Lots of interesting abstracts and cases were submitted for TCTAP 2021 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don’t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
TCTAP C-005
Presenter
Kogulakrishnan Kaniappan
Authors
Kogulakrishnan Kaniappan1, Ahmad Khairuddin Mohamed Yusof1, Rhuban Sundran1
Affiliation
National Heart Institute, Malaysia1,
View Study Report
TCTAP C-005
CORONARY - Acute Coronary Syndromes (STEMI, NSTE-ACS)
High Risk Percutaneous Coronary Intervention in the Setting of Acute Myeloid Leukemia with Severe Bicytopenia
Kogulakrishnan Kaniappan1, Ahmad Khairuddin Mohamed Yusof1, Rhuban Sundran1
National Heart Institute, Malaysia1,
Clinical Information
Patient initials or Identifier Number
OBG
Relevant Clinical History and Physical Exam
73-year-old male with underlying Bronchial Asthma, referred to us for chest pain, in the setting of newly diagnosed acute leukaemia with severe bicytopenia and leucocytosis. He was initially planned for a diagnostic bone marrow aspiration and aimed for chemotherapy induction later. Upon arrival, he was in respiratory distress, hypoxic with face mask 8L with signs of cardiac failure. He was treated for Non ST elevation Myocardial infarction in failure with concomitant Pneumonia and acute kidney injury
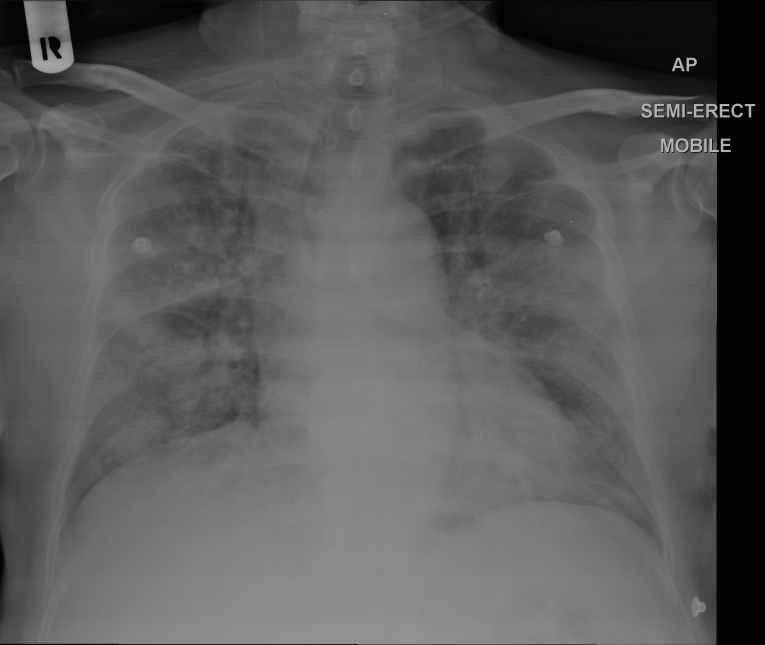
