Lots of interesting abstracts and cases were submitted for TCTAP 2021 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don’t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
TCTAP C-032
Presenter
Naoki Shibata
Authors
Naoki Shibata1, Tsuyoshi Sugiura2
Affiliation
Ogaki Municipal Hospital, Japan1, Department of Cardiology, Japan2,
View Study Report
TCTAP C-032
CORONARY - Bifurcation/Left Main Diseases and Intervention
Our Experience of Covered Stent Implantation for a Saphenous Vein Graft Peri-stent Contrast Staining
Naoki Shibata1, Tsuyoshi Sugiura2
Ogaki Municipal Hospital, Japan1, Department of Cardiology, Japan2,
Clinical Information
Patient initials or Identifier Number
O.H.
Relevant Clinical History and Physical Exam
A 47-year-old woman who underwent Bental and hemiarch replacement due to severe aortic regurgitation caused by aortitis syndrome had coronary artery reconstruction using SVG. Two months later, however, emergent PCI to SVG due to VF caused by total occlusion of SVG was performed. Although PCI was succeeded, thereafter, recurrent in-stent restenosis, and advancing peri-stent contrast staining expansion was indicated.
Relevant Test Results Prior to Catheterization
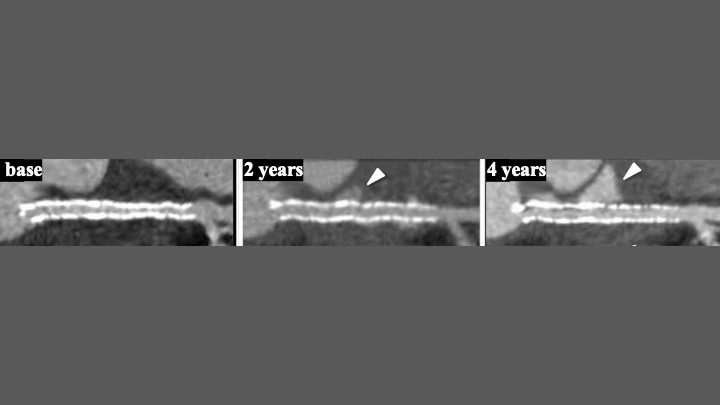
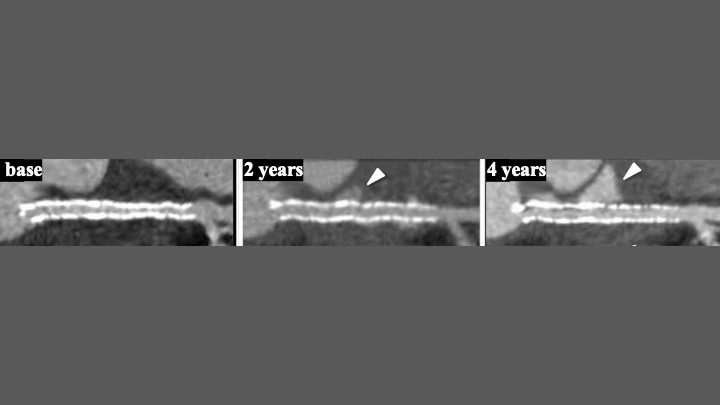
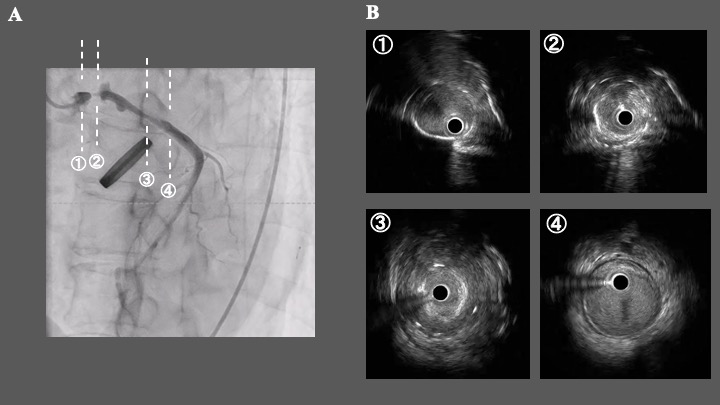
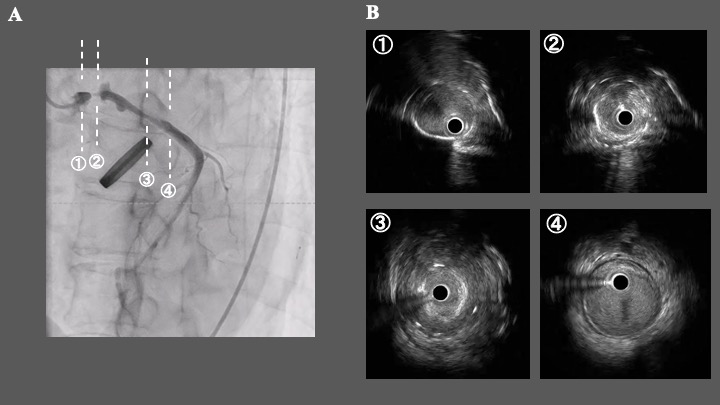
An adequate dose of PSL was prescribed to control the level of inflammation due to aortitis syndrome. CCTA indicated the contrast media extending around the stent (Fig 1).
