Lots of interesting abstracts and cases were submitted for TCTAP 2021 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don’t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
TCTAP A-046
Presenter
Numfon Sinchai
Authors
Numfon Sinchai1, Wongsakorn Luangphiphat2, Chatree Wongsinkongman2, Viroj Muangsillapasart2, Anuruck Jeamanukoolkit3, Piyanart Preeyanont4, Worawut Tassanawiwat5, Jiraporn Laothamatas1, Tanyarat Aramsareewong6
Affiliation
Chulabhorn Royal Academy, Thailand1, Chulabhorn Hospital, Thailand2, Police General Hospital, Thailand3, Cardiac Center, Thailand4, Sunpasitthiprasong, Thailand5, Phramongkutklao Hospital, Thailand6
View Study Report
TCTAP A-046
Imaging: Non-Invasive
Incidence of Silent Ischemic Stroke After Transcatheter Aortic Valve Replacement in Severe Aortic Stenosis in Thailand Using 3.0 Tesla MRI
Numfon Sinchai1, Wongsakorn Luangphiphat2, Chatree Wongsinkongman2, Viroj Muangsillapasart2, Anuruck Jeamanukoolkit3, Piyanart Preeyanont4, Worawut Tassanawiwat5, Jiraporn Laothamatas1, Tanyarat Aramsareewong6
