TCTAP A-002
Physiologic Lesion Assessment
Limitation of Angiographic Parameters in Predicting Residual Ischemia after Drug-eluting Stent Implantation
Jaewook Chung1, Jinlong Zhang2, Doyeon Hwang1, Seokhun Yang1, Jeehoon Kang1, Jung-Kyu Han1, Han-Mo Yang1, Kyung Woo Park1, Joo Myung Lee3, Chang-Wook Nam4, Eun-Seok Shin5, Joon-Hyung Doh6, Fei Ye7, Shao-Liang Chen7, Tsunekazu Kakuta8, Bon-Kwon Koo1, Hyo-Soo Kim1
Seoul National University Hospital, Korea (Republic of)1, The Second Affiliated Hospital of Zhejiang University School of Medicine, China2, Samsung Medical Center, Korea (Republic of)3, Keimyung University Dongsan Hospital, Korea (Republic of)4, Ulsan University Hospital, Korea (Republic of)5, Inje University Ilsan Paik Hospital, Korea (Republic of)6, Nanjing First Hospital of Nanjing Medical University, China7, Tsuchiura Kyodo General Hospital, Japan8
Background
We sought to investigate the predictive value of angiographic parameters for residual ischemia after drug-eluting stent (DES) implantation.
Methods
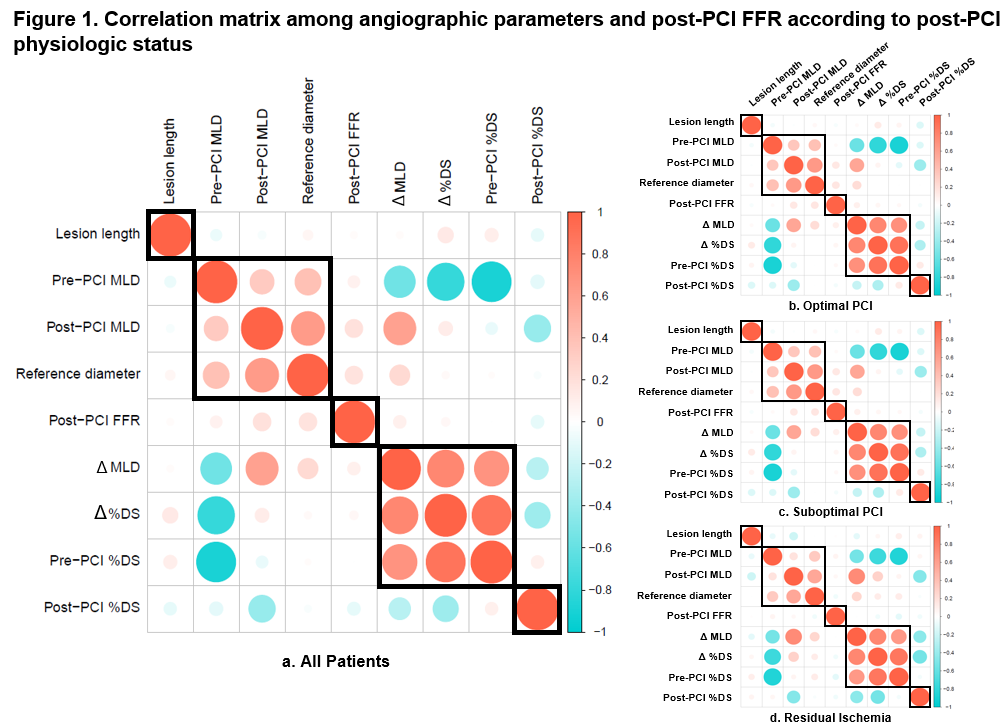
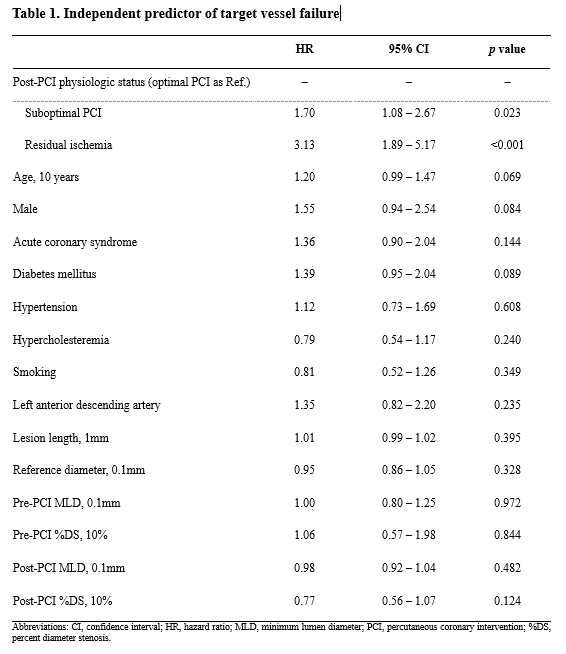
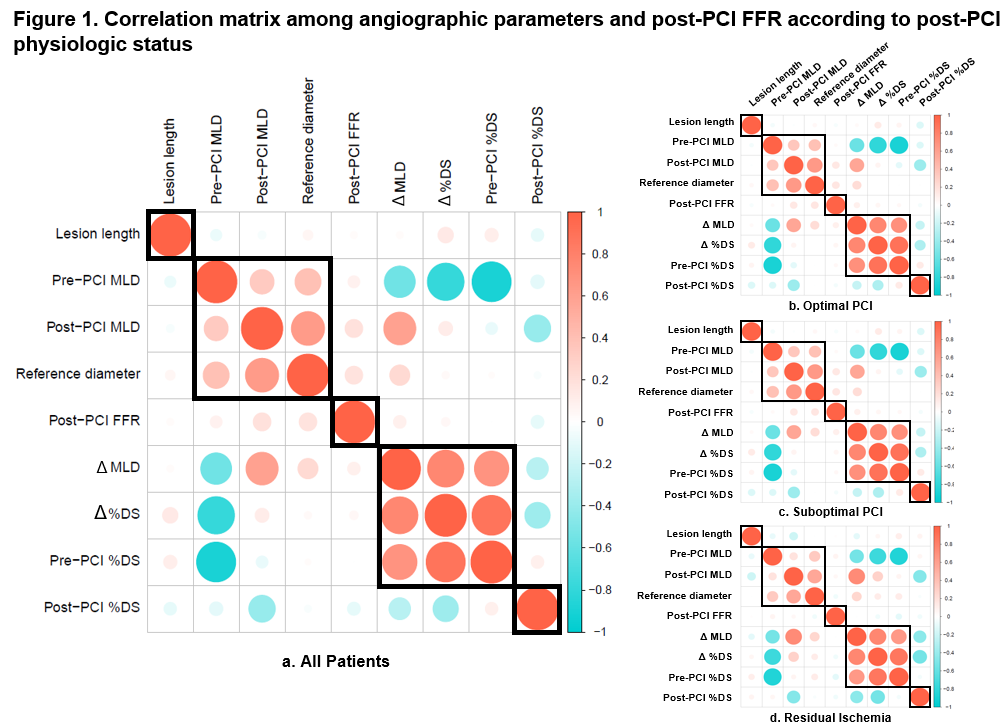
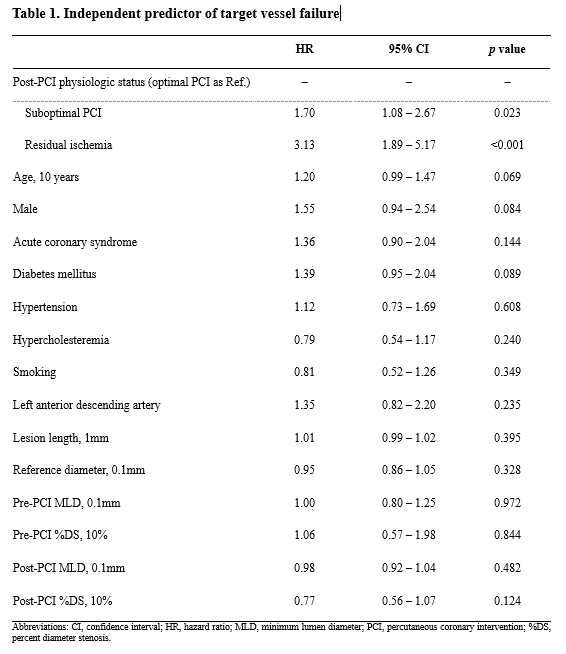
