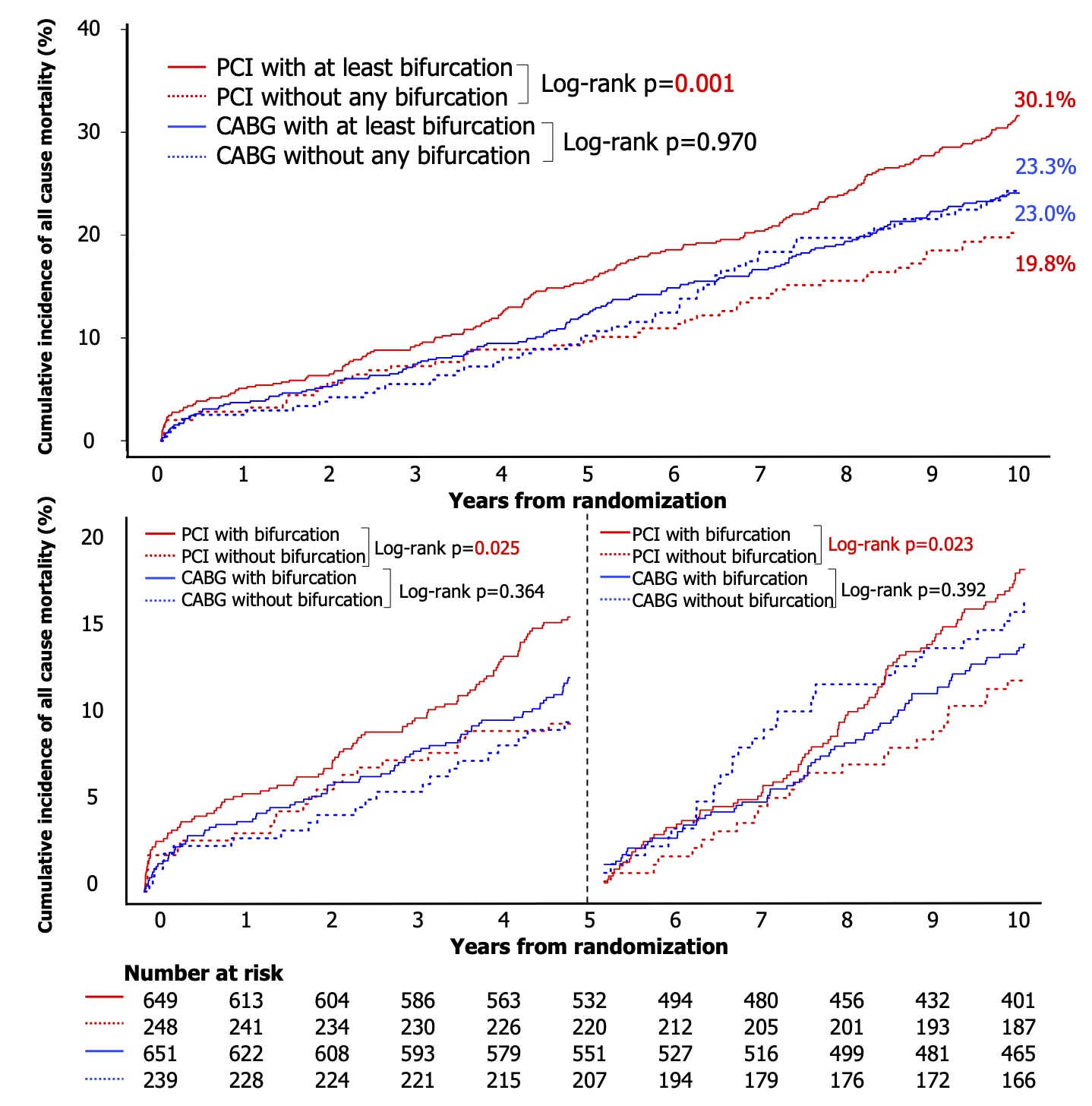
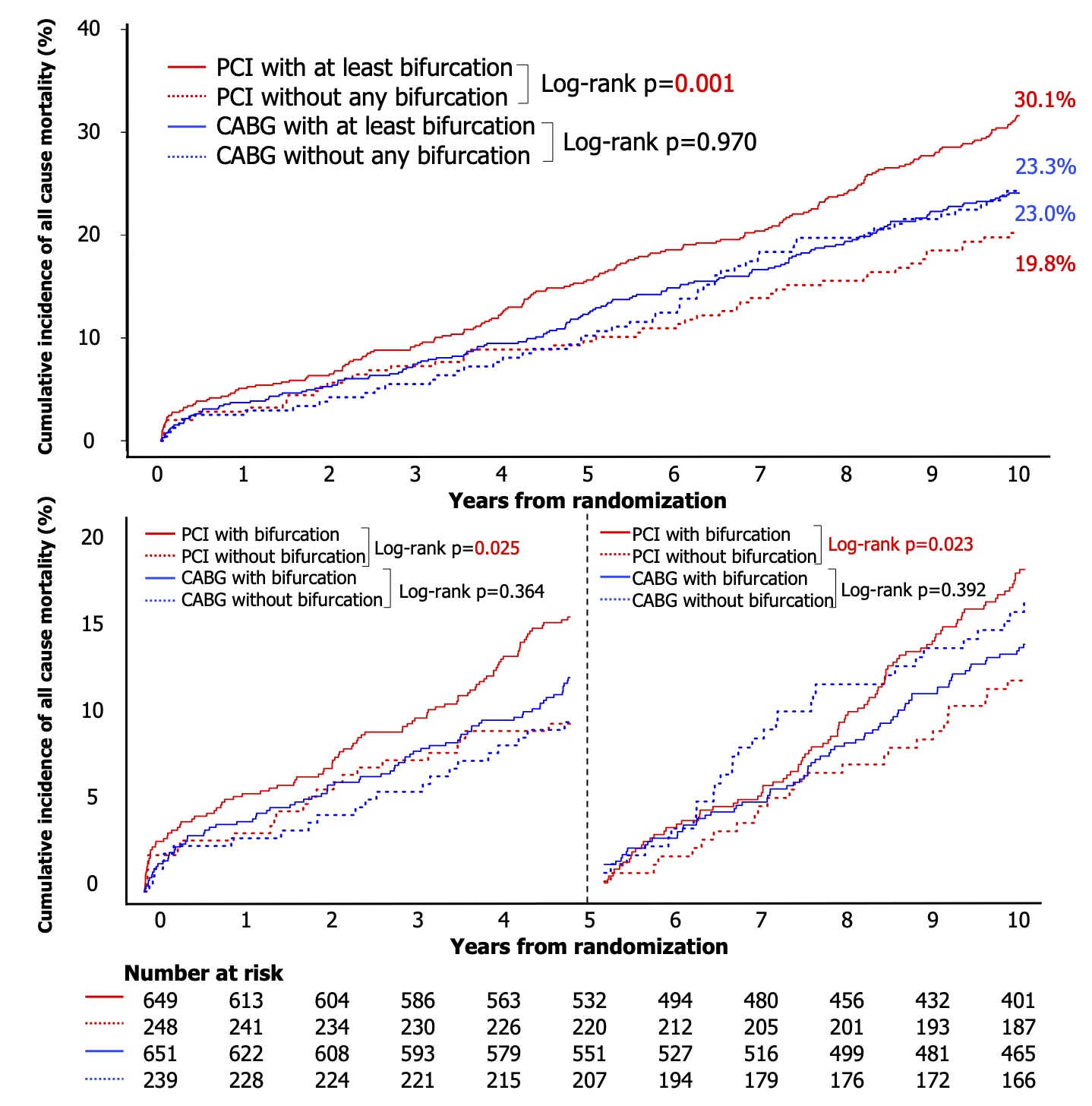
Patients were categorized in four groups: (a) presence of ≥1bifurcation lesion and treatment with PCI, (b) no bifurcation lesion and treatment with PCI, (c) presence of ≥1bifurcation lesion and treatment with CABG, and (d) no bifurcation lesion and treatment with CABG. The primary endpoint was all-cause mortality at 10-year.