Chulabhorn Royal Academy, Thailand1, Chulabhorn Hospital, Thailand2, Police General Hospital, Thailand3, Cardiac Center, Thailand4, Sunpasitthiprasong, Thailand5, Phramongkutklao Hospital, Thailand6
Background
Neurologic complication like silent ischemic stroke often occurs after transcatheter aortic valve replacement (TAVR) which is an unpredictable incidence, especially in Thailand. We aimed to evaluate the incidence and predictors.
Methods
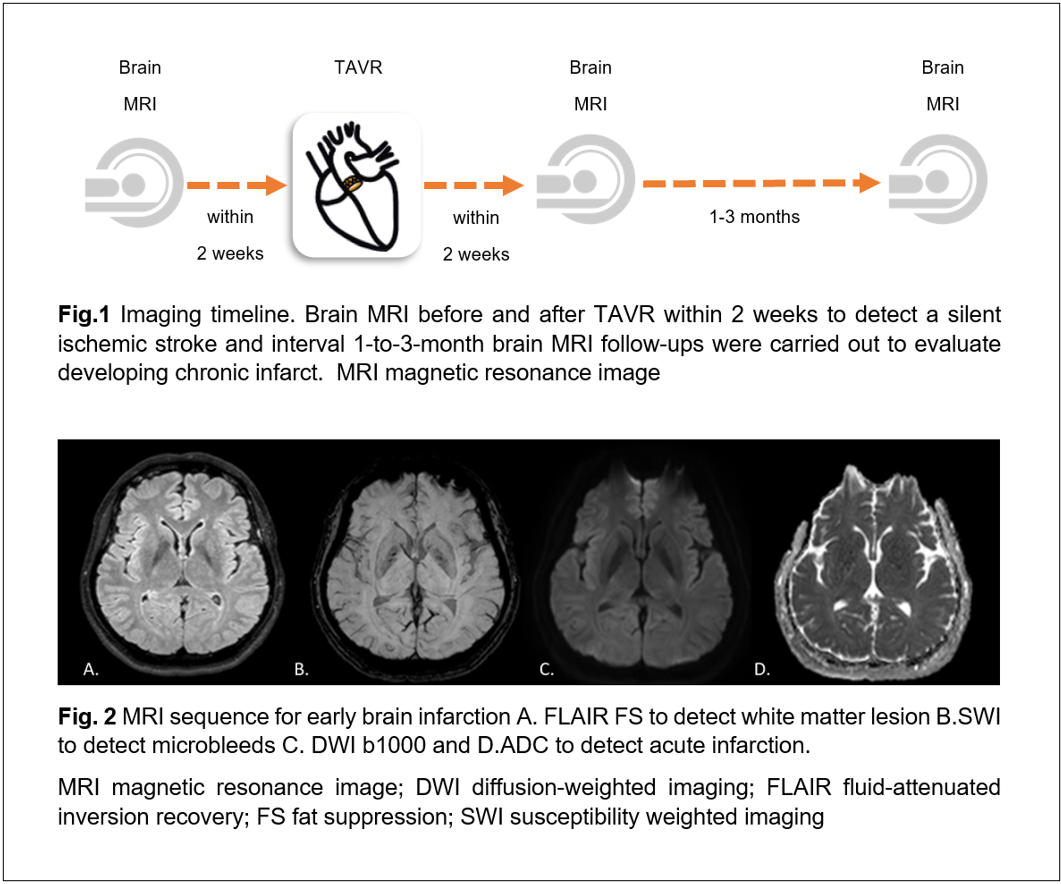
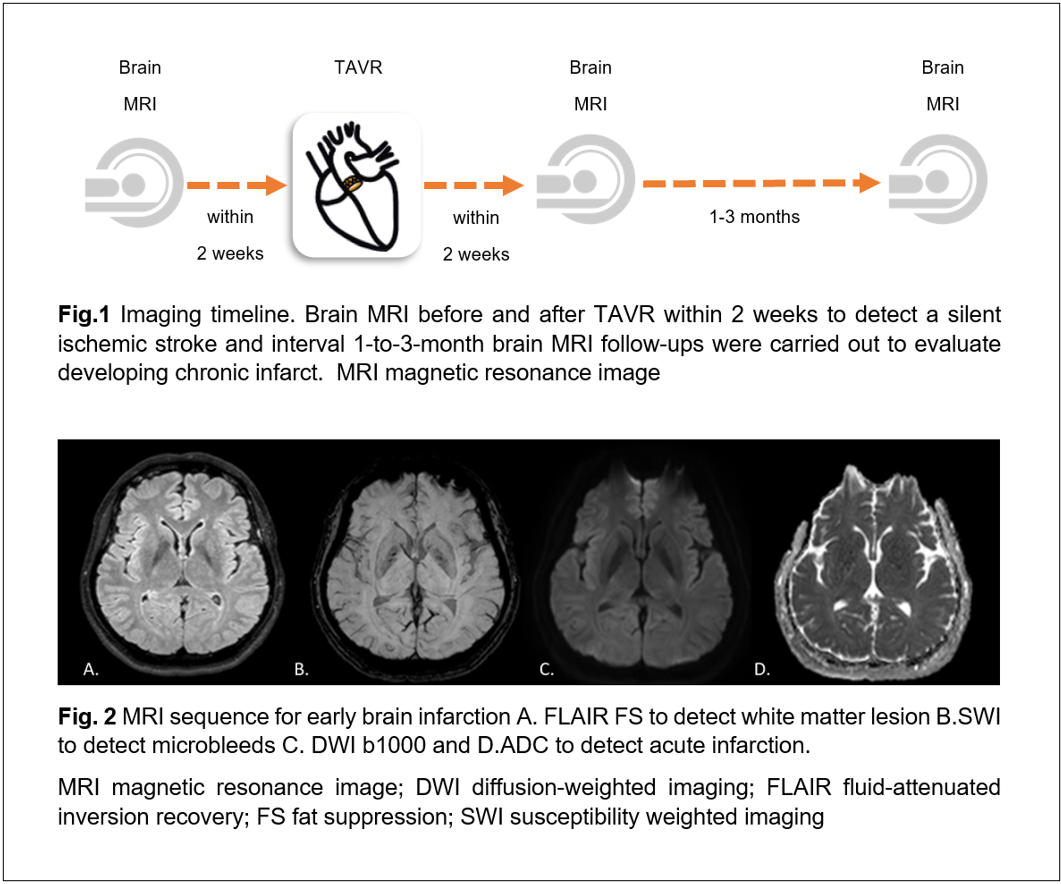
Patients diagnosed with severe aortic stenosis underwent brain MRI before and after TAVR within 2 weeks(Fig 1.) to detect a silent ischemic stroke in terms of number, size, ADC value, location, vascular distribution, and new microbleeds by using DWI b1000, ADC, FLAIR FS, and SWI techniques(Fig. 2). Interval 1-to-3-month brain MRI follow-ups were carried out to evaluate developing chronic infarct.
