Lots of interesting abstracts and cases were submitted for TCTAP 2022. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-067
Elevated C-Reactive Protein/Albumin Ratio Is Associated With Lesion Complexity, Multilevel Involvement, and Adverse Outcomes in Patients With Peripheral Artery Disease
By Byung Gyu Kim, Jongkwon Seo, Gwang Sil Kim, Moo-Nyun Jin, Hye Young Lee, Young Sup Byun, Byung Ok Kim
Presenter
Byung Gyu Kim
Authors
Byung Gyu Kim1, Jongkwon Seo1, Gwang Sil Kim, Moo-Nyun Jin1, Hye Young Lee1, Young Sup Byun1, Byung Ok Kim2
Affiliation
Inje University Sanggye Paik Hospital, Korea (Republic of)1, Veterans Health Service Medical Center, Korea (Republic of)2
View Study Report
TCTAP A-067
Peripheral Vascular Disease and Intervention
Elevated C-Reactive Protein/Albumin Ratio Is Associated With Lesion Complexity, Multilevel Involvement, and Adverse Outcomes in Patients With Peripheral Artery Disease
Byung Gyu Kim1, Jongkwon Seo1, Gwang Sil Kim, Moo-Nyun Jin1, Hye Young Lee1, Young Sup Byun1, Byung Ok Kim2
Inje University Sanggye Paik Hospital, Korea (Republic of)1, Veterans Health Service Medical Center, Korea (Republic of)2
Background
The inflammatory process and malnutrition play important roles in the pathogenesis and progression of atherosclerosis. C-reactive protein (CRP) is a commonly used clinical inflammatory marker in routine preprocedural blood tests that correlate with both disease severity and prognosis in patients with coronary artery disease. Serum albumin is expressed as a negative acute-phase protein and inversely correlated with the severity of the inflammatory response and reflects the nutritional status. Several studies regarding the clinical outcomes of cardiovascular disease have suggested that the CRP-to-albumin ratio (CAR), a simple value that reflects the balance between systemic inflammation and malnutrition, can be a novel indicator to predict disease progression and patients’ outcome. However, the relationship between CAR and the disease burden and the long-term clinical outcomes of patients with peripheral artery disease (PAD) after endovascular therapy (EVT) has not been well elucidated. Thus, the aim of this study was to evaluate the prognostic value of CAR in predicting the prevalence of complex lesions and multilevel involvement in patients with PAD treated with EVT. The secondary aim was to evaluate the association between CAR and clinical outcomes after EVT.
Methods
A total of 307 patients with PAD who underwent EVTwere retrospectively reviewed and categorized according to CAR tertiles; 1sttertile, 0.022‒0.029; 2nd tertile, 0.030‒0.628; and 3rdtertile, 0.629‒13.917. The groups were compared for the prevalence of complex lesions and multilevel involvement as well as the incidence of major adverse cardiovascular events(MACEs) and major adverse limb events (MALEs). TASC type C or D lesions were considered as complex lesions. Multileveldisease was defined by the presence of severe disease in more than one categorical region (aortoiliac, femoropopliteal, or infrapopliteal) in the same limb.
