Lots of interesting abstracts and cases were submitted for TCTAP 2021 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don’t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
TCTAP A-060
Presenter
Choon Keong Tee
Authors
Choon Keong Tee1, Heng Shee Kim1, Kim Fong Ng1, Kumutha Gobal1, Adelyn Nisha Henry1, Vicknesan Kulasingham2, Wei Juan Lim3, Norliza Bt. Othman4, Benjamin Leo Cheang Leng5
Affiliation
Sultanah Aminah Hospital, Malaysia1, Ministry of Health Malaysia, Malaysia2, National Heart Institute, Malaysia3, Hospital Sultanah Aminah, Malaysia4, Columbia Asia Hospital Tebrau, Malaysia5
View Study Report
TCTAP A-060
Others (Structural Heart Disease)
A Rare Case of Arrhythmogenic Right Ventricular Cardiomyopathy with Right Ventricular Clot and Its Potential Complications and Influence on the Timing of Insertion of Implantable Cardioverter Defibrillator
Choon Keong Tee1, Heng Shee Kim1, Kim Fong Ng1, Kumutha Gobal1, Adelyn Nisha Henry1, Vicknesan Kulasingham2, Wei Juan Lim3, Norliza Bt. Othman4, Benjamin Leo Cheang Leng5
Sultanah Aminah Hospital, Malaysia1, Ministry of Health Malaysia, Malaysia2, National Heart Institute, Malaysia3, Hospital Sultanah Aminah, Malaysia4, Columbia Asia Hospital Tebrau, Malaysia5
Background
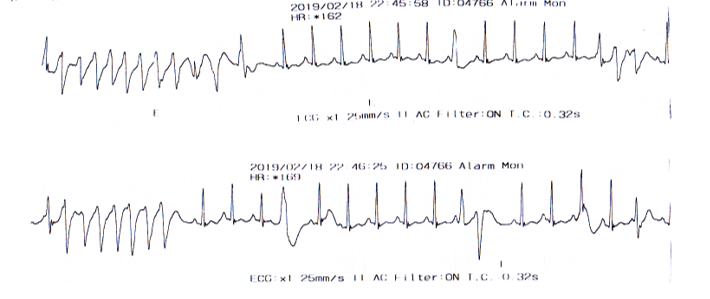
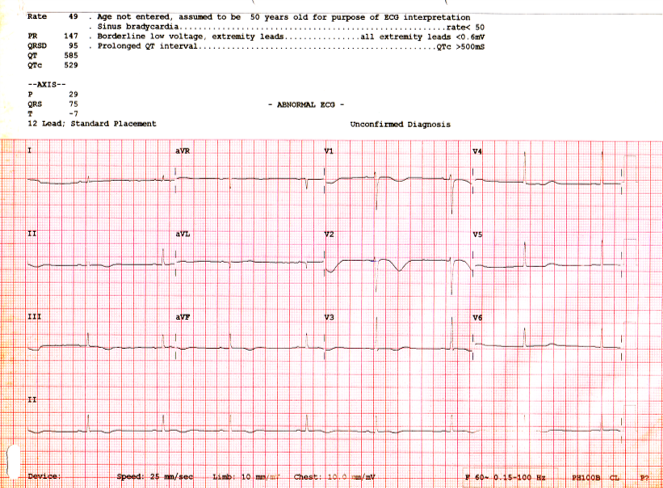
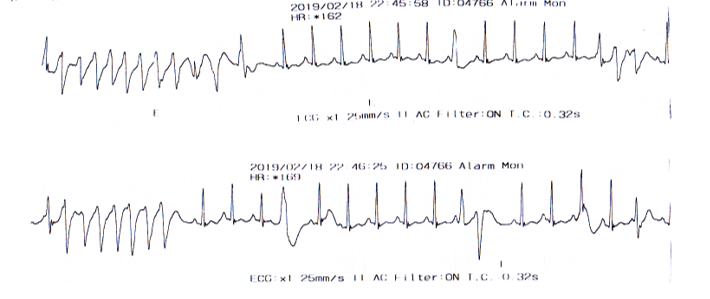
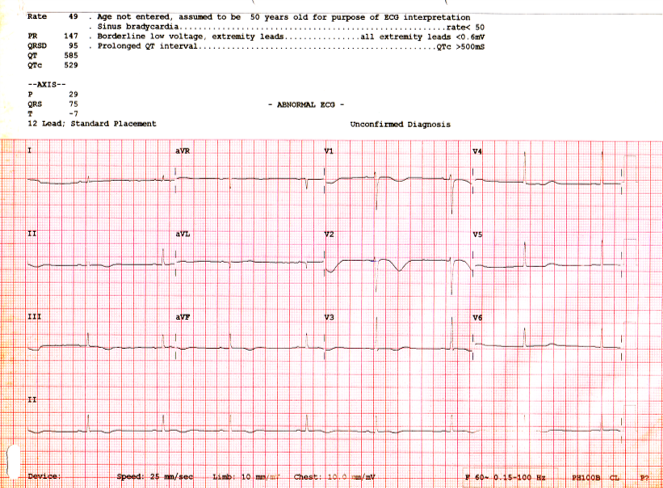
Arrhythmogenic right ventricular cardiomyopathy (ARVC) typically presents in young adults with ventricular arrhythmias and sudden cardiac death. It is characterized by replacement of the myocardium with fibrofatty tissue. Here, we describe a case of a 19-year-old male patient who collapsed during a football game. Resuscitation was performed together with