Results
In patient receiving PCI, compared to those without a bifurcation lesion, those with bifurcation lesion(s) had a significantly higher risk of all-cause death (19.8% vs 30.1%; HR: 1.55, 95% CI: 1.12-2.14; p=0.007), whereas following CABG, mortality was similar in patients with or without bifurcation lesion(s) (23.3% vs 23.0%; adjusted HR: 0.81, 95% CI: 0.59-1.12; p=0.207). There was a significant interaction between bifurcation lesion(s) and the treatment effect of PCI versus CABG on mortality (p for interaction =0.006). Of note, a landmark analysis in patients with bifurcation lesions treated with PCI, shows a continuous and significant divergence of cumulative mortality beyond 5-year (Figure 1).
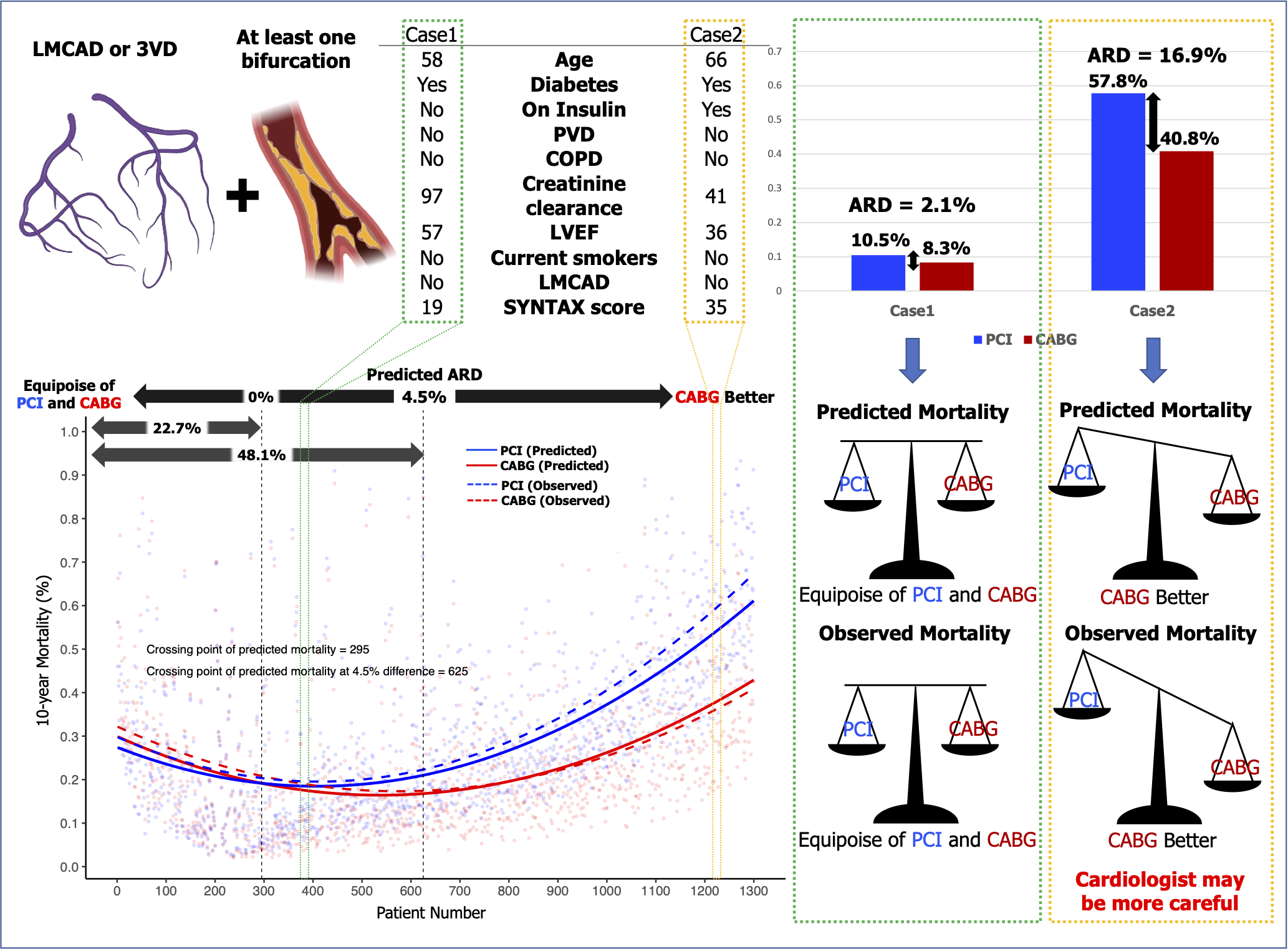
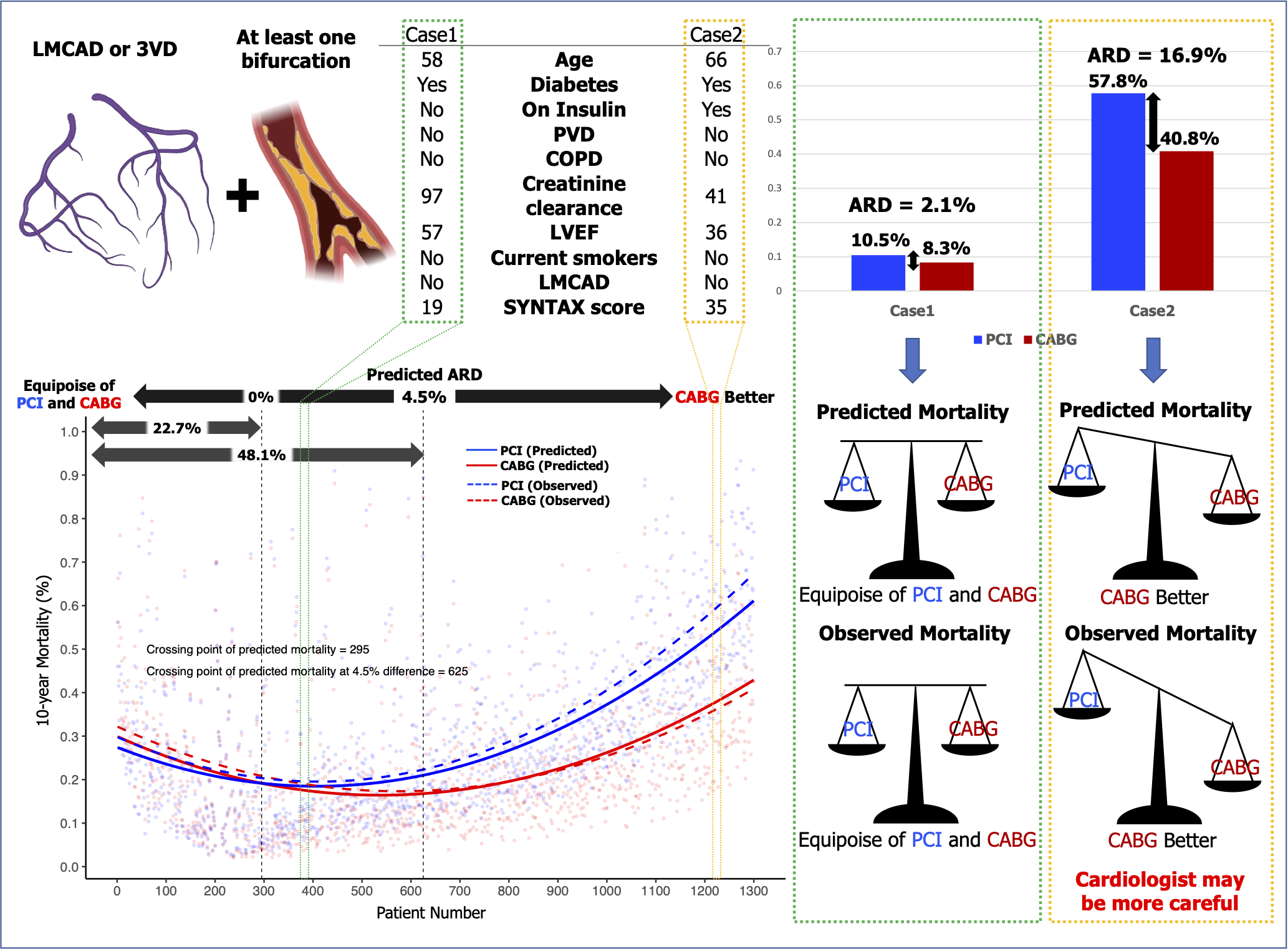
Conclusion
Bifurcation lesion(s) require specific consideration by the Heart team when deciding between PCI and CABG, as a consequence of their higher associated all-cause mortality following PCI. Notwithstanding this, the average treatment effect can be mitigated by calculating an individualized 10-year vital prognosis using the SSII-2020.


