Lots of interesting abstracts and cases were submitted for TCTAP 2021 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don’t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
TCTAP C-102
Presenter
Hehe Cui
Authors
Hehe Cui, Li Zhou3, Hui Chen3
Affiliation
, Beijing Friendship Hospital, China3,
View Study Report
TCTAP C-102
IMAGING AND PHYSIOLOGIC LESION ASSESSMENT - Physiologic Lesion Assessment
Combining Fractional Flow Reserve and Optical Coherence Tomography Guided Percutaneous Coronary Intervention in Two-vessel Intermediate Coronary Artery Lesions
Hehe Cui, Li Zhou3, Hui Chen3
, Beijing Friendship Hospital, China3,
Clinical Information
Patient initials or Identifier Number
ZZP/00135618
Relevant Clinical History and Physical Exam
A 60-year-old man was hospitalized because of paroxysmal chest pain during cooking three days before. The retrosternal burning pain last about five minutes and was relieved automatically. He had no history of hypertension, dyslipidemia or diabetes, but he had smoked for 30 years. His physical examination was unremarkable: Blood pressure 139 / 68 mmHg (right arm). Pulse 66 /minute. Body mass index 23.1 kg/m2. No positive sign in the heart and vascular system.
Relevant Test Results Prior to Catheterization
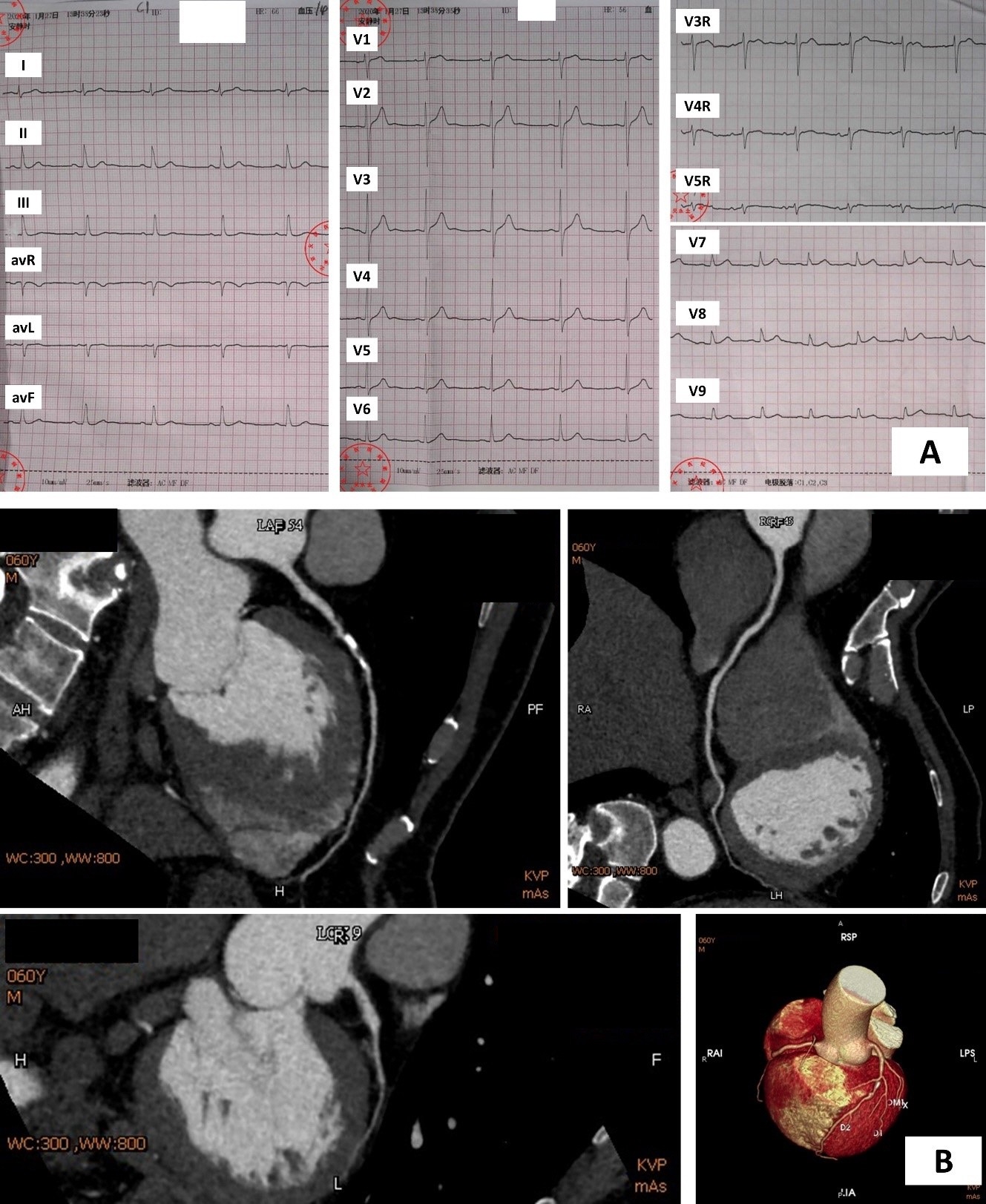
