Lots of interesting abstracts and cases were submitted for TCTAP 2021 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don’t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
TCTAP A-049
Presenter
Jasmine Chan
Authors
Andrea Comella1, Jasmine Chan1, Harsh Vipin Thakkar2, Michael Michail1, Brian Ko1, Adam Brown1
Affiliation
Monash Health and Monash University, Australia1, Victorian Heart Hospital, Australia2
View Study Report
TCTAP A-049
Physiologic Lesion Assessment
Non-hyperaemic Pressure Ratios Demonstrate Excellent Agreement with iFR in Patients with Severe Aortic Stenosis
Andrea Comella1, Jasmine Chan1, Harsh Vipin Thakkar2, Michael Michail1, Brian Ko1, Adam Brown1
Monash Health and Monash University, Australia1, Victorian Heart Hospital, Australia2
Background
Fractional flow reserve (FFR) and non-hyperaemic pressure ratios (NHPRs) are well-validated tools that assess the physiological significance of coronary artery disease (CAD). Previous studies have studied the interrelationship between these indices in patients with CAD. However, there is no data exploring whether this association holds true in abnormal resting physiological states, such as that observed in patients with severe aortic stenosis (AS).
Methods
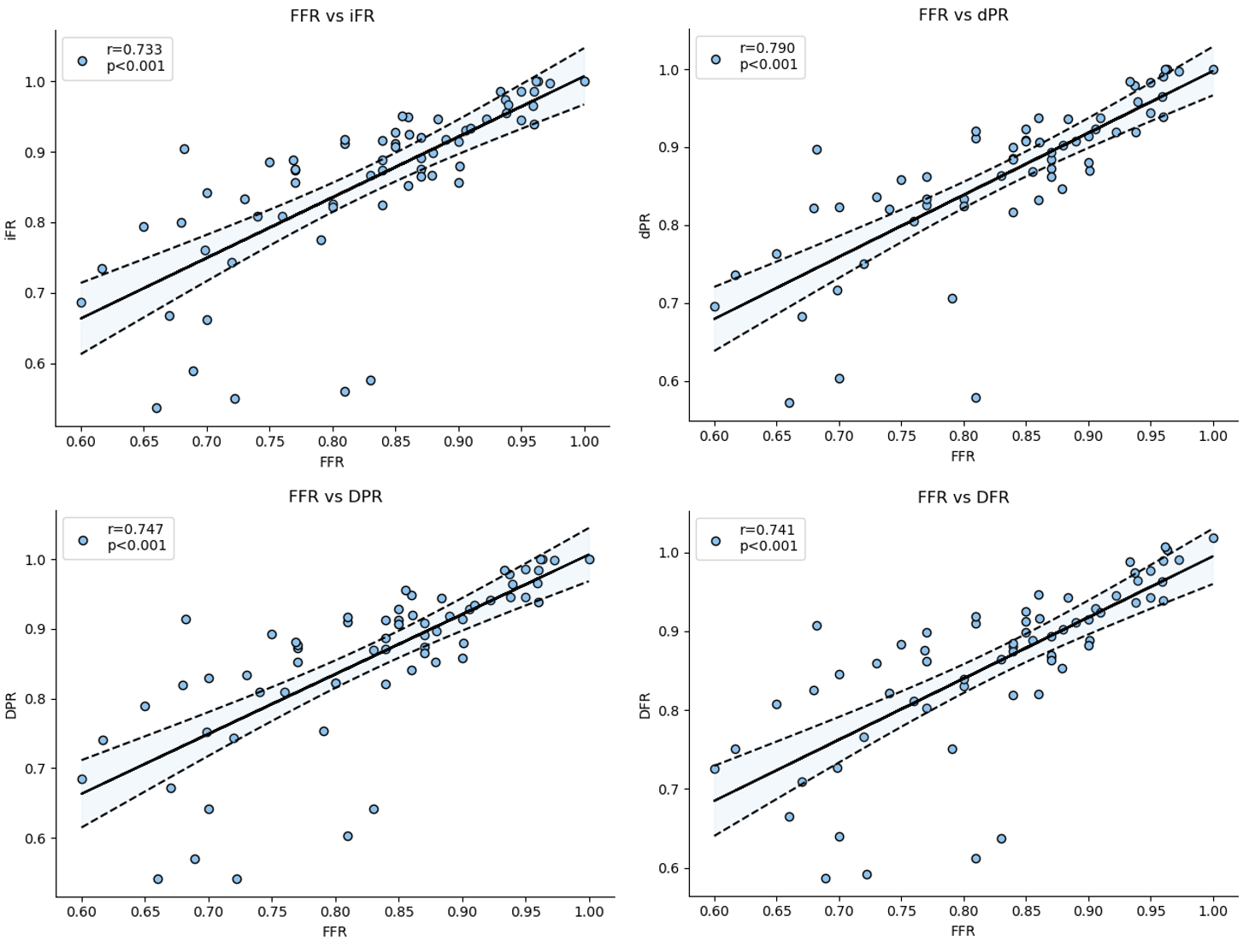
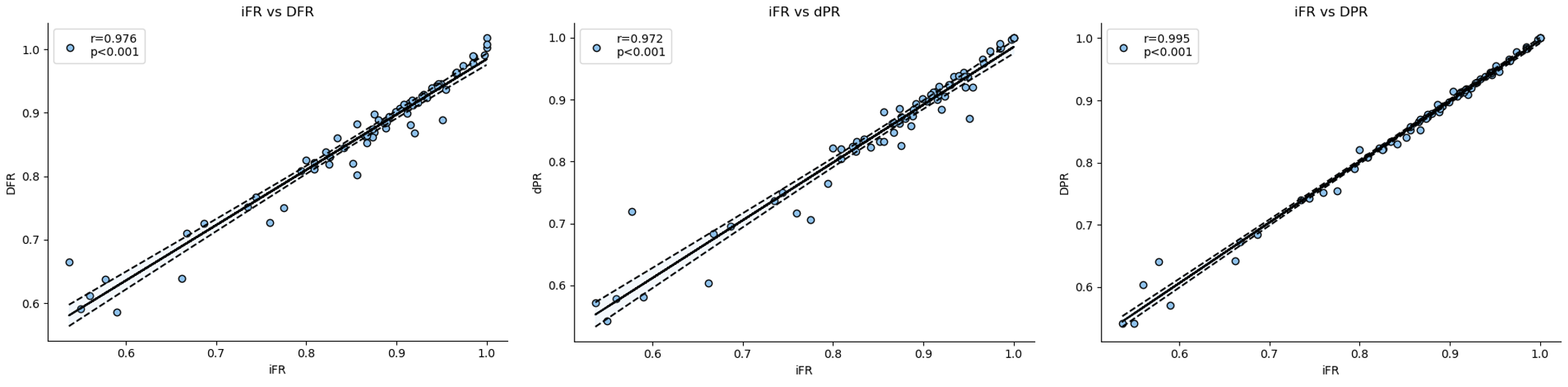