Results
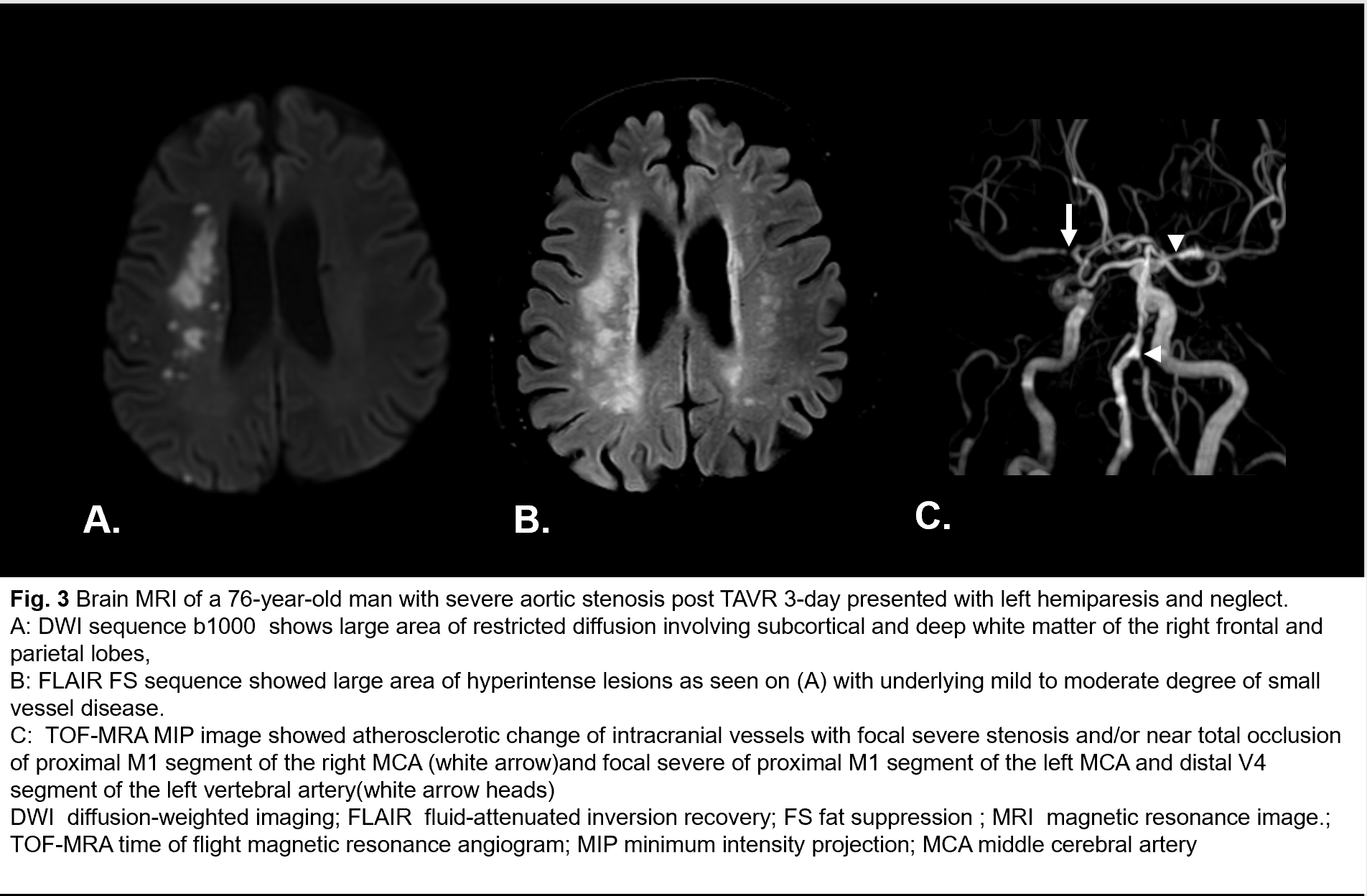
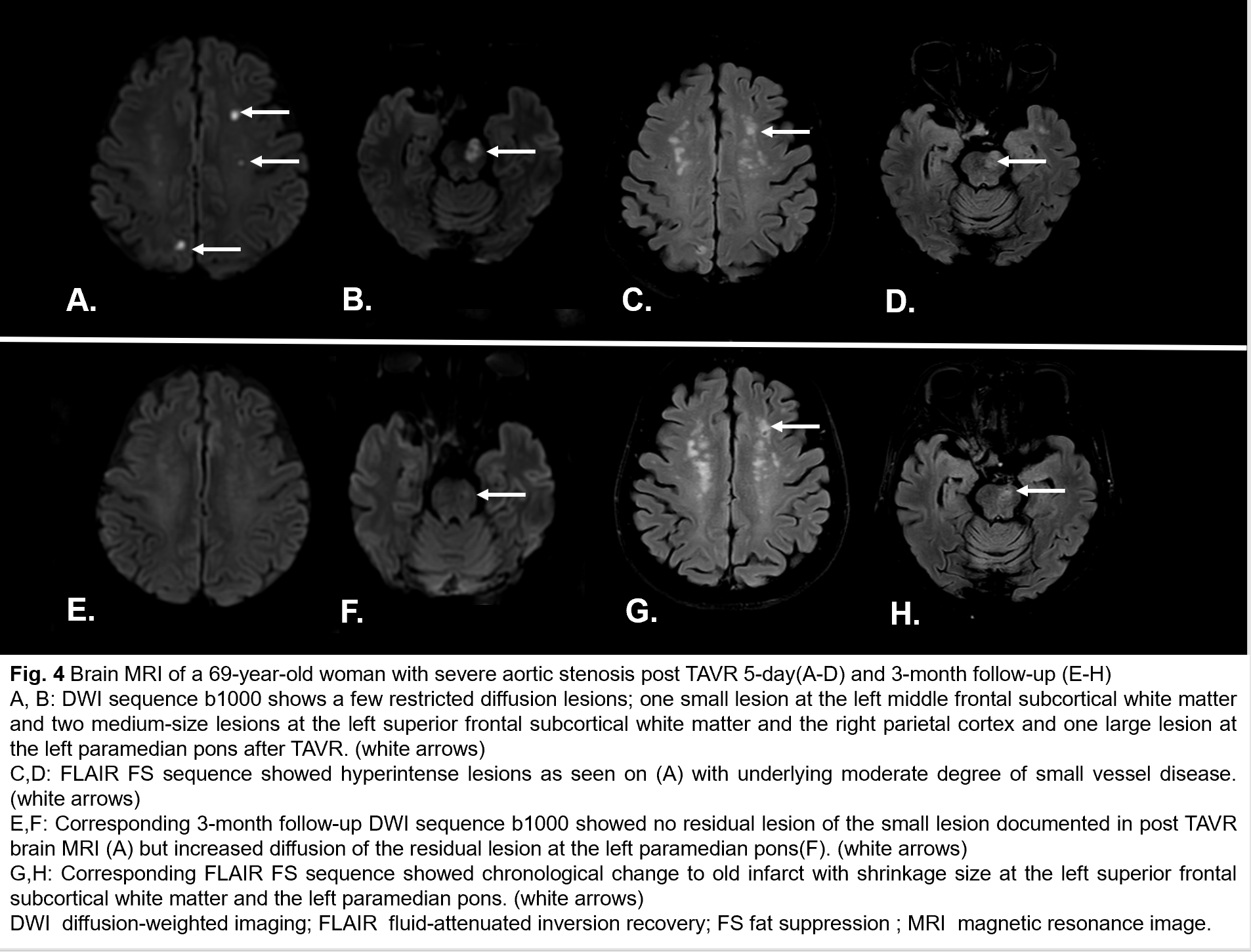
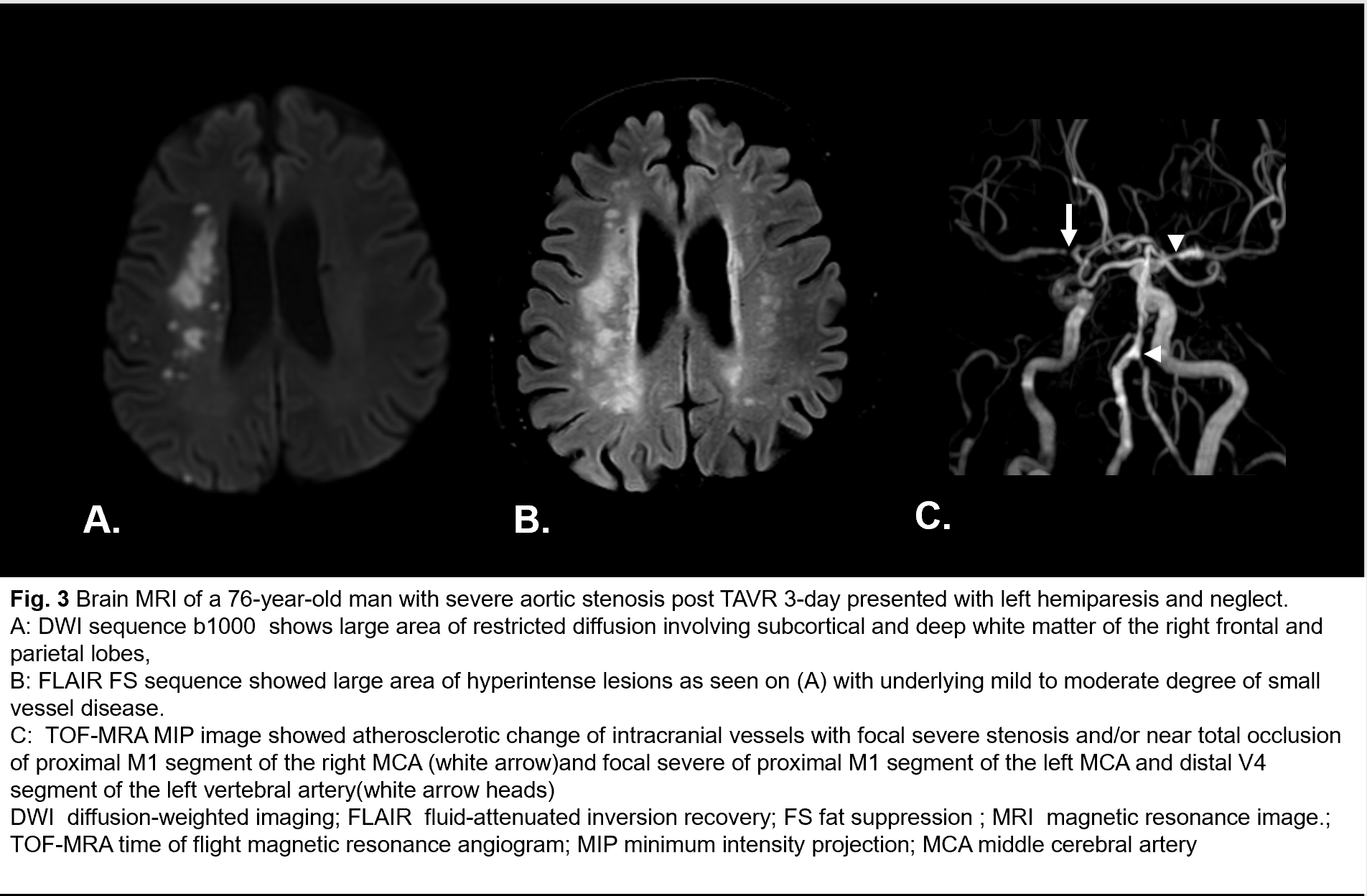
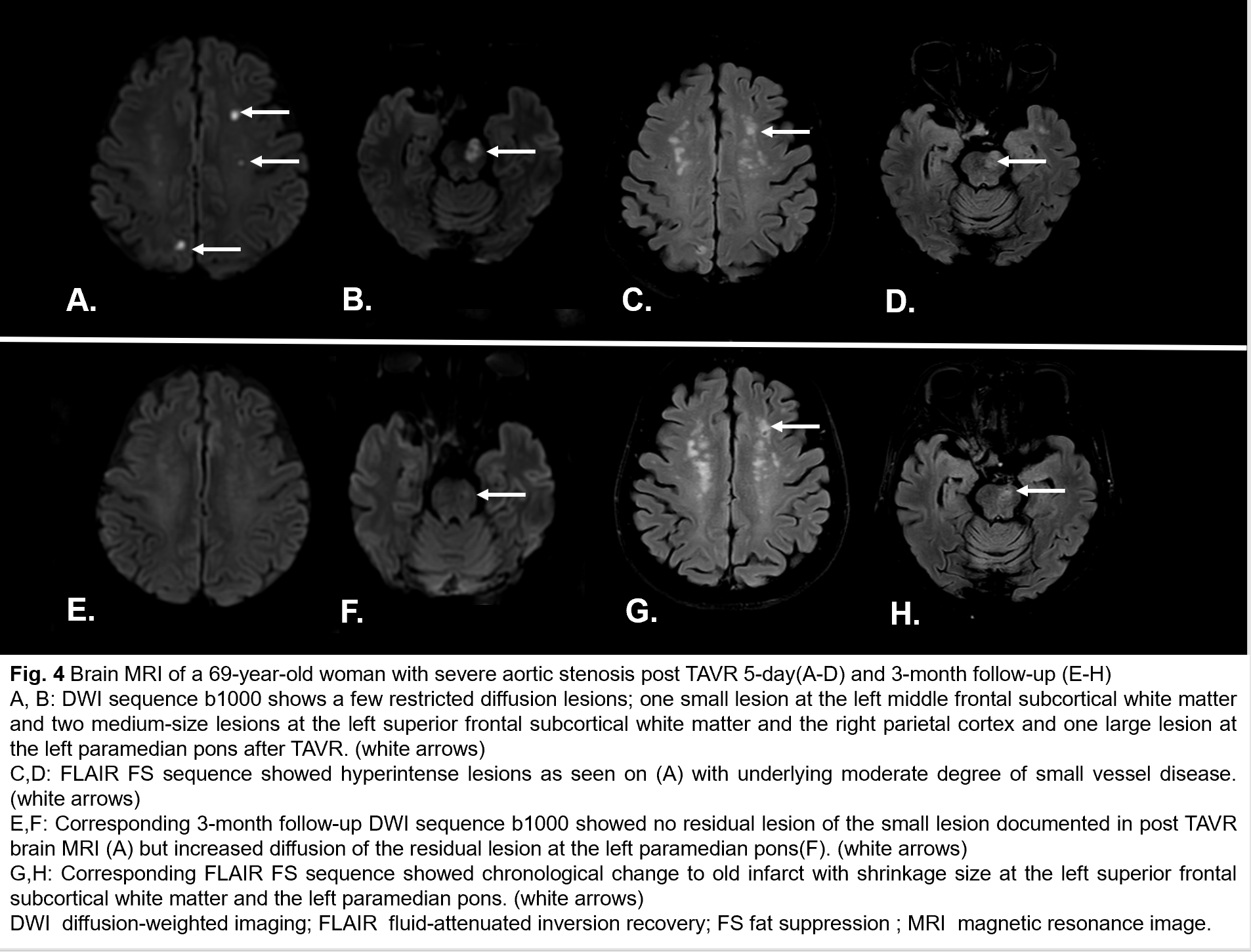
32/34 patients (94%) had acute ischemic foci after TAVR. Most patients had clinically silent ischemic strokes. Only two patients presented with neurological symptoms. One had acute large right MCA infarction with severe stenosis at M1 Segment of the right MCA with atherosclerosis(Fig. 3), and another one had acute