An ECG was acquired (Figure 1 A). Cardiac troponin I 0.147 ng/mL (99% URL 0.030). Total cholesterol 3.57 mmol/L, LDL-C 2.11 mmol/L. Echocardiogram showed a good ejection fraction (64%) and no wall motion abnormalities. The patient was hesitated to undergo an invasive coronary angiogram, a non-invasive coronary computed tomographic angiography (CTA) was performed and a heavily calcified plaque with unevaluable stenosis was found in the middle left descending artery (LAD) (Figure 1 B).
Relevant Catheterization Findings
To show lesions and stenosis clearly, the patient was persuaded to undergo coronary angiography (CAG). As the clips showed, The CAG demonstrated a 60% - 80% diffuse stenosis in the proximal to mid LAD, a normal left circumflex artery, an atherosclerotic plaque in the proximal right coronary artery (RCA) and a 50% - 70% stenosis in the distal RCA.
 se001.avi
se001.avi
 se005.avi
se005.avi
 se011.avi
se011.avi
Interventional Management
Procedural Step
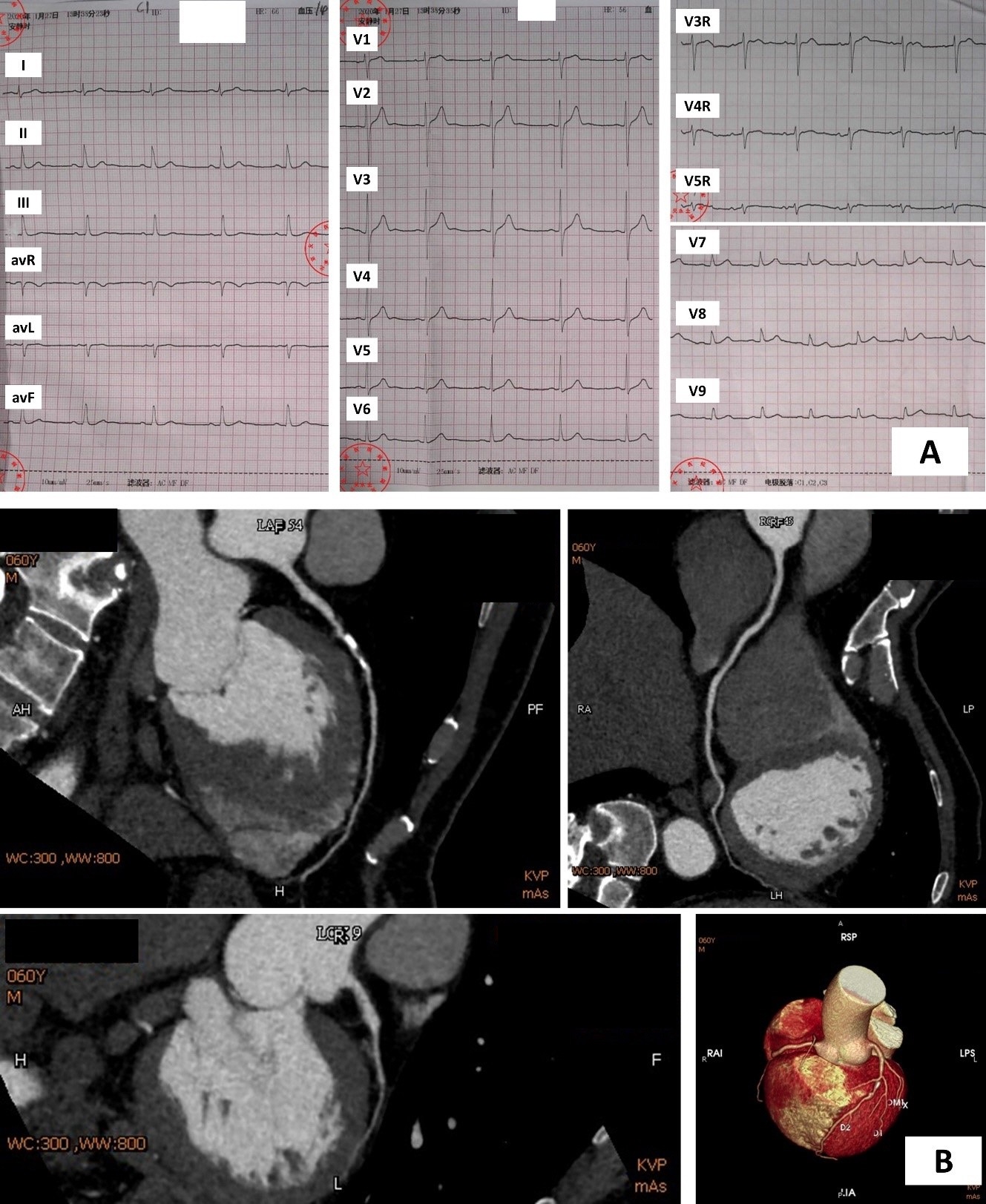
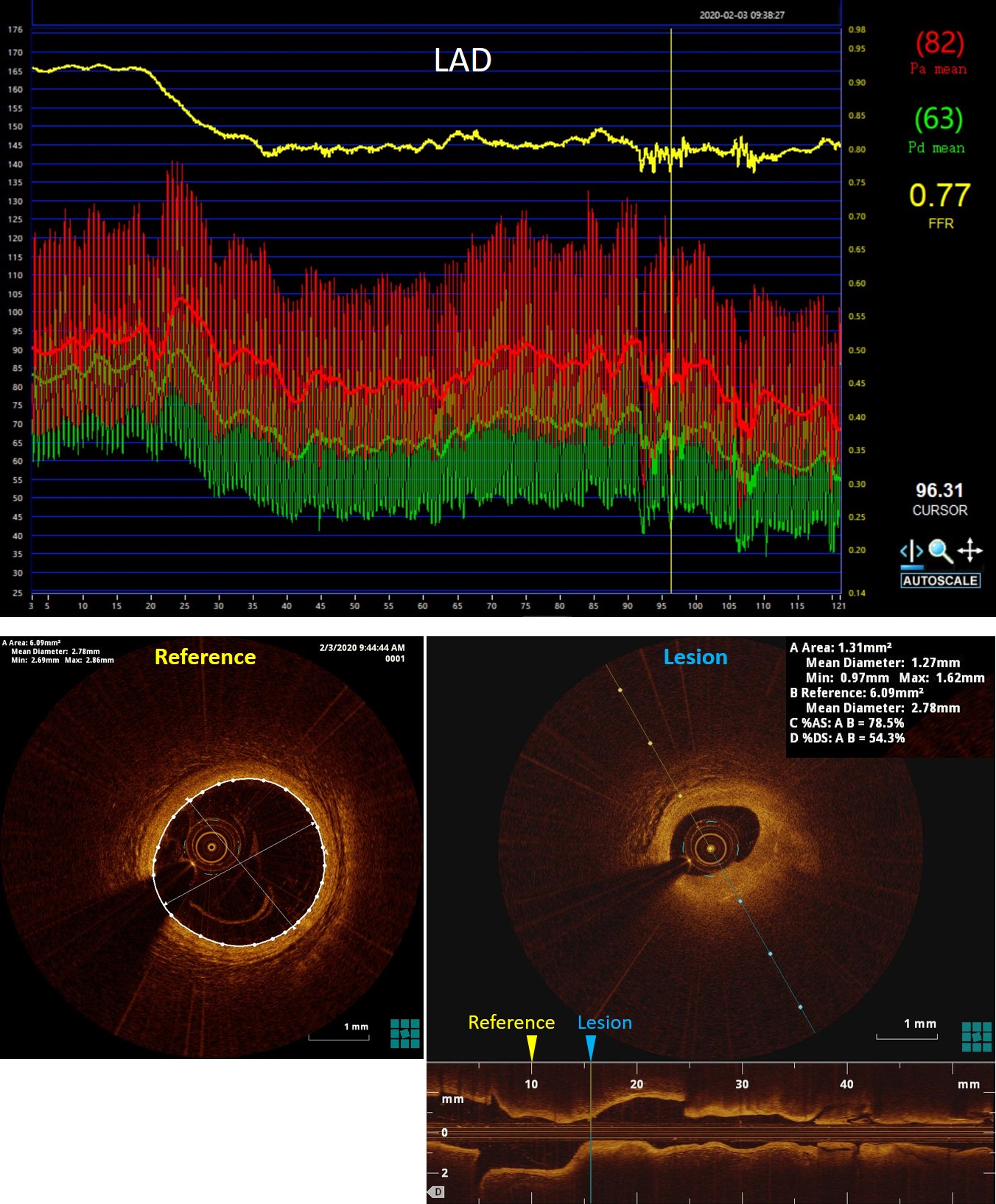
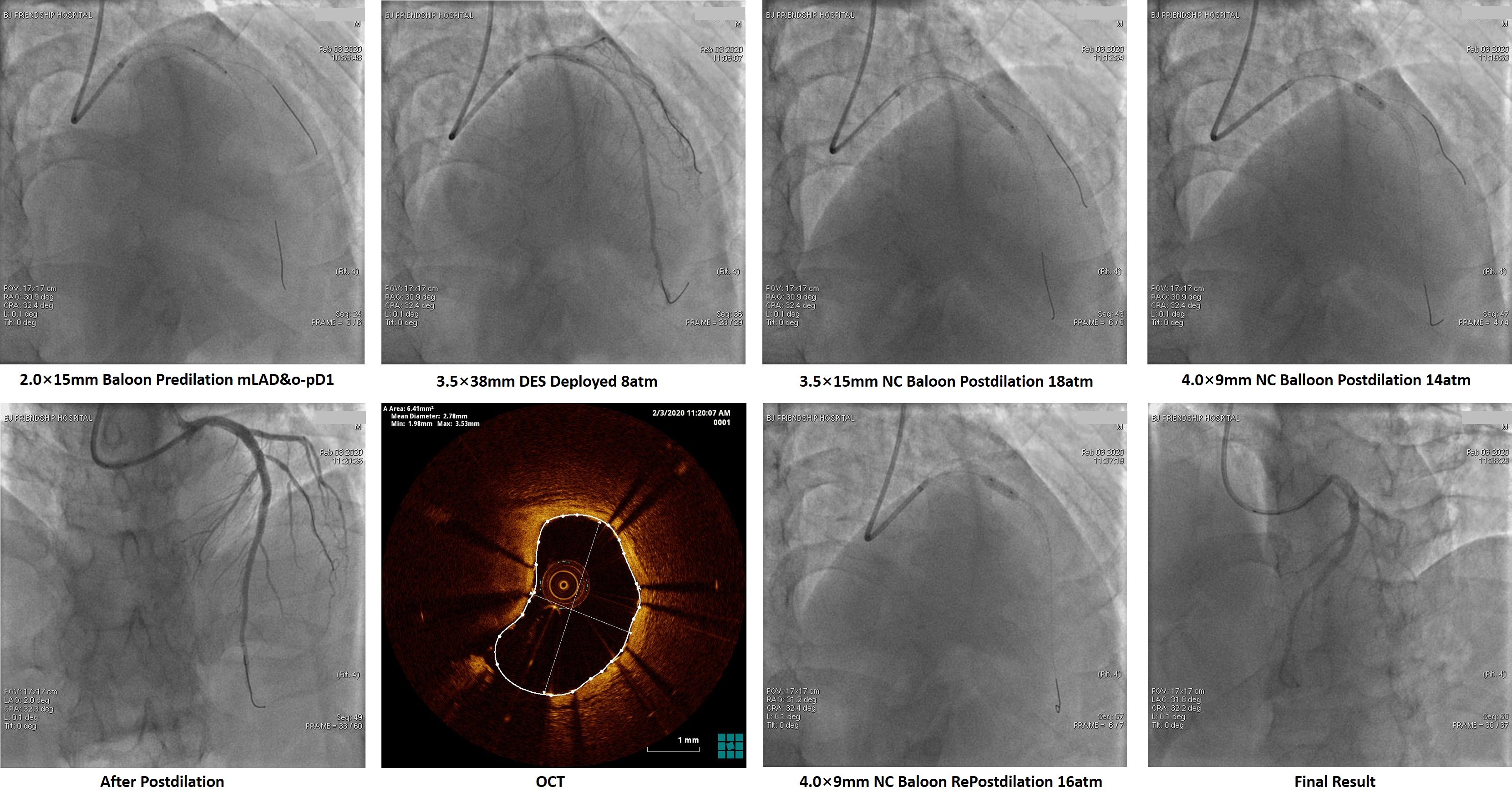
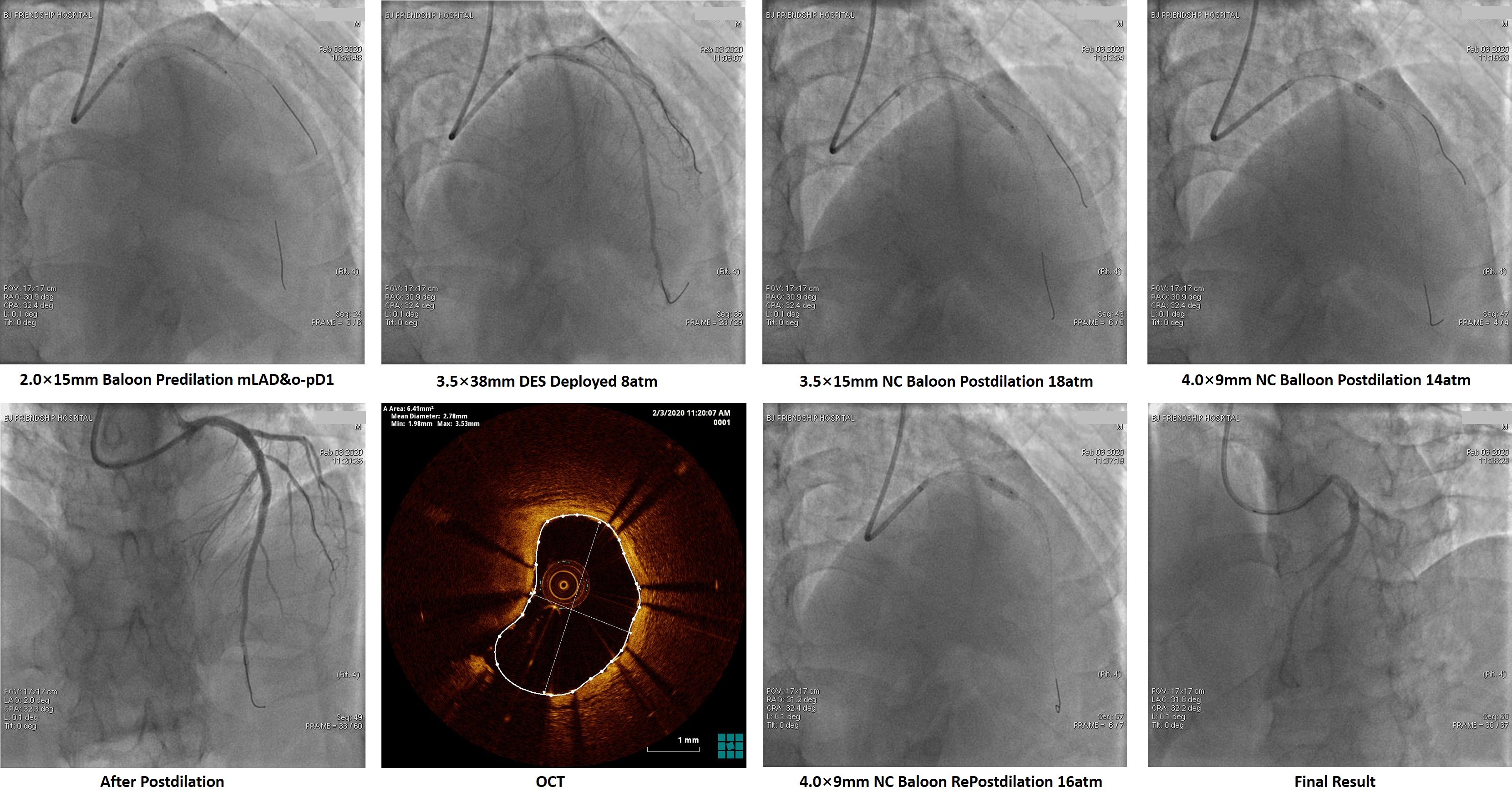
Intravascular tools were adopted to evaluate intermediate coronary lesions. The fractional flow reserve (FFR) value of the lesion in LAD was 0.77, which located in so-called grey-zone. To assess the plaque individually, We performed optical coherence tomography (OCT) and find severe stenosis (MLA = 1.31mm2), which needs further revascularization therapy. The intermediate lesion in the RCA was identified by OCT as a ruptured plaque with a little residual thrombus and intimal flap. However, OCT also demonstrated that lipid pool of the lesion was almost empty, and the residual thrombus burden was not heavy. Besides, the angiographic blood flow was graded TIMI 3, and the patient did not have any symptoms reoccurred after dual antiplatelet therapy. This evidence indicated the ruptured plaque tended to be "healing". Furthermore, FFR test got a value of 0.88. Base on above reasons, we decided to treat the RCA lesion with optimized antiplatelet therapy (ticagrelor instead of clopidogrel) rather than intervention.Then revascularization to LAD was performed, a pre-dilation balloon (2.0 × 15mm) was used in predilation at 12 - 18 atmospheric pressure. A drug-eluting-stent (3.5 × 38mm) was deployed into the proximal to mid LAD at 8 atmospheric pressure, non-compliance balloons (3.5 × 15mm, 4.0 × 9mm) were used to post-dilate the stent. OCT after stenting showed the minimum intra-stent area was 6.41mm2, and the stent was well attached.