Forty-two patients (67 lesions) with severe AS were prospectively recruited as part of the CAST-FFR study. Patients underwent invasive pressure-wire assessment, and data was extracted to calculate iFR, diastolic pressure ratios (DPR and dPR) and Diastolic Hyperaemia-Free Ratio (DFR). NHPR were first compared with gold standard FFR to determine accuracy and then compared to iFR to determine overall agreement.
Results
Mean age was 75.3 ± 7.5 yrs and mean aortic gradient and DI were 44.3 ± 11.6 mmHg and 0.23 ± 0.04, respectively. Of the 67 vessels, 57% were LAD, 15% LCx, 13% RCA and 12% others. There was a strong positive correlation between FFR and all NHPR, including iFR (r = 0.73, p < 0.001), DPR (r = 0.75, p < 0.001), dPR (r = 0.79, p < 0.001) and DFR (r = 0.74, p < 0.001). ROC analysis demonstrated that the best cut-off values for each tool to predict FFR ≤ 0.80 were iFR 0.89, DPR 0.85, dPR 0.86 and DFR 0.86. Furthermore, there were excellent correlations between iFR and all NHPRs, including DPR (r = 0.99, p < 0.001), dPR (r = 0.98, p < 0.0001) and DFR (r = 0.98, p < 0.0001).
Conclusion
All NHPR demonstrate strong correlation with FFR in patients with severe AS. Furthermore, there is excellent agreement between iFR and other NHPR. These data suggest that no one individual NHPR is significantly affected by the presence of severe AS and they can be used interchangeably in this patient cohort.