Results
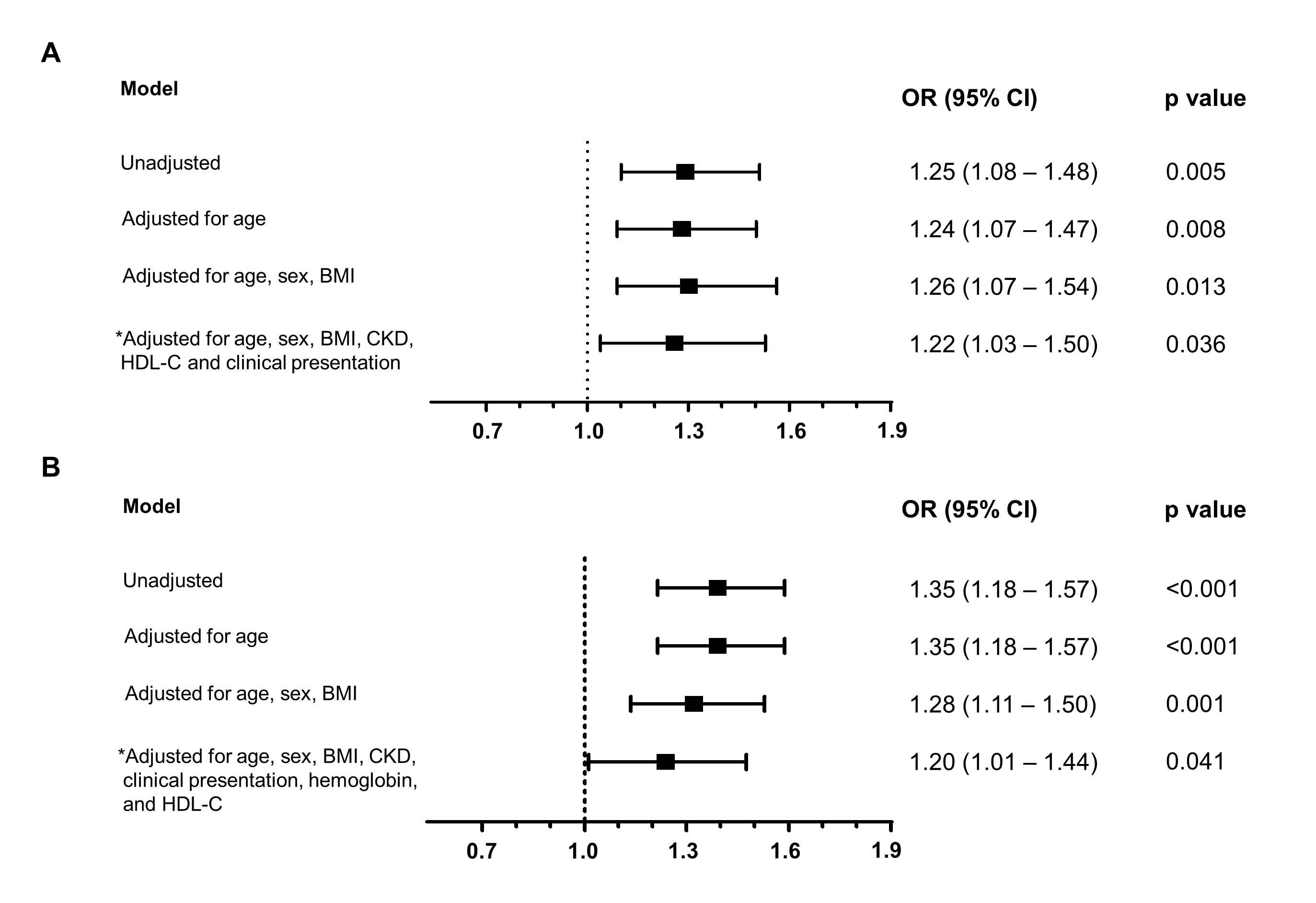
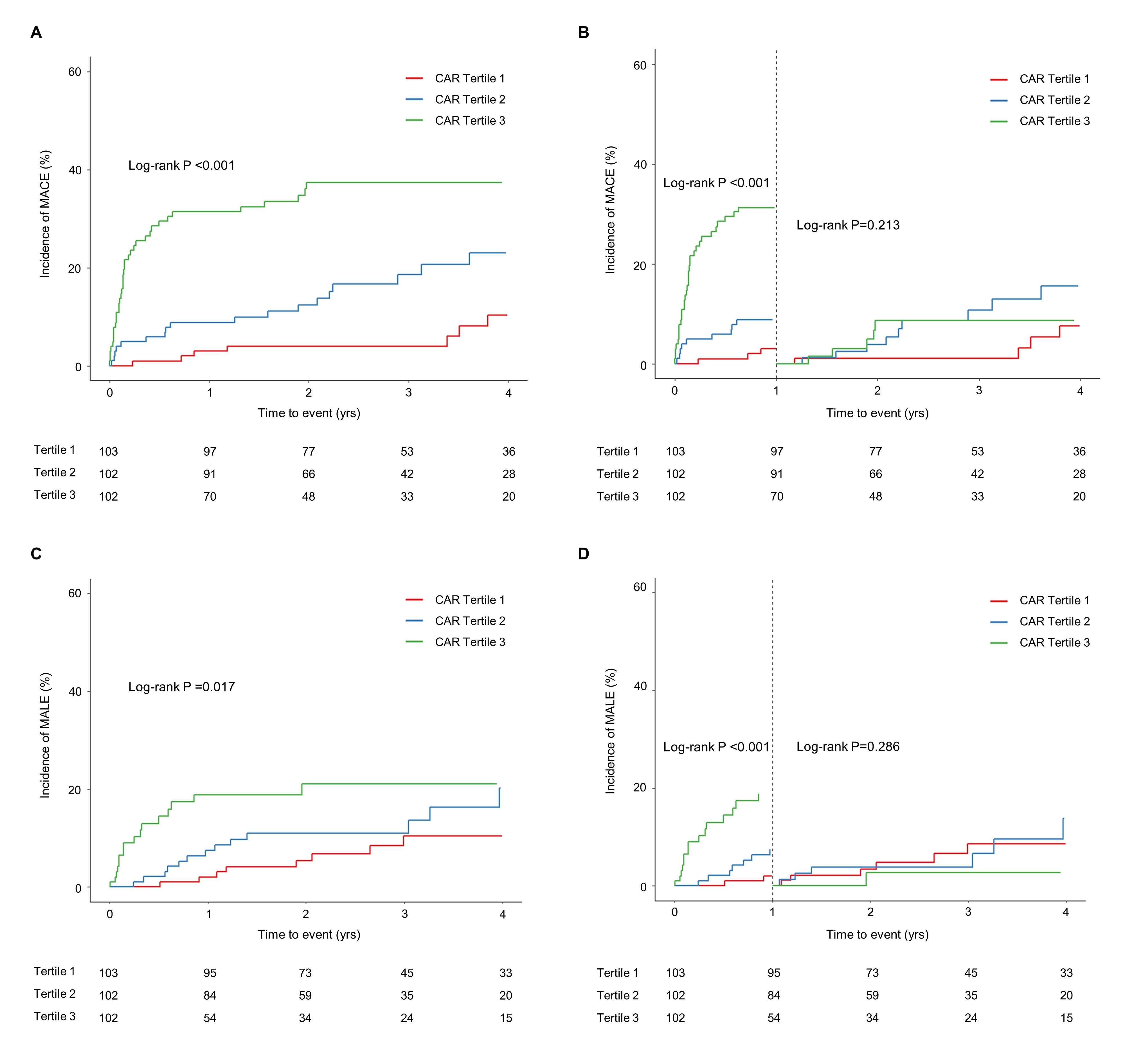
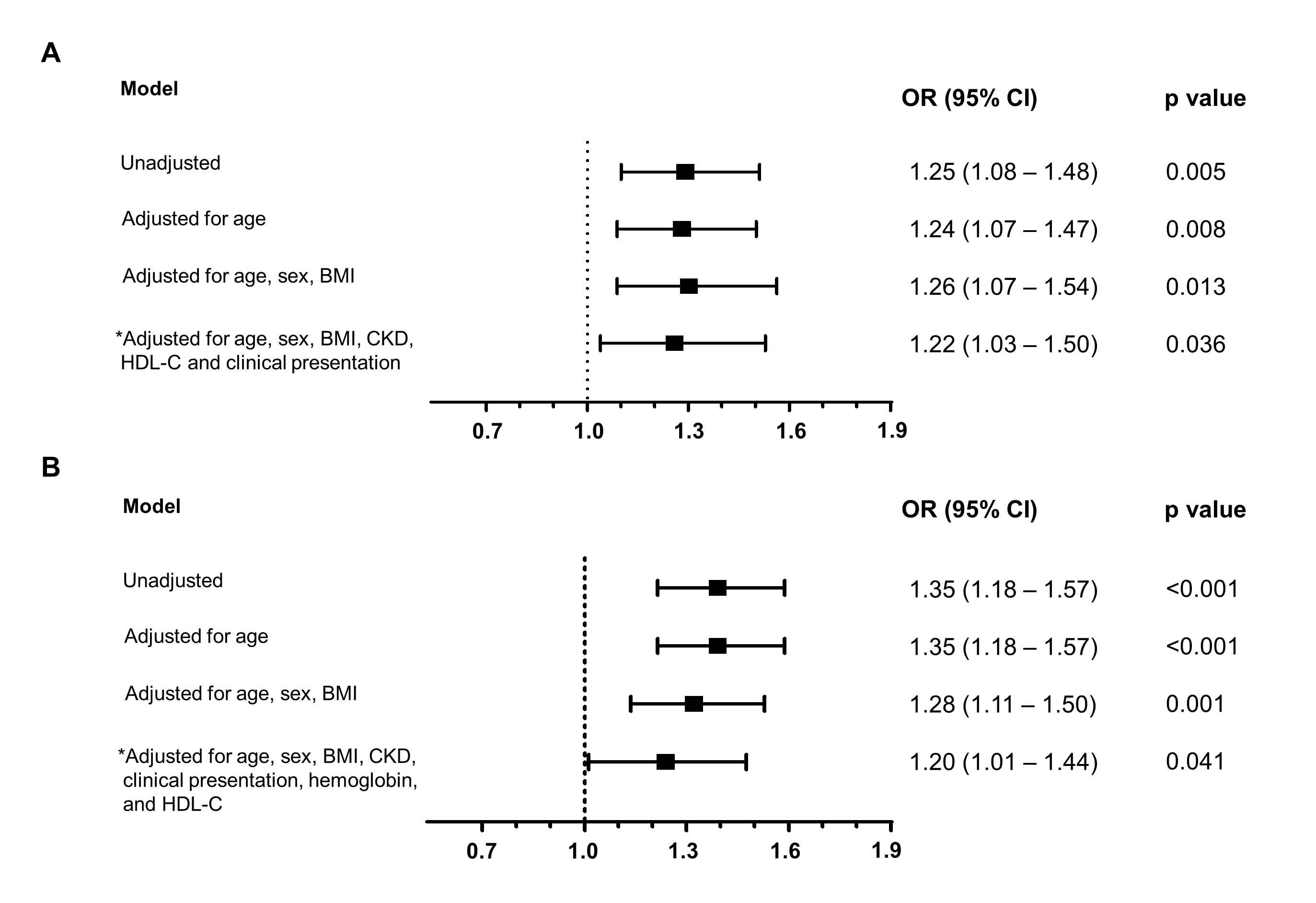
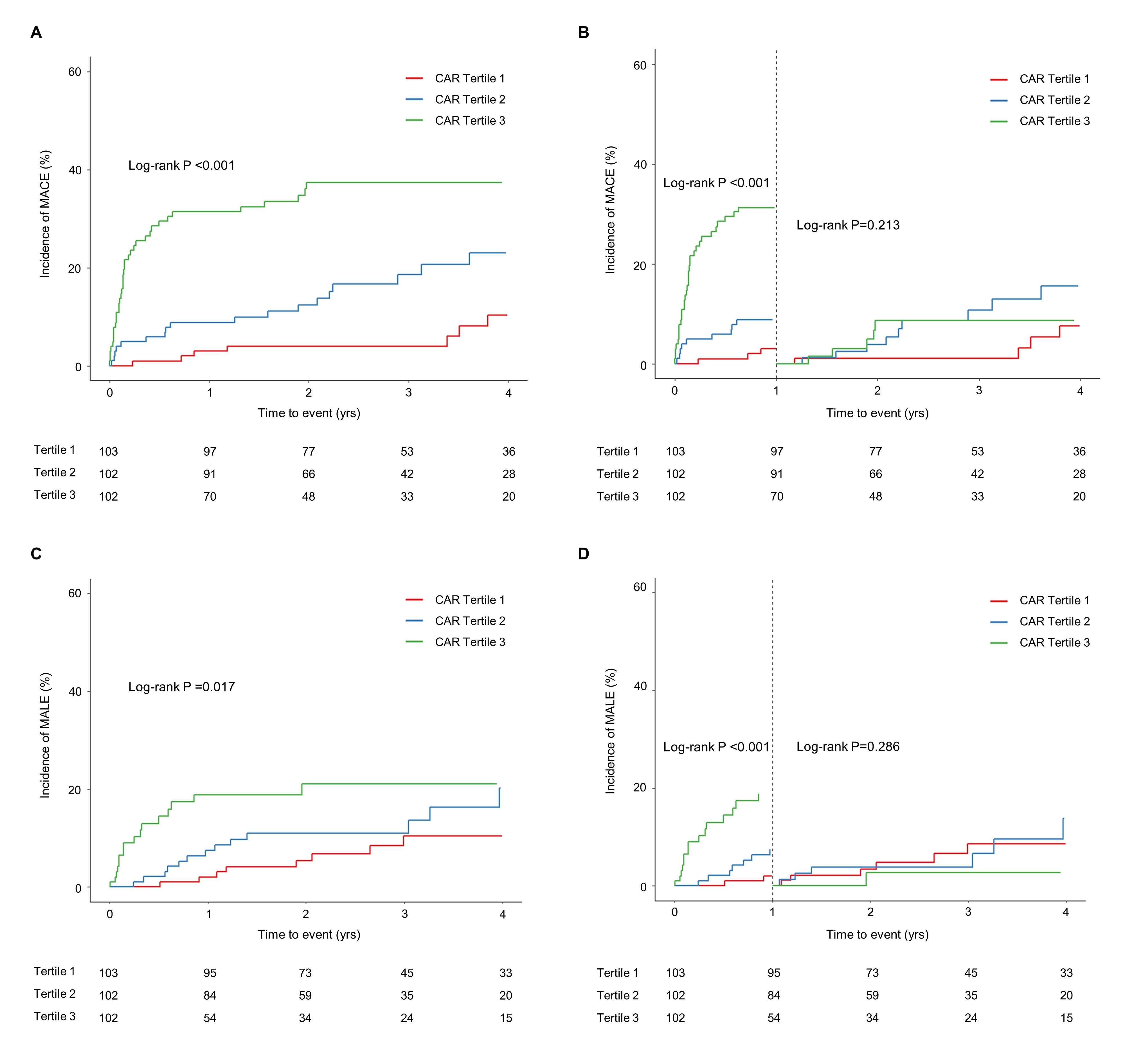
The rates of complex lesions and multilevel involvement increased with increasing CAR tertiles (all p<0.001). These associations remained significant even after adjustment for other confounders(complex lesion odds ratio, 1.22 [1.03‒1.50], p=0.036; multilevel disease odds ratio, 1.20 [1.01‒1.44],p=0.041) (Figure 1). The third tertile of the CAR group showed a significantly higher incidence of MACEs and MALEs than the second and first tertile within a year (log-rank p<0.001) (Figure 2). A higher CAR as a continuous variable was also independently associated with the 4-year rate of MACE (hazard ratio, 1.20 [1.04‒1.38], p=0.015).
Conclusion
In conclusion, CAR, a novel marker of the inflammatory state measured in routine biochemical assessments, conveys valuable prognostic information that is independent of other conventional clinical risk factors in patients with PAD. Therefore, the high inflammatory conditions indicated by an elevated CAR should be considered as a risk factor for advanced disease and future MACEs in patients with PAD. Proper preventive strategies to reduce adverse events in these patients should be established in the future.