A total of 2,147 patients who underwent percutaneous coronary intervention (PCI) with 2nd generation DES were analyzed. All patients were divided into three groups based on post-PCI fractional flow reserve (FFR) (≥0.88 in optimal PCI, <0.88 or >0.80 in suboptimal PCI, ≤0.80 in residual ischemia). Target vessel failure (TVF) was defined as a composite of cardiac death, target vessel-related myocardial infarction and target vessel revascularization. Association between variables was assessed using the Pearson or Spearman correlation coefficient. Hierarchical clustering of correlation matrix was used to visualize the similarity among the parameters. Survival analysis and multivariable cox proportional hazard regression analysis were used to investigate the cumulative incidence and the independent predictor of target vessel failure.
Results
Among the 2,147 patients, 269 (12.5 %) had residual ischemia. With the exception of optimal PCI group, all angiographic parameters showed insignificant correlations with post-PCI FFR. Hierarchical clustering of correlation matrix showed isolated post-PCI FFR from other angiographic parameters in all groups (Figure 1). The presence of residual ischemia was an independent predictor of TVF (HR 3.13, 95% CI 1.89-5.17, p<0.001), while angiographic parameters were not (Table 1).
Conclusion
Angiographic parameters did not show significant correlations with residual ischemia and could not predict TVF. Physiologic assessment after PCI can improve the patients’ clinical outcomes.