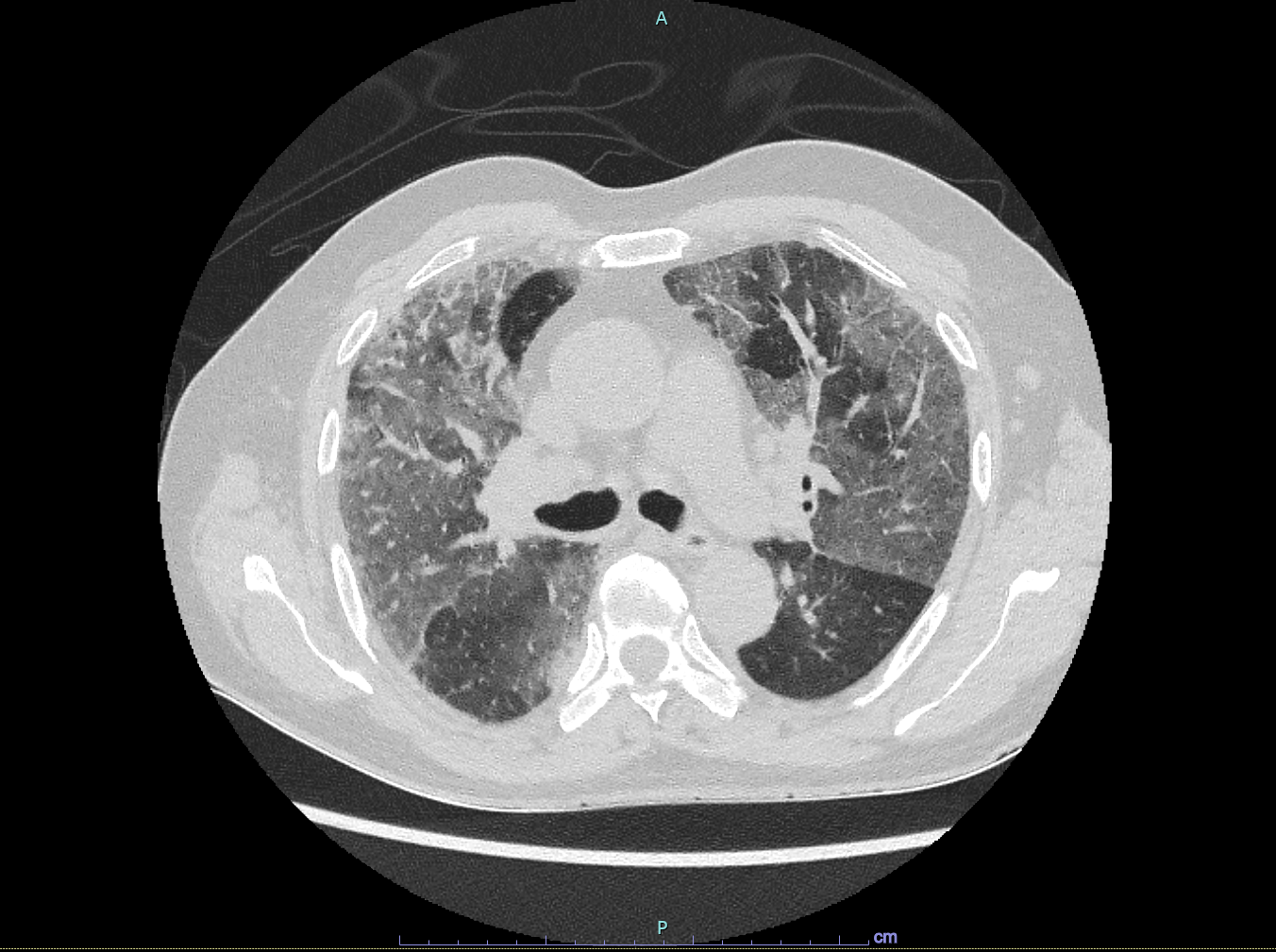
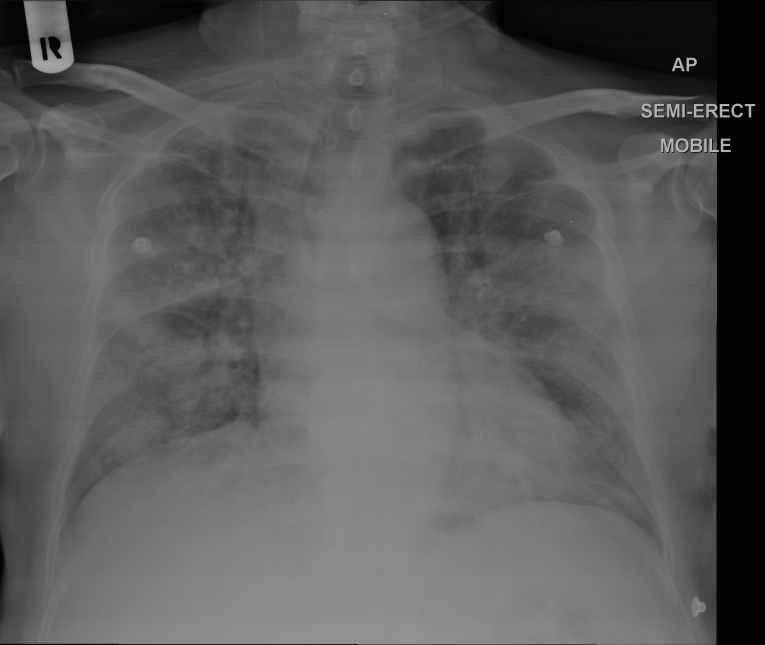
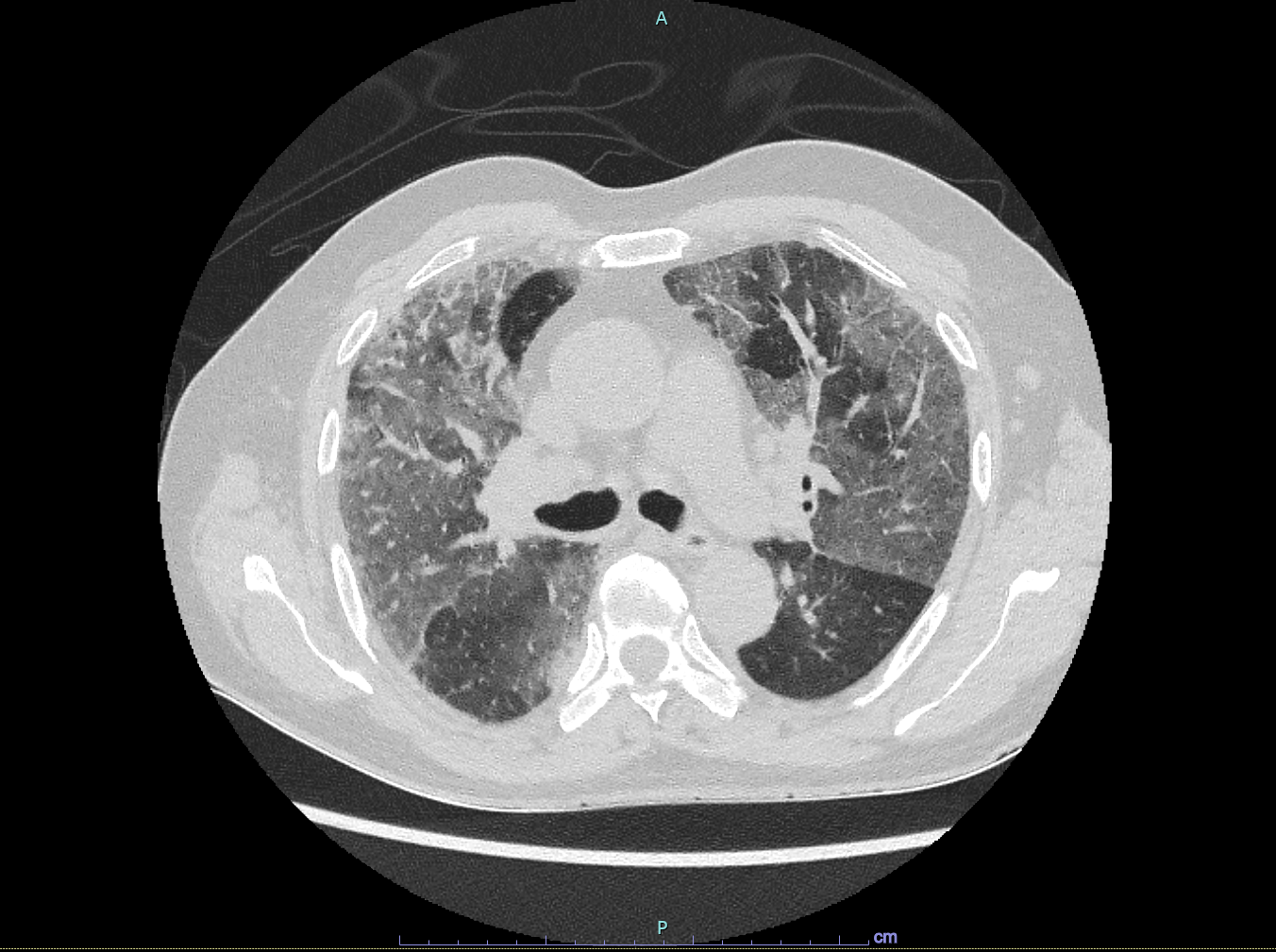
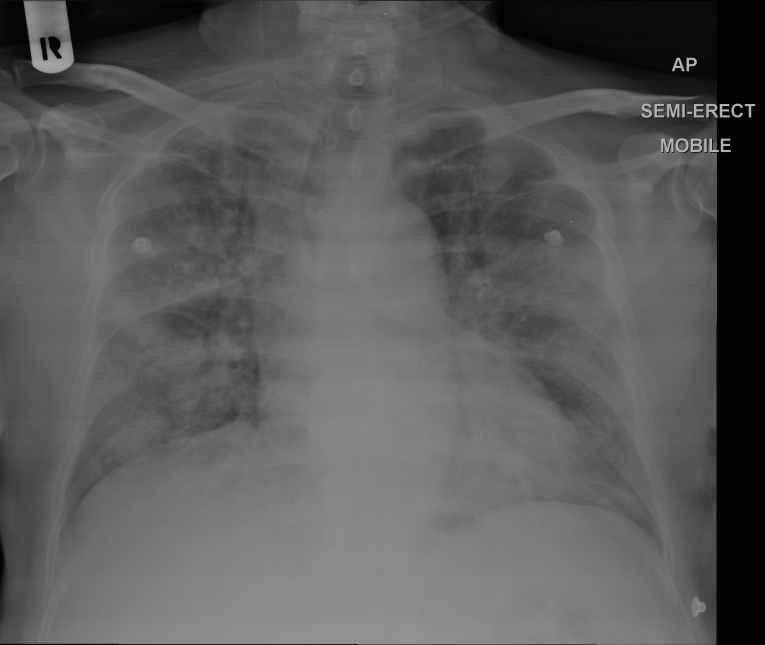
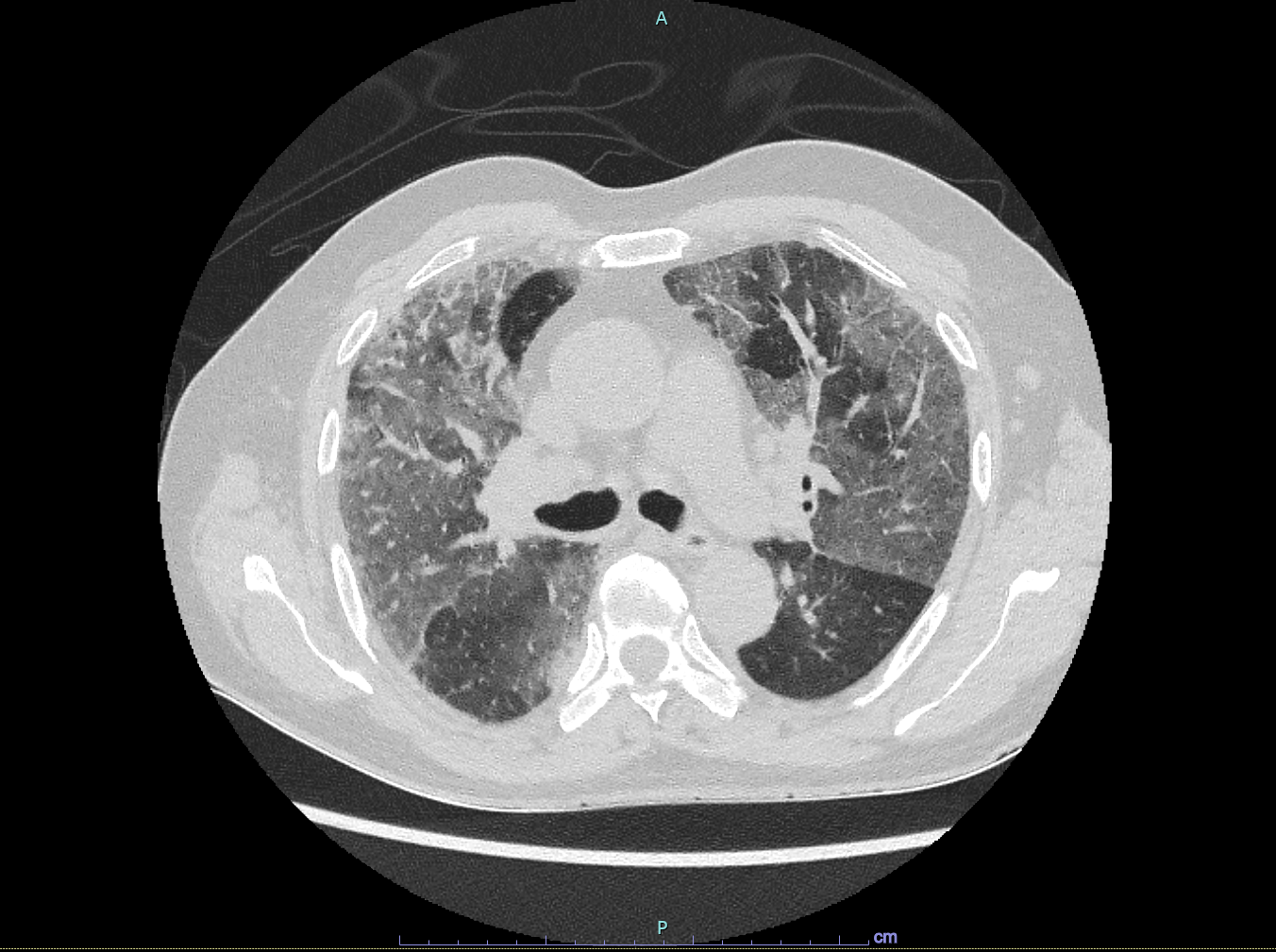
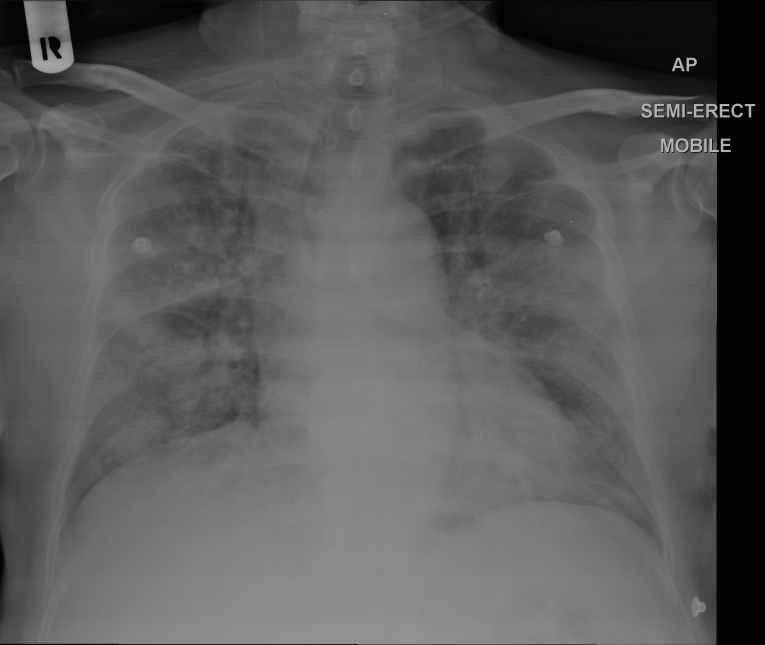
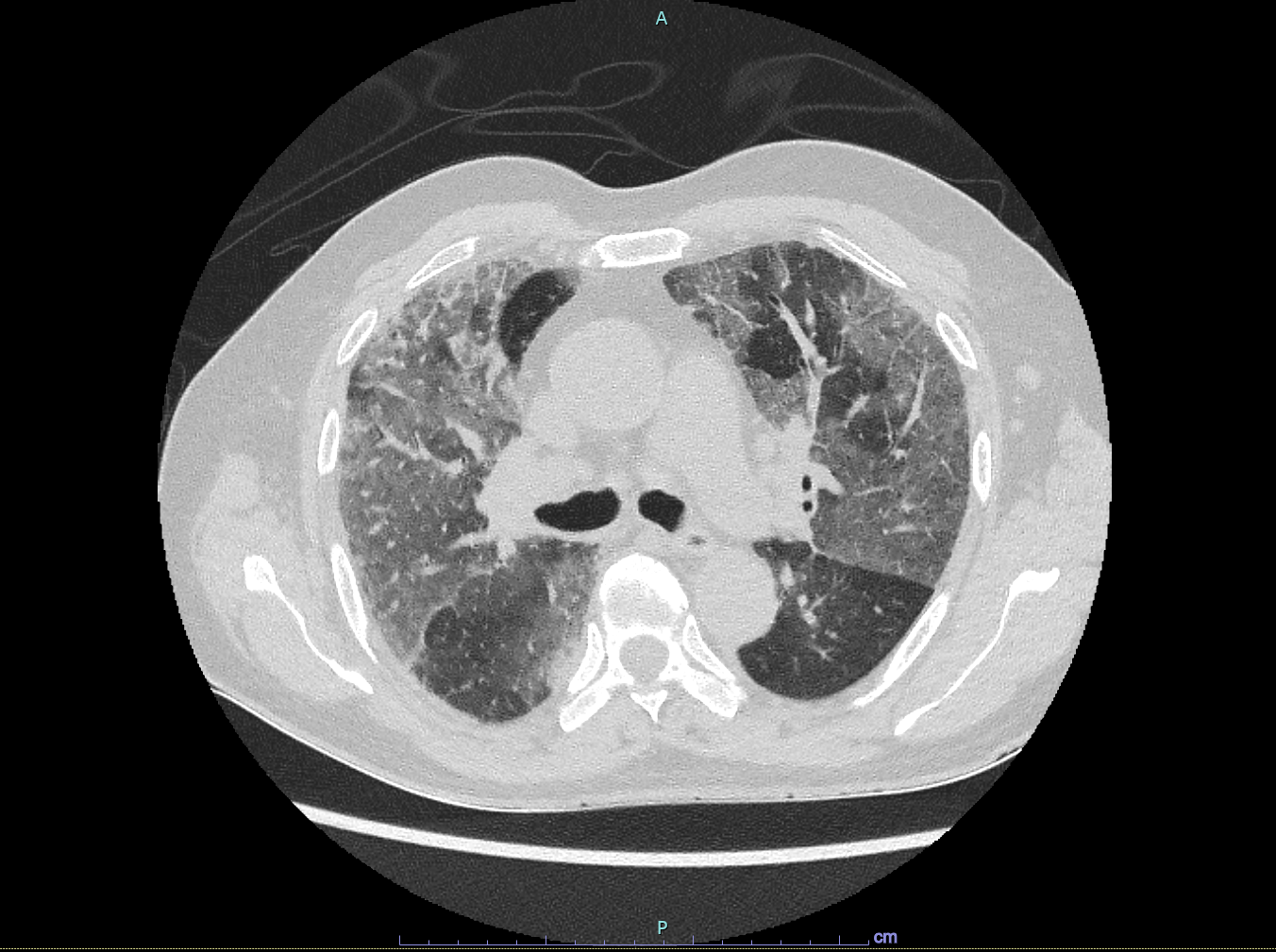
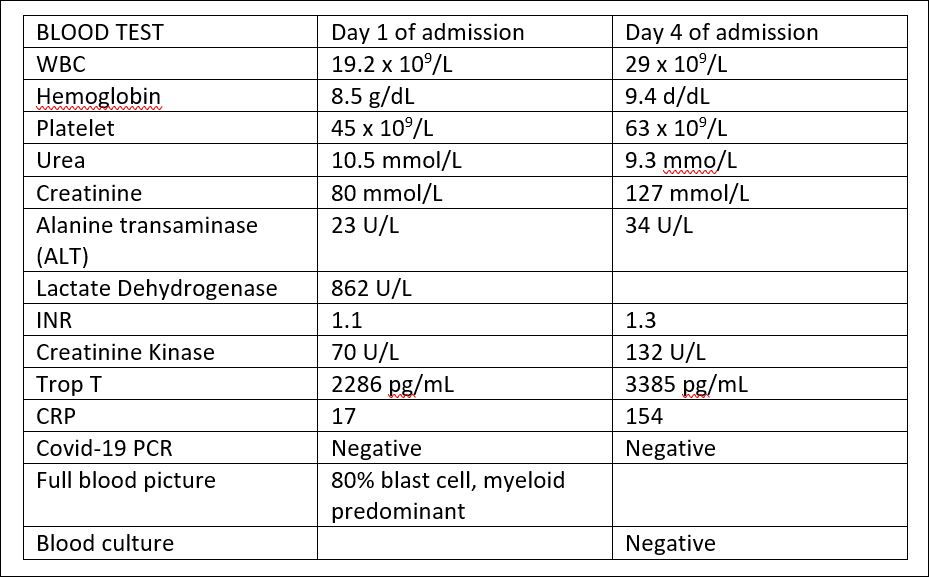
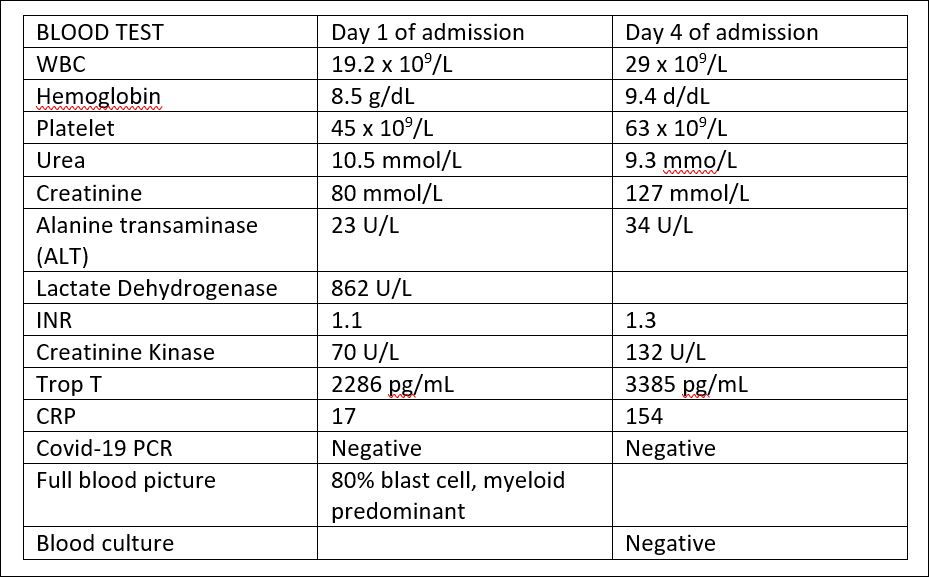
Relevant Test Results Prior to Catheterization
1) Blood tests attached in image format
2) Serial ECG: SR, ST depression in V2 - V6
2) Serial ECG: SR, ST depression in V2 - V6
Relevant Catheterization Findings
CORONARY ANGIOGRAM :
Right radial approach, Opti torque 5f, very tortuous vessel
LMS: smooth, normal