AED showing ventricular tachycardia which was subsequently reverted after defibrillation. His baseline ECG revealed sinus rhythm with symmetrical T wave inversion in the anterior leads. Echocardiogram showed an LVEF of 66% and dilated right ventricle with no appreciable clot. CMR showed right ventricle dyskinesia with fibrosis and right ventricular clot but no fibrofatty infiltration. The findings were suggestive of the diagnosis of ARVC and warranted treatment with an implantable cardioverter defibrillator (ICD) keeping in view electrophysiology study and catheter ablation of VT. Patient was given warfarin for right ventricular clot prior to ICD insertion for four weeks and repeated CMR did not show any residual RV clot. We were able to provide correct diagnosis and management, thereby preventing future lethal consequences. We have also recommended family screening for members of the family who may be asymptomatic for the disease.
Methods
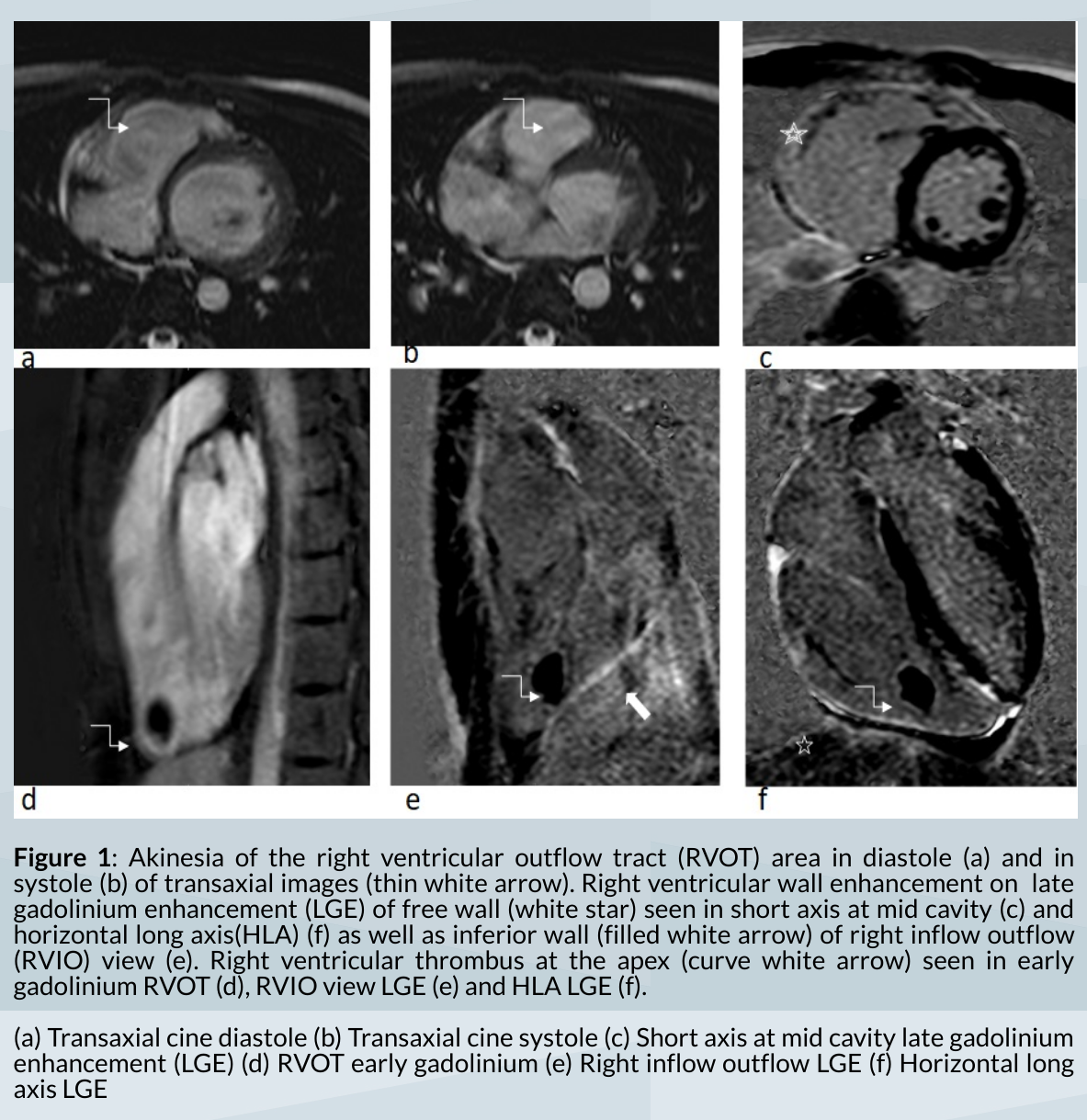
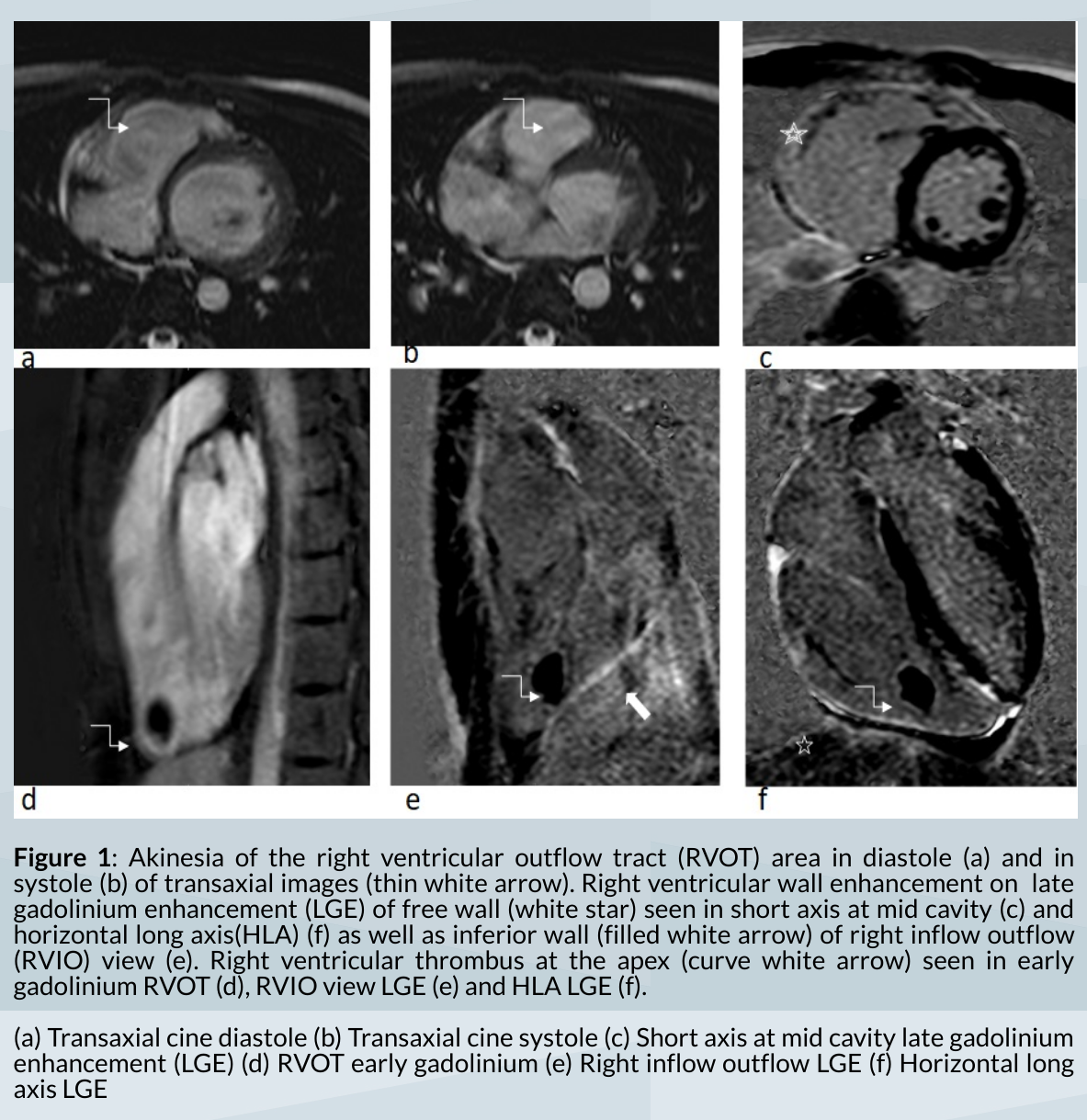
Figure 1: CMR images showing right ventricle dyskinesia with fibrosis and right ventricular clot but no fibrofatty infiltration.The history and investigative findings were suggestive of the diagnosis of ARVC according to the 'Revised Task Force For Diagnosis of ARVC 2010'
Results
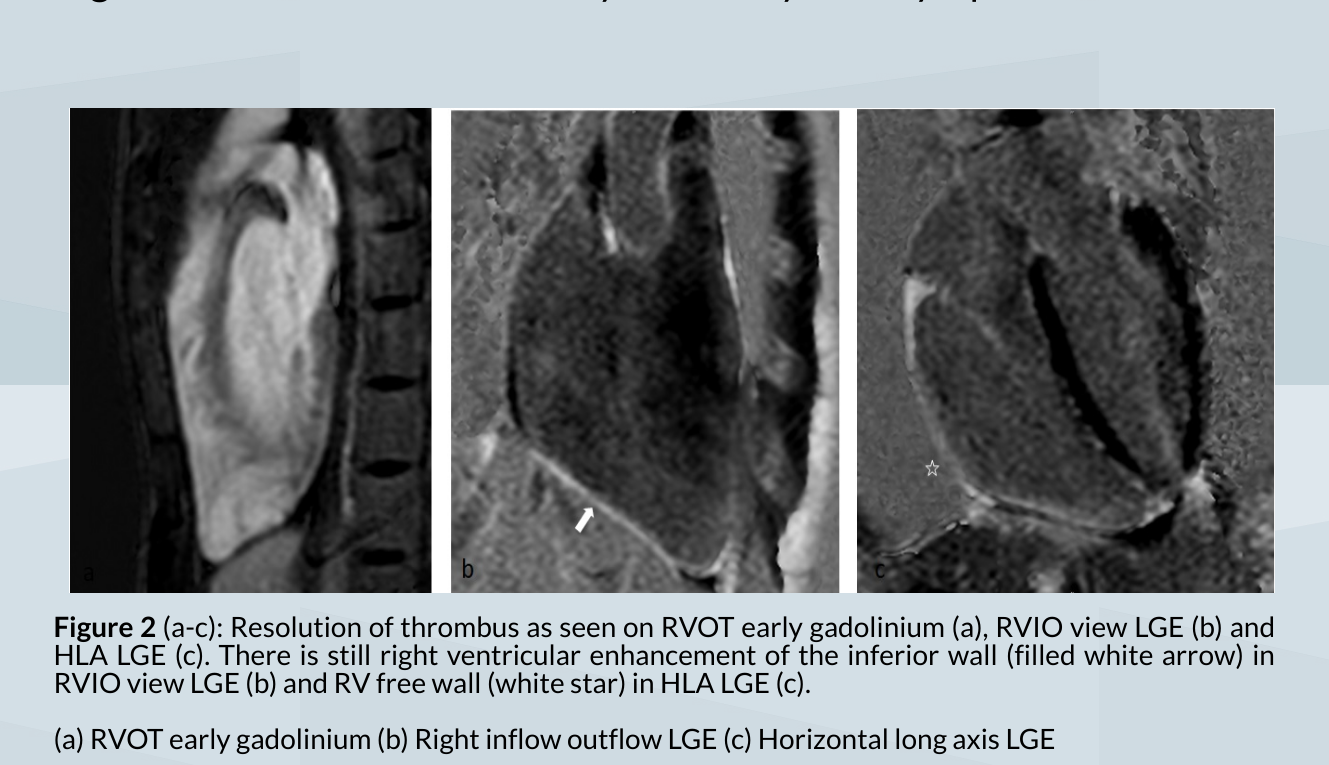
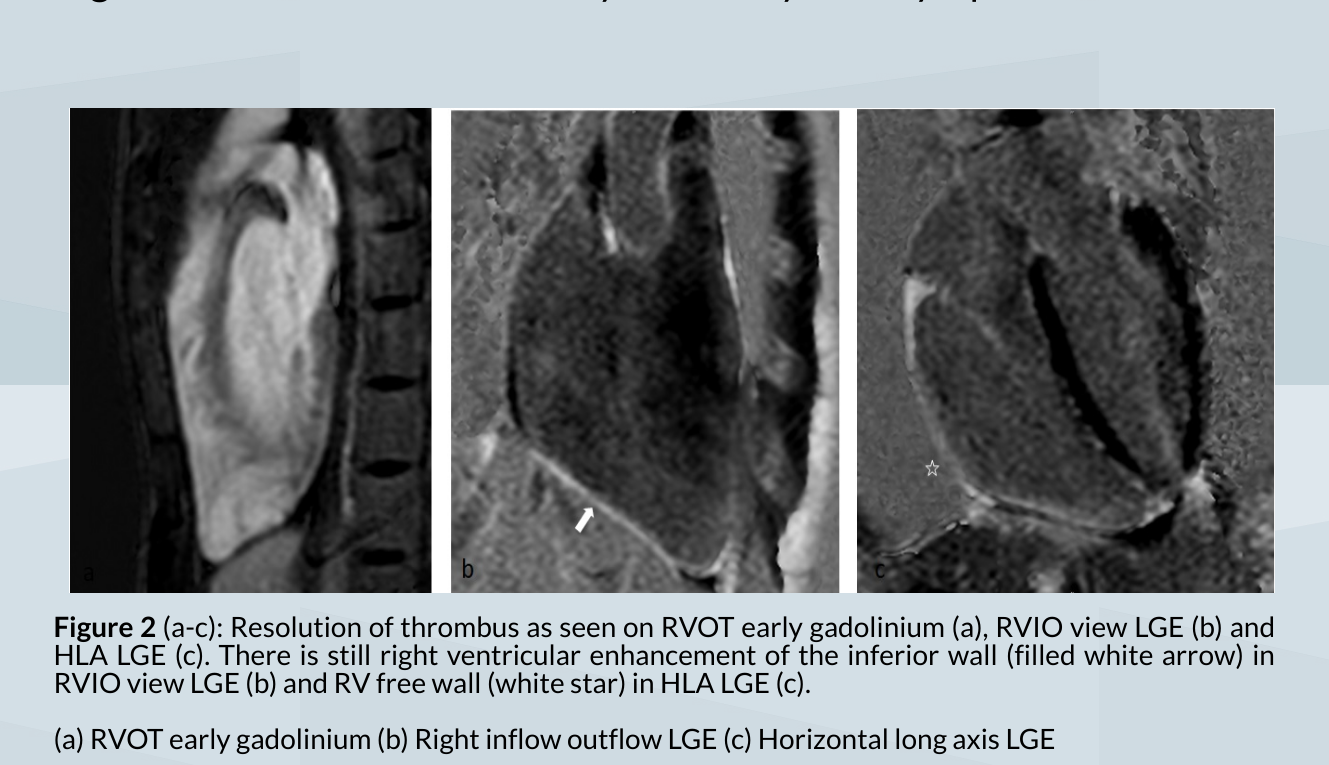
CMR images after four weeks of anticoagulation with warfarin showed resolution of right ventricular clot. An ICD was arranged and was implanted successfully paving the way for future electrophysiology study and VT ablation.
Conclusion
To avoid dislodgement and propagation of clot during manipulation of the right ventricle, we recommend an effort be made to ascertain the presence of clot in ARVC via advanced imaging methods prior to planned intervention. The increasing use of CMR has proven to be useful in the diagnosis and the evaluation of the extent of the structural abnormalities and any associated findings such as a clot in ARVC. However, right ventricular clots are generally not commonly seen even in the presence of advanced right heart failure compared to left ventricular dysfunction.In general, routine anti-coagulation is not recommended in the setting of ARVC, however fatal thromboembolic events may occur if this particular issue is not addressed adequately. The formation of the clot may be contributed by RV dysfunction, RV aneurysm, ventricular arrhythmias, or in the case of patients with ICD, frequent shocks. Effective imaging and appropriate therapy with anticoagulation may improve outcome and prognosis in such cases.