left pontine infarction(Fig. 4). Total acute ischemic lesions were 308 lesions with 1 - 59 lesions per patient. 58.4% of lesions were small (≤ 3 mm), 40% were medium (4 -10 mm) and 1.6% were large (> 10 mm). ADC value was 0.1 - 1.33x10−3 mm2/s (mean±SD = 0.61±0.17 x10−3 mm2/s) representing acute infarct with fewer varying ages. The distribution of the lesions was predominantly in the left cerebral hemisphere (34%) which mostly located at the left frontal lobe, cortical/subcortical region. Middle cerebral artery (MCA) territory is most affected which is followed by posterior cerebral artery (PCA) and anterior cerebral artery (ACA) territories. After 1-to-3-month follow-up, only 71 lesions chronologically changed into chronic infarct with shrinkage size. New microbleeds were 8 lesions and macrobleed were 4 lesions which some are not associated with acute infarct location. The valve dislodgement (B=36.18, p=0.007) was only independently associated with the number of post TAVR acute infarct foci.
Conclusion
Most patients undergoing TAVR had a silent ischemic stroke with embolic nature. Valve dislodgement was only independently associated with the number of post-TAVR acute infarct foci. Major neurologic complications occur in patients with pre-existing intracranial atherosclerosis with significant vascular stenosis. Pre-operative brain MRA could help with the early detection of significant intracranial arterial stenosis as systemic atherosclerosis.