 Caudal View - LAD and LCX arteries.avi
Caudal View - LAD and LCX arteries.avi
 Left Anterior Descending - AP view.avi
Left Anterior Descending - AP view.avi
 Right Coronary Artery.avi
Right Coronary Artery.avi
Right radial approach, Opti torque 5f, very tortuous vessel
LMS: smooth, normal
Interventional Management
Procedural Step
Right radial approach / EBU 3.5 / 6Fr, Run through Floppy wire, TELEPORT microcatheter, GUIDEZILLA guide extension, VIPER wire used RUN THROUGH Floppy wire advanced and wired down LAD, crossed the lesion. Attempted to predilate with SCOREFLEX 2.0/15mm, but unable to cross. Microcatheter TELEPORT introduced for better support. Predilate successfully with MINI TREK 2.0/12 mm at 8 ATM. Then, exchanged with VIPER wire. Proceeded with Orbital Atherectomy with DiamondBack 360 system, run at 80k rpm. Atherectomy done x 7 times sequentially. Re-attempted to predilate with SCOREFLEX balloon, however still unable to cross the lesion. Predilate again with MINI TREK 2.0/12m at 12 atm. Despite predilation with MINI TREK, still unable to pass down bigger sized balloons. GUIDEZILLA II 6FR now inserted and used buddy wire technique with CHOICE PT but still failed to push down bigger balloons. Decided to re-run Orbital Atherectomy DIAMONDBACK at 80k rpm x 5 times sequentially. Finally able