Relevant Catheterization Findings
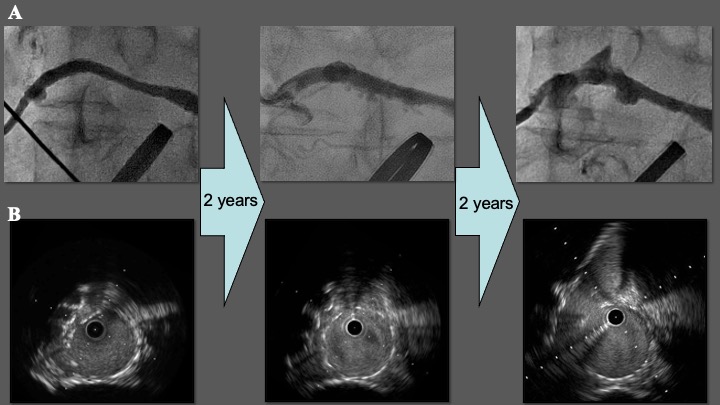
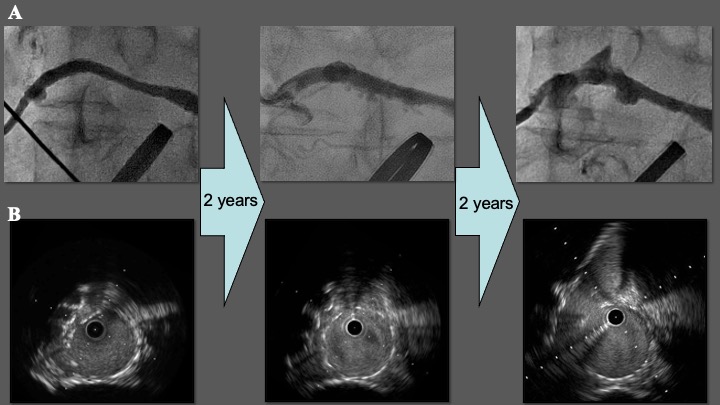
This patient underwent CABG previously, and SVGgraft was connected from ascending aorta to LMT (SVG-LMT). Whereas CoCr-EES was implanted to SVG at the previous PCI session, recurrent ISR and expansion of PSS were indicated (Fig 2-A), and IVUS found a significant positive remodeling of SVG and stent malapposition. (Fig 2-B)
Interventional Management
Procedural Step
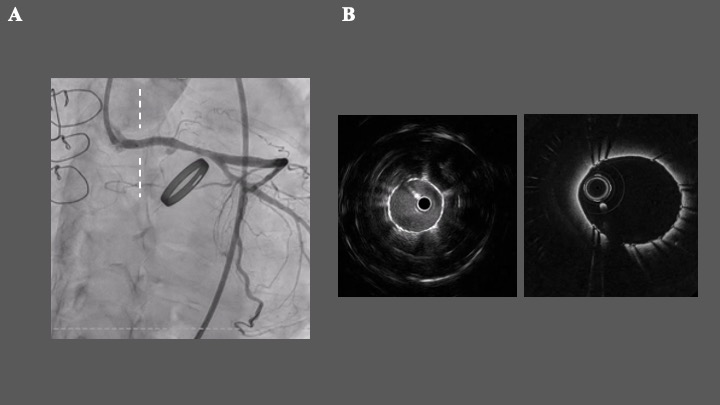
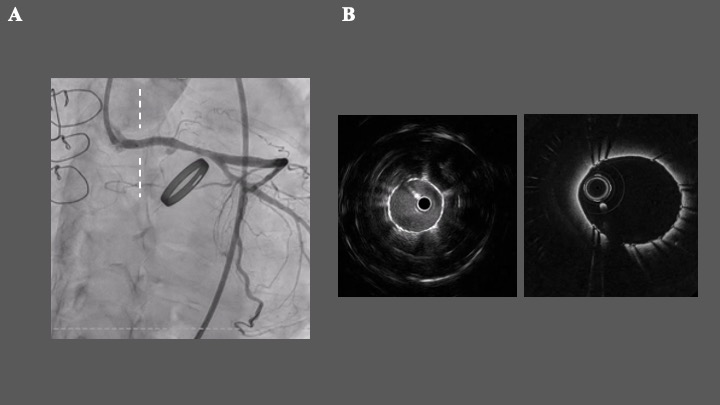
After guiding catheter engaged, angiography showed the significant ISR at SVG's proximal site and remarkable PSS (Fig 3-A). We evaluated this site via IVUS and OCT, revealing severe stenosis due to thrombosis and plaque in the stent (Fig 3-B). After pre ballooning with a cutting balloon (Wolverine 3.0/15mm), we put a covered stent (Graft Master4.8/26mm) at this site (Fig 4-A). Final IVUS and OCT showed the good expansion of the covered stent (Fig 4-B). After confirming the PSS covered completely, we finished this session.
Case Summary
We faced a patient with aortitis syndrome who suffered from repeating coronary stenosis and proceeding PSS. Although PSS is considered an abnormal coronary artery wall response to antiproliferative drug released by DES, staining after DES implantation in SVG is rare. We eventually implanted a covered stent for this lesion to prevent the progression of PSS, but other options might be considered.


