Radiation injury in interventional cardiology is largely overlooked since most interventional procedures in the lab do not exceed the threshold radiation dose that causes harm.
But for interventionists who perform complex PCI procedures - especially on CTO patients wherein the procedure duration is prolonged - management of radiation dose is crucial for preventing serious radiation injury both to the patient and the operating staff.
During the Hot Topic session on CTO held at TCTAP 2021 Virtual, the second session was dedicated to “The Quest for Safety” in CTO-PCI.
 Gerald Werner, MD, PhD (Klinikum Darmstadt, Germany) spoke about the topic of radiation safety, adding to the previous two talks on management of anti-thrombotic and coronary perforation in CTO.
Gerald Werner, MD, PhD (Klinikum Darmstadt, Germany) spoke about the topic of radiation safety, adding to the previous two talks on management of anti-thrombotic and coronary perforation in CTO.
“Radiation injury is one of the few avoidable complications of complex PCI in general, and especially in CTO-PCI,” Werner said. “But radiation safety doesn’t get enough attention because radiation injury is rarely reported in studies, and they occur days or even weeks after the initial procedure.”
Radiation skin injury is dose-dependent and occurs when certain threshold dose (Gy) is exceeded. With different amounts of exposure, the types of skin injury could range from transient erythema (2 Gy), permanent epilation (7 Gy), dry desquamation (14 Gy) or dermal necrosis (18 Gy).
Werner paralleled the radiation dose rate to the speed of a car. Akin to a driver who needs to keep an eye on the speedometer of the car to be safe, complex PCI operators need to know the dose rate (Gy/s) during the procedure, which is shown instantaneously on the angiography machines.
Studies published over the years have shown that patient radiation exposure (Air Kerma, Gy) decreased from 10 Gy to about 2 Gy. Despite the progress, Werner pointed out more room for improvement.
Radiation exposure is also related to the complexity of the PCI procedure. In 2017, Werner and his team found that the Air Kerma was 2.1 Gy, 2.7 Gy and 3.5 Gy for J-CTO score of 0-1, 2-3, and 4-5, respectively, but also noted individual variability in radiation procedures due to individual practice.
In a recently published paper, Werner’s team compared the median fluoroscopy time of different operators and Air Kerma at two different years (2012 and 2017).
Results showed that although there was overall improvement in reducing the median Air Kerma between the two periods, there was a large variation of median Air Kerma between operators even though median fluoroscopy time was similar.
“Improvement in managing radiation exposure can be achieved through continuous discussion and education on radiation safety during live cases and CTO courses,” Werner said.
Several ways to reduce radiation exposure for a given procedure were suggested, including lowering the fluoroscopy rate from 15 fps to 7.5 fps as the easiest method. The lowering of the fluoroscopy rate, while reducing the fluoroscopy exposure, leaves the total radiation time at a high level due to a larger contribution to the total dose by cine runs.
Secondly, further reduction of cine runs to 7.5 fps will cut down total dose significantly in suitable patients, Werner said.
Thirdly, reducing the number of cine runs as much as possible and using fluoroscopy storage to record important procedure steps rather than cine recording was also stressed.
Finally, changing the angulation of working views could also reduce the dose rate. For example, when working on RCA, changing from LAO 450 to LAO 300 will cut down the dose rate by nearly 30 percent.
“The rule of “as low as reasonably achievable” - or ALARA - should be applied from the beginning to the end of the procedure, Werner said.
Werner’s approach to radiation management for complex PCI was to use cine runs of 15 fps only for the initial bilateral imaging to visualize the collaterals and only in potential using retrograde approach. The cine run will be halved at 7.5 fps and the lowest fluoroscopy protocol is used for the rest of the procedure. Werner used fluoroscopy storage and low radiation angulation for visualizing and storing balloons or stents movement in the vessel.
Modern angiography machines come with low radiation exposure features, but not every lab can afford to change or upgrade their machines frequently.
With newly published data, Werner noted a large disparity in dose rate index amongst individuals who use the same machines from different manufacturers. One particular machine that stands out is Philips Clarity which limits the outliers amongst the operators. By using the same machines and new radiation protocol, Werner reported in his paper that the Air Kerma had been slashed by nearly 75 percent over 10 years, initially by reducing the fluoroscopy frame rate and later by reducing the number of required cine runs.
Before the new radiation protocol, 10.4 percent of their patients exceeded Air Kerma of 5 Gy, which is the threshold for causing radiation damage. The 5 Gy threshold was never exceeded after the new radiation protocol was introduced, even with patients with BMI >30, or when procedure fluoroscopy time was more than 120 minutes. Similarly, maximum skin entry dose (mGy) rarely exceeded the threshold of 2 Gy after the new radiation protocol.
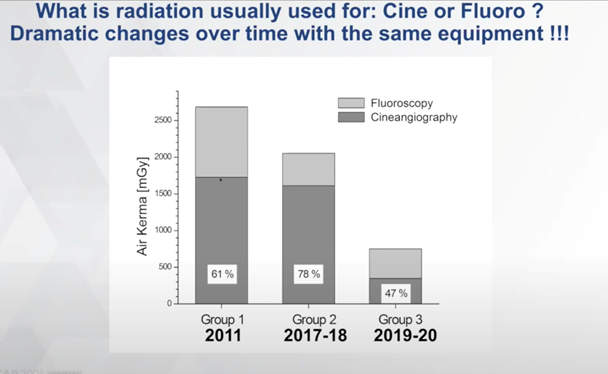
Werner noted that, “The latest and biggest steps we achieved was reducing cine angiography by three times. This brought us to an average Air Kerma in our CTO procedures to the lowest-reported 700 mGy.”
One significant advantage of reducing radiation dose exposure to patients is a decrease in occupational exposure for the operators and cath lab staffs.
Although acknowledging concerns that scatter dose at C-arm may increase during low-dose protocol, Werner pointed out that these low-dose scatter are negligible when using modern shielding technique.
For occupation protection for operators, Werner mentioned Biotronik‘s suspended radiation protection system, Zero-Gravity, - wherein operators are protected from both radiation and back injury due to the weight of the lead apron. He was also enthusiastic about the new Rampart IC M1128 shielding system, a full-bodied radiation protection where operators can work without the individual lead apron.
Werner concluded that in his practice, radiation is no longer the reason for abandoning a procedure.
“It is true that most interventionist still do not understand how to optimize the radiation exposure dose for both patients and themselves,” he said. “This is mainly because most do not realize their machines are better than they believe, and by tweaking the angiography machines’ settings, the total radiation exposure dose could be significantly reduced without upgrading to a new machine.”
“The ultimate wish for CTO operators is to have an effective lead shielding system that can reduce radiation to patients and themselves and also can get rid of the personal lead apron to work in just scrubs to reduce back injury,” Werner added.
Edited by

Aaron Sung Lung Wong, MD
National Heart Centre Singapore, Singapore