to predilate with WEDGE SC 2.5 / 10mm at 10 atm. Finally, deployed DCB SEQUENT PLEASE NEO 2.5 x 20mm at 6 atm for 1 minute to midsegment of LAD. Deployed another DCB SEQUENT PLEASE NEO 3.0 x 20mm at 6 atm for 50 sec at proximal LAD. ST elevation noted transiently during DCB inflation but resolved. Good final results noted. TIMI 3 flow established with no immediate complications
 1) Run Through Floppy wired down LAD.avi
1) Run Through Floppy wired down LAD.avi
 2) Re-run of OAS atherectomy device.avi
2) Re-run of OAS atherectomy device.avi
 3) final shot post DCB deployment.avi
3) final shot post DCB deployment.avi
Case Summary
We humbly seek to highlight the challenges encountered during this high risk PCI in the setting of acute leukaemia with severe bicytopenia, Patient was co-managed with nephrologist and haematologist support to optimize therapy prior to coronary intervention.He received multiple pre and intra procedural packed cell and platelet transfusions. Radial approach was chosen to minimize bleeding risk. We opted for ad hoc orbital atherectomy in view of heavily calcified vessel. Drug coated balloon strategy was carefully chosen after taking into account risk of bleeding, stent thrombosis, double anti platelet duration, post atherectomy vessel outcome and future chemotherapy induction therapy


