Lots of interesting abstracts and cases were submitted for TCTAP 2022. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-071
Role of Serum N-6 Polyunsaturated Fatty Acids in the Development of Acute Coronary Syndromes
By Naoya Inoue, Shuji Morikawa
Presenter
Naoya Inoue
Authors
Naoya Inoue1, Shuji Morikawa1
Affiliation
Chutoen General Medical Center, Japan1
View Study Report
TCTAP A-071
Pharmacology/Pharmacotherapy
Role of Serum N-6 Polyunsaturated Fatty Acids in the Development of Acute Coronary Syndromes
Naoya Inoue1, Shuji Morikawa1
Chutoen General Medical Center, Japan1
Background
Methods
Patient population
Results
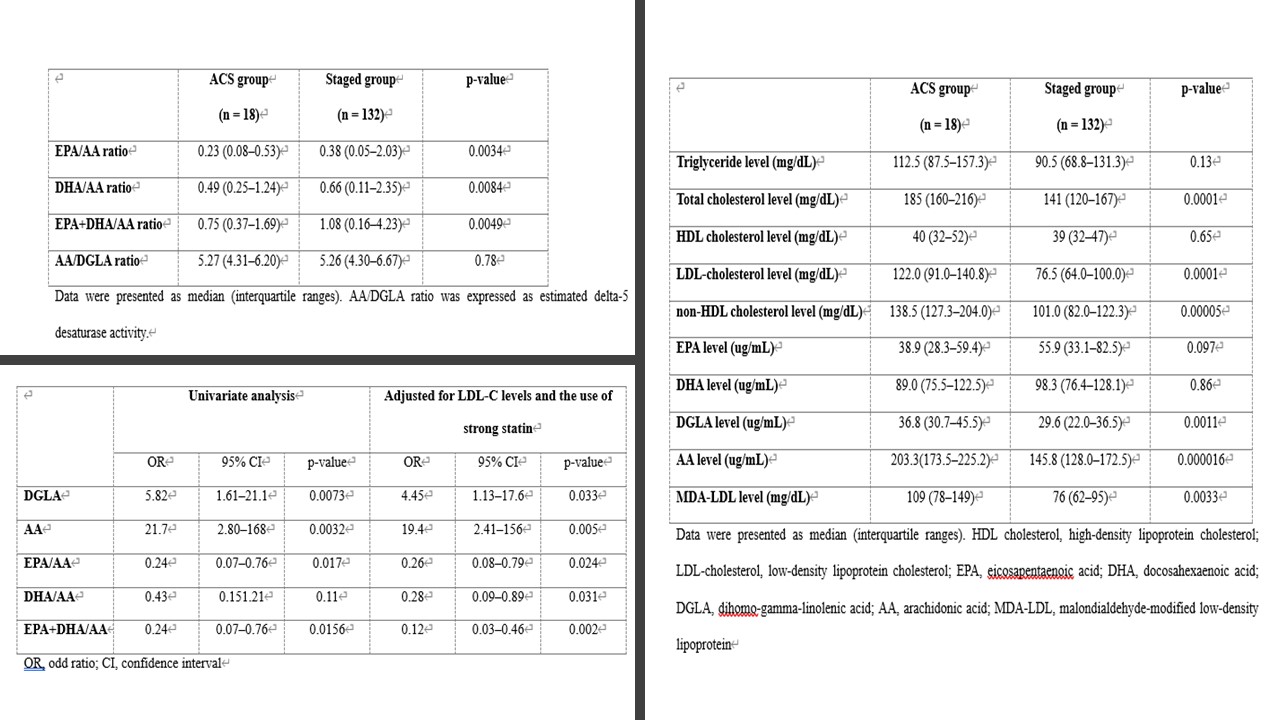
Comparison of each lipid and PUFAs levels in the staged and ACS groups
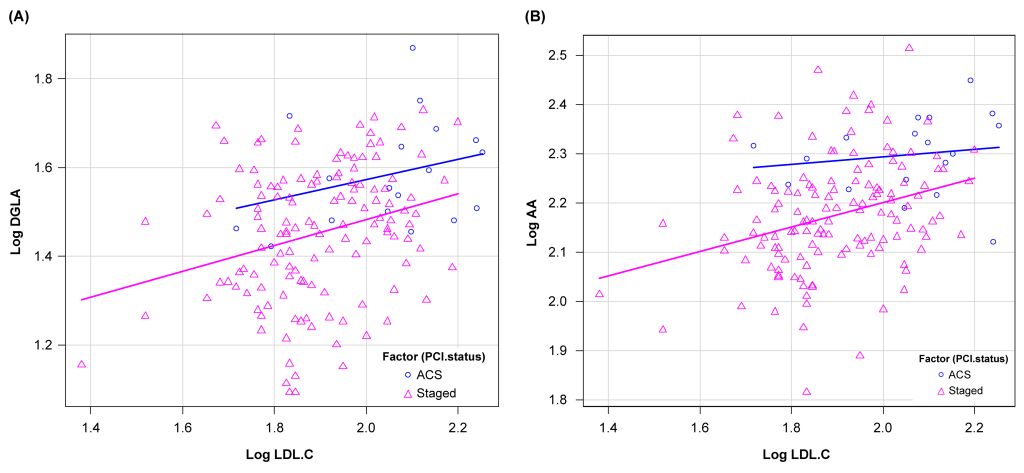
Effect of DGLA and AA on ACS with consideration of the difference in LDL-C levels and the use of strong statinsWe performed ANCOVA to analyze the effect of DGLA and AA on the development of ACS, with consideration of the difference in LDL-C levels (FIG2). Results showed statistically significant differences in DGLA and AA levels between the two groups based on ANCOVA adjusted for LDL-C levels (DGLA: p=0.022, AA: p=0.0028).
