The East Asian Paradox - a term coined by Young-Hoon Jeong, MD (Changwon Gyeongsang National University Hospital, South Korea) in 2012 - is growing in importance with the development of potent antiplatelet agents.
These potent antiplatelet agents are used frequently in acute coronary syndromes (ACS) patients after percutaneous coronary intervention (PCI) with direct oral anticoagulants (DOAC), which are essential for the management in patients with atrial fibrillation.
 At TCTAP 2021 Virtual, Glenn N. Levine (Baylor College of Medicine, Texas, USA) presented insights on antithrombotic therapy in East Asians with ACS and undergoing PCI. Levine was a member of an international group that systematically looked at the concept of the East Asian paradox in patients with ACS or undergoing PCI.
At TCTAP 2021 Virtual, Glenn N. Levine (Baylor College of Medicine, Texas, USA) presented insights on antithrombotic therapy in East Asians with ACS and undergoing PCI. Levine was a member of an international group that systematically looked at the concept of the East Asian paradox in patients with ACS or undergoing PCI.
East Asians have a higher prevalence of CYP2C19 loss of function alleles (East Asians 60% vs. whites 30%) leading to high on-treatment platelet reactivity (HTPR). Furthermore, East Asians demonstrate 30 to 47 percent higher degree of platelet inhibition with prasugrel and up to 40 percent higher degree of platelet inhibition with ticagrelor compared to whites at any given dose. The prasugrel 5mg dose seemed to confer the same degree of platelet inhibition as the standard 10mg dose in East Asians.
The East Asian “paradox” refers to (1) similar or lower incident of stent thrombosis compared to Caucasian patients despite HTPR on clopidogrel and (2) the fact that East Asians are at greater risk of bleeding. East Asians have an increased risk of intracranial hemorrhage (ICH) on warfarin compared to Caucasians, despite a similar INR, and some studies also report an increased risk of bleeding on the same doses of DAPT.
Levine explained that the East Asian paradox is probably multifactorial, including hemostatic and thrombotic differences pertaining to hemostatic factors, endothelial function activation, and pharmacokinetic/pharmacodynamics aspects. Pharmacokinetic/pharmacodynamics considerations include smaller body size and lower BMI, differences in drug metabolism, and relatively lower renal clearance of drugs in East Asians.
Levine discussed the therapeutic window of antiplatelet therapy, which is bound by low on-treatment platelet reactivity (LPR) below which bleeding predominates, and high on-treatment platelet reactivity (HPR), above which thrombotic events prevail.
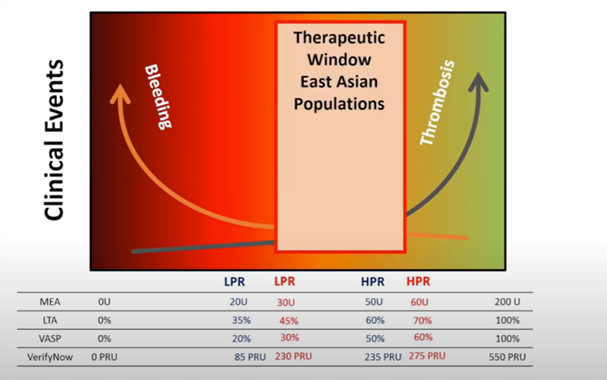
This window is different for East Asians, indicating a shift to the right. Namely, East Asians are “therapeutic” at higher LPR and HPR because of the increased risk of bleeding and lower risk of thrombotic events, respectively.
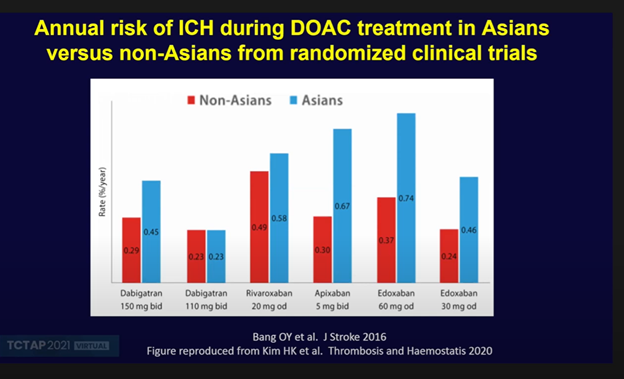
Over the last decade, data has emerged to suggest that this East Asian paradox extends to DOACs also, with East Asians and Caucasians differing significantly in their response to antithrombotic agents. The annual risk of ICH with DOAC therapy appears to be much higher in East Asians at the same DOAC dose.
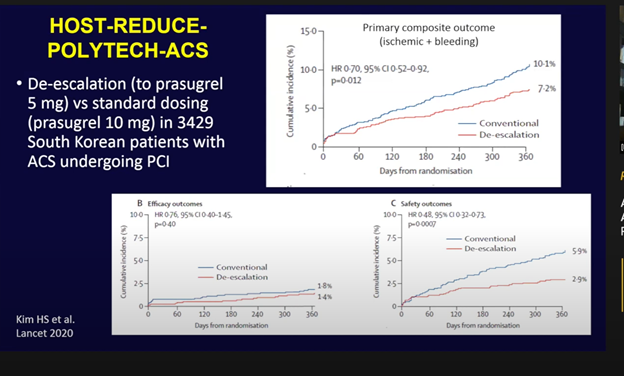
Furthermore, in the HOST-REDUCE-POLYTECH-ACS trial, de-escalation of prasugrel from 10mg to 5mg in 3,000 South Korean patients with ACS undergoing PCI resulted in significantly lower bleeding with no increase in ischemic endpoints.
These concepts were recently iterated in a position statement document published last year, which emphasized the different therapeutic windows for inhibition of platelet P2Y12 receptors and DOACs
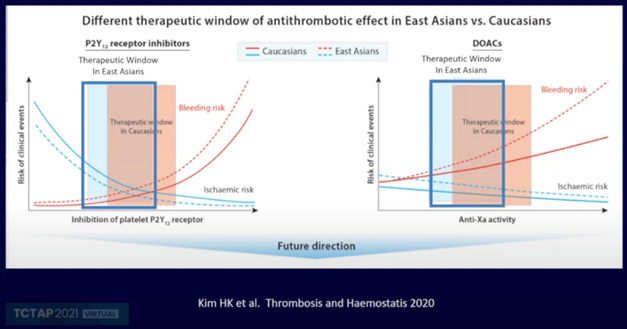
“Since data, trial results, dosing, and recommendations from U.S. and European population studies influence guideline recommendations, they should not necessarily be directly extrapolated to East Asian populations, Levine said. “Ultimately, tailored or personalized therapy in East Asians, particularly dosing continues to be advisable.”
Editor: Chang Hoon Lee, MD (VHS Medical Center, Korea (Republic of))
Edited by
Chang Hoon Lee, MD
VHS Medical Center, Korea (Republic of)


