TCTAP A-047
Physiologic Lesion Assessment
Are Diabetic Patients with Above 0.8 FFR Really Safe?
Kyu-Sun Lee1, Bon-Kwon Koo2, Seokhun Yang2, Doyeon Hwang2, Gilwoo Choi3, Joo Myung Lee4, Eun-Seok Shin5, Joon-Hyung Doh6, Chang-Wook Nam7, Hyuk-Jae Chang8, Kyung Woo Park2, Hyun-Jae Kang2, Hyo-Soo Kim2
Daejeon Eulji Medical Center, Eulji University, Korea (Republic of)1, Seoul National University Hospital, Korea (Republic of)2, HeartFlow, Inc., USA3, Samsung Medical Center, Korea (Republic of)4, Ulsan University Hospital, Korea (Republic of)5, Inje University Ilsan Paik Hospital, Korea (Republic of)6, Keimyung University Dongsan Hospital, Korea (Republic of)7, Severance Hospital, Korea (Republic of)8
Background
Fractional flow reserve (FFR) is an invasive method to determine the presence of myocardial ischemia and FFR-guided revascularization has been a standard treatment strategy for patients with coronary artery disease (CAD). Unlike functional significant lesions (FFR ≤ 0.8), the treatment strategy of deferred lesions (FFR > 0.8) is conservative medical treatment and this strategy is relatively safe and showed good clinical outcomes. However, whether deferred lesions are also as safe and have good clinical outcomes in diabetes mellitus (DM) patients is unknown. To investigate this question, we evaluate the clinical outcomes of DM patients with deferred lesions according to FFR.
Methods
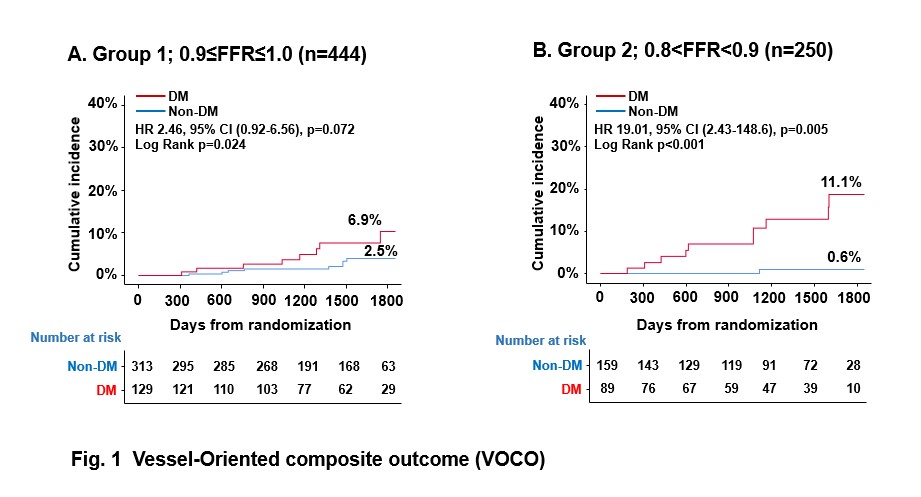
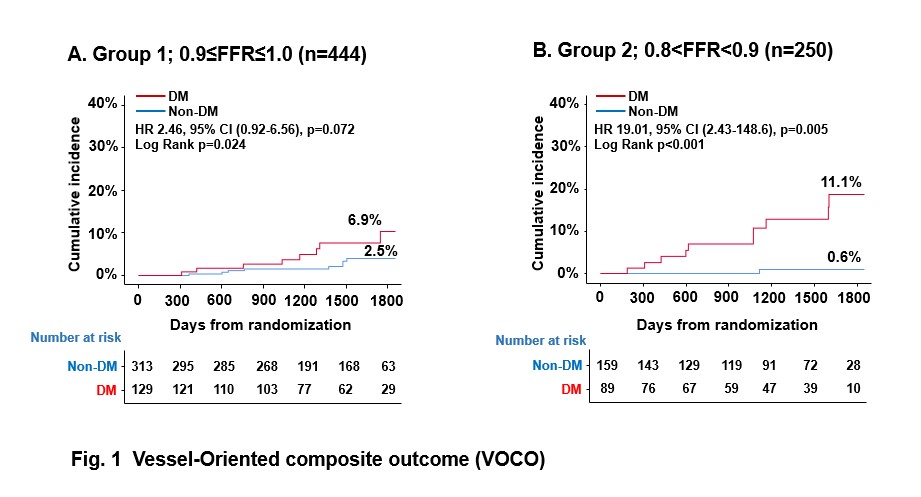
This study was performed based on data of two cohort studies from the 3V FFR-FRIENDS study and institutional registry of Tsuchiura Kyodo General Hospital. Patients with CAD were measured FFR and the vessel-oriented composite outcome (VOCO) (a composite of vessel-related ischemia-driven revascularization, vessel-related myocardial infarction, or cardiac death) at 5years were evaluated according to the presence of DM and FFR values.
Results
A total of 455 patients (mean age 64.7 ± 10.2 years and male 66.7%) with 826 deferred vessels were analyzed. Deferred vessels were divided into 2 groups according to FFR; Group 1 with 0.9≤ FFR ≤ 1.0 (444 vessels) and Group 2 with 0.8< FFR < 0.9 (250 vessels). The VOCO rate is 6.9% in DM patients in Group 1 (Hazard Ratio[HR], 2.46; 95% CI 0.92-6.56, p = 0.024), and VOCO rate is 11.1% in DM patients in Group2 (Hazard Ratio [HR], 19.01; 95% CI 2.43-148.6, p = 0.005). Despite deferred lesions, Group 2 (0.8 < FFR < 0.9) showed significantly higher VOCO rate in DM patient compared to Non-DM patient.
Conclusion
Although FFR-guided management improves clinical outcomes in patients with CAD, DM patients with borderline FFR had poor clinical outcomes. These results suggest that DM patients with borderline FFR might require more intensive therapy.