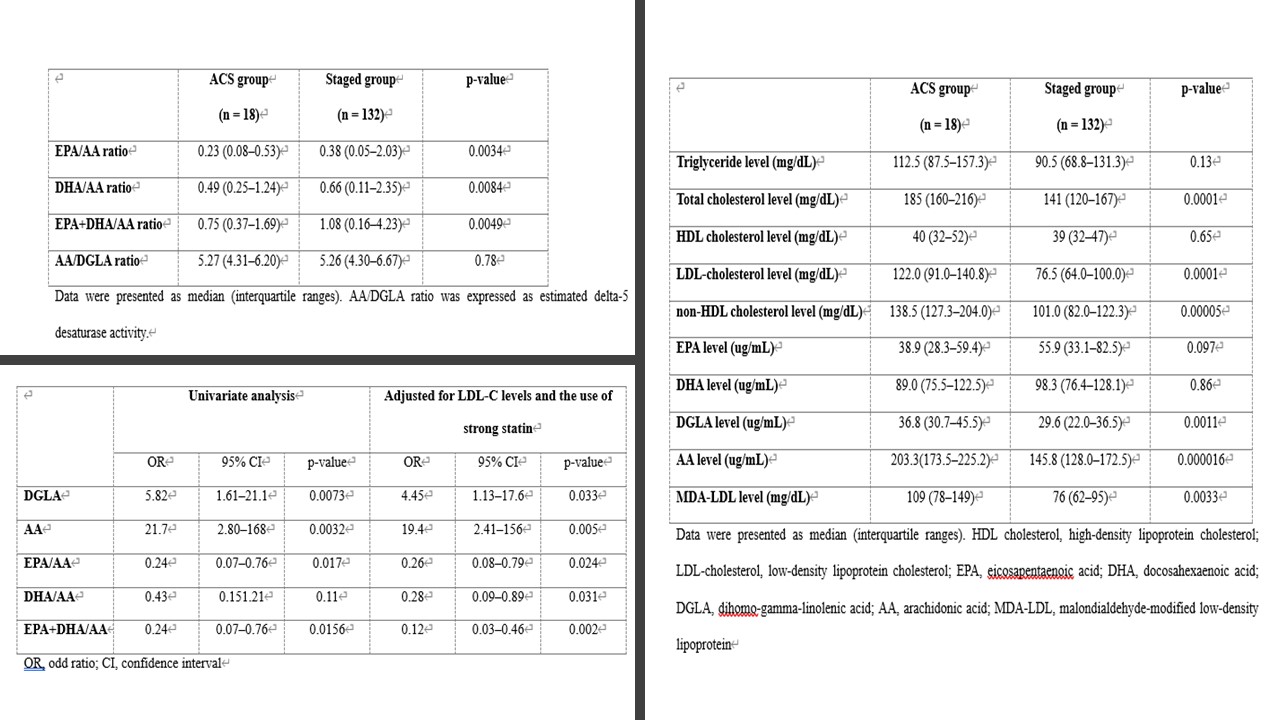
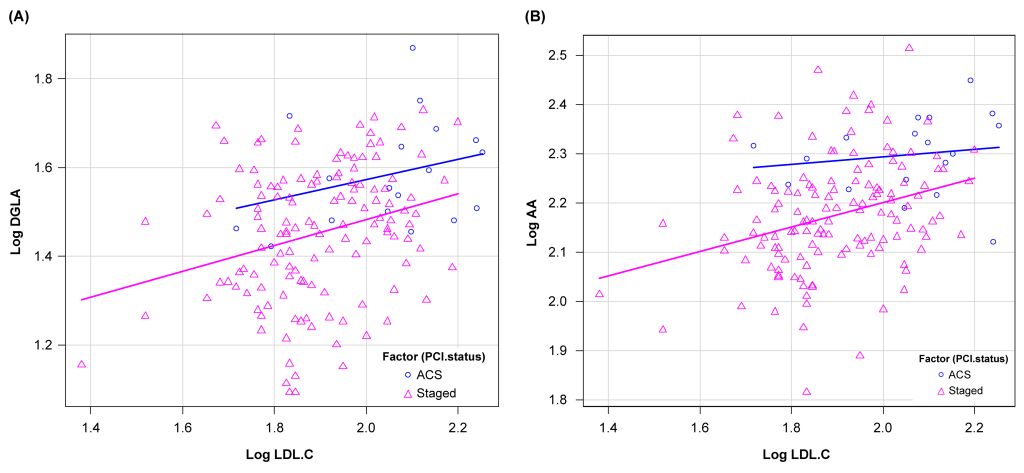
Effect of DGLA and AA on ACS with consideration of the difference in LDL-C levels and the use of strong statinsWe performed ANCOVA to analyze the effect of DGLA and AA on the development of ACS, with consideration of the difference in LDL-C levels (FIG2). Results showed statistically significant differences in DGLA and AA levels between the two groups based on ANCOVA adjusted for LDL-C levels (DGLA: p=0.022, AA: p=0.0028).
Conclusion
The ACS group had significantly higher AA and DGLA levels than the staged group. This result was consistent even after adjusting for the effects of confounding factors such as use of strong statins and LDL-C levels. Therefore, excess serum n-6 PUFAs levels may be a risk factor for the development of ACS. In addition, supplementation with n-3 PUFAs may not be necessary for the prevention of ACS.