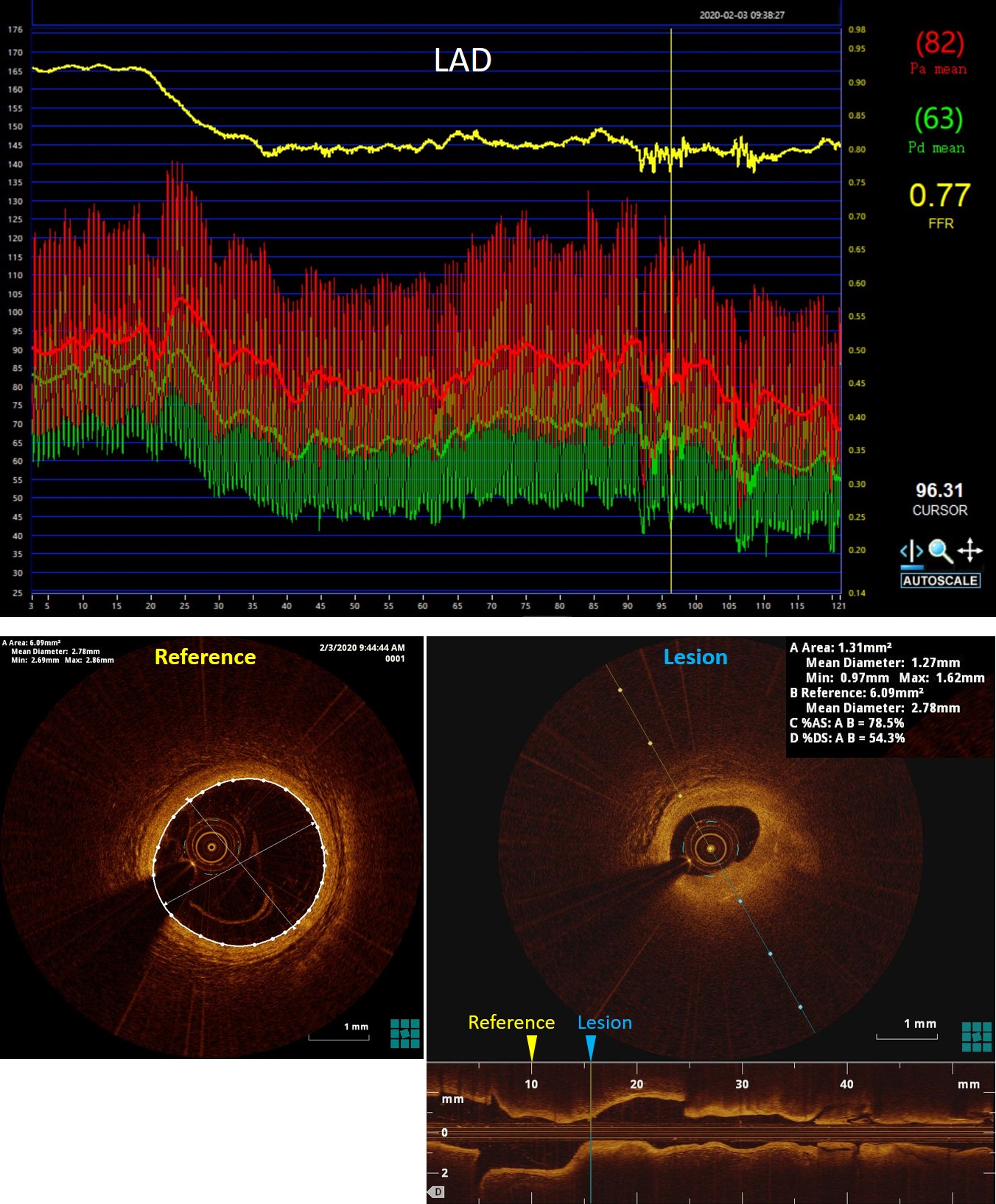
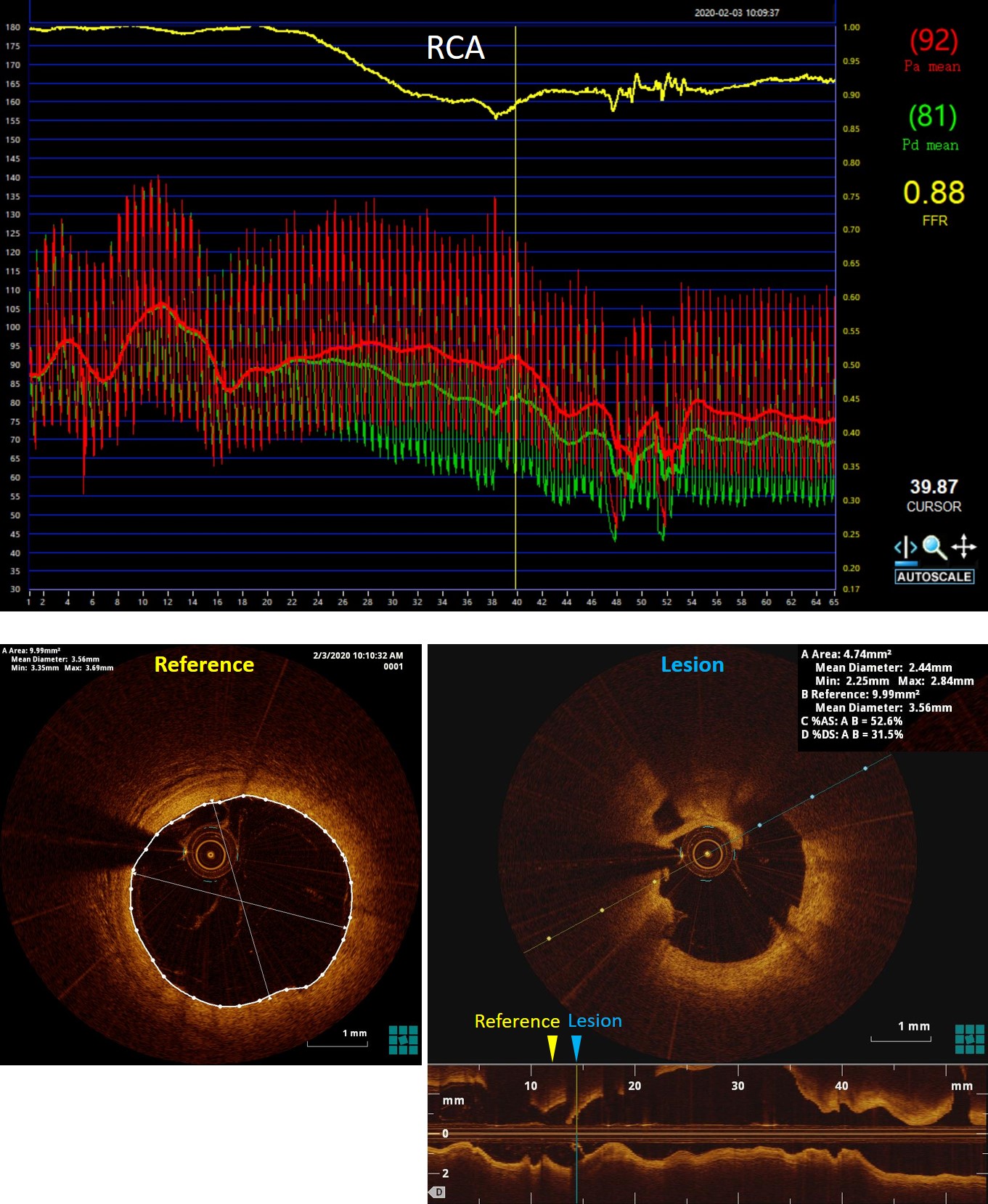
Case Summary
FFR is regarded as the gold standard for the physiological assessment of intermediate coronary artery stenosis. However, FFR does not allow assessment of plaque morphology and lesion geometry. The disadvantage could be offset by intracoronary imaging techniques such as OCT. FFR and OCT clearly answer different questions, provide complementary information, and should, therefore, not be pitched against one other. The best treatment strategy in patients with coronary heart disease will include guidance by co-registered physiology and detailed plaque morphology.


