Lots of interesting abstracts and cases were submitted for TCTAP 2021 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don’t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
TCTAP A-053
Presenter
Babasaheb Deshmukh
Authors
Babasaheb Deshmukh1, Ayan Kar1, Saurabh Dhumale2, Snehil Goswami3, Debdatta Bhattacharyya4
Affiliation
NH-Rabindranath Tagore International Institute of Cardiac Sciences, India1, Narayana Health Rabindranath Tagore International Institute of Cardiac Sciences, India2, NH MMI Hospital, India3, RN Tagore Hospital, India4
View Study Report
TCTAP A-053
Others (Unclassified)
A Simple Reproducible Common Femoral Artery Puncture Technique Using Radiologic Markers to Ensure Safe Zone Punctures
Babasaheb Deshmukh1, Ayan Kar1, Saurabh Dhumale2, Snehil Goswami3, Debdatta Bhattacharyya4
NH-Rabindranath Tagore International Institute of Cardiac Sciences, India1, Narayana Health Rabindranath Tagore International Institute of Cardiac Sciences, India2, NH MMI Hospital, India3, RN Tagore Hospital, India4
Background
Femoral arterial vascular access remains one of the most crucial steps to master for beginners in modern interventional cardiology. Increasing usage of radial access for coronary interventions has reduced the exposure of beginners as femoral access is infrequently being used in diagnostic and interventional coronary procedures. Despite multiple published methods and operator preferences, there still remains an unmet need for a simple and quick reproducible technique, ensuring safe zone punctures so that when the need arises interventional fellows are not found wanting. In this abstract, we describe a technique that is a combination of the palpatory method assisted by radiologic guidance.
Methods
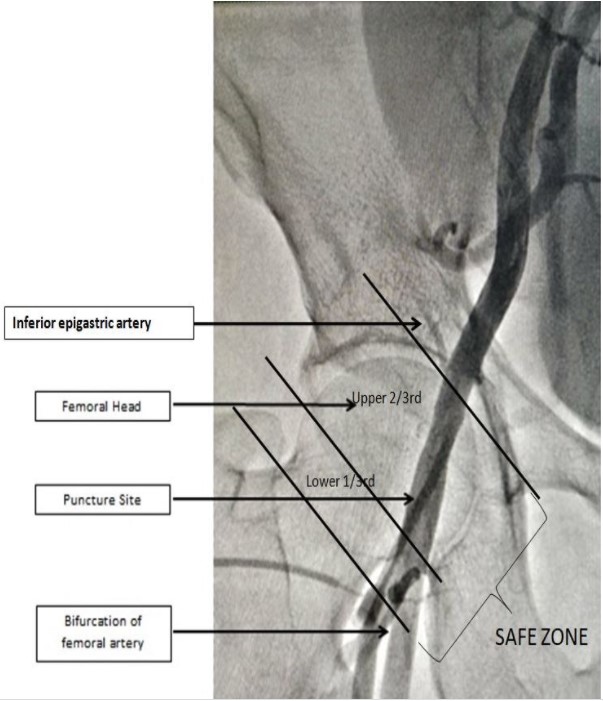
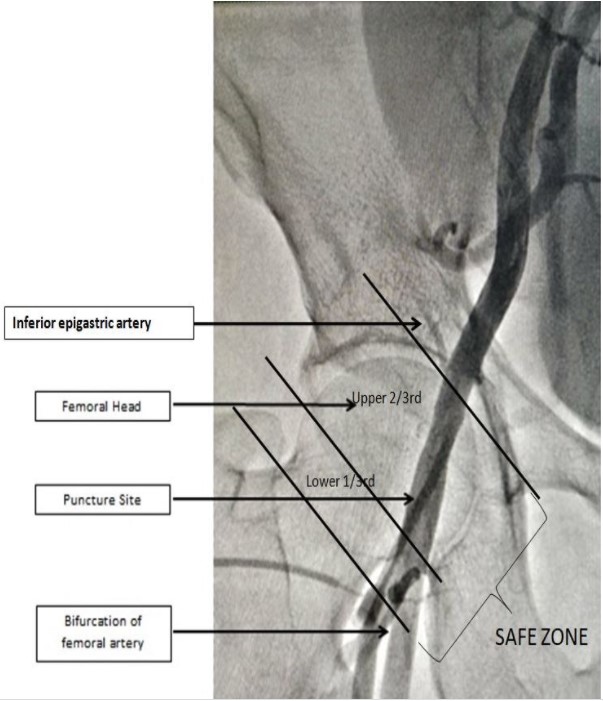
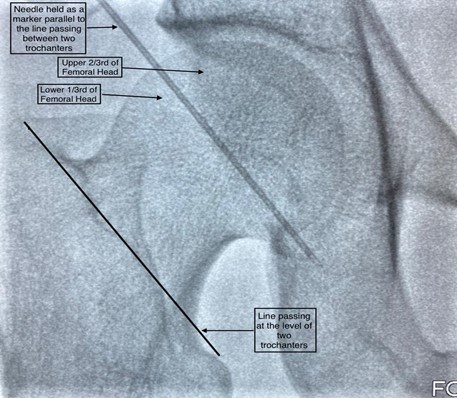
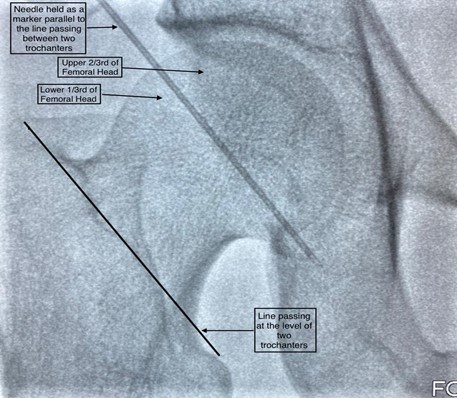
440 consecutive patients who presented for femoral interventions were randomized in 1:1 fashion to “control” and "ïntervention” groups. In the control group, patients underwent arterial puncture by the conventional Seldinger technique using the maximum pulsatility of the femoral pulse as the landmark for arterial puncture.In the intervention group, the following method was carried out to locate the site of puncture. Following aseptic precautions, the femoral head was delineated under fluoroscopic guidance. A puncture needle was placed at the junction of upper 2/3rd and lower 1/3rd of the femoral head, parallel to a line joining the greater and lesser trochanters under fluoroscopic guidance. Next, the surface puncture point was identified in a region 4 cm below the needle, where the femoral artery was best palpable. Local anesthetic was infiltrated, and vascular access obtained. Thus, in the intervention group, the location of the puncture site was determined by two variables ensuring a more restricted site of puncture compared to the control group.At the end of each procedure, a femoral angiogram was taken in both groups using diluted contrast and the site of puncture in relation to the femoral head was noted. Patients in both arms were followed up until discharge for vascular access site complications by a nurse practitioner/physician assistant blinded to the initial randomization. The study data was anonymized, coded and analyzed using SPSS 15.0 to look for rates of complications and frequency of safe zone punctures between the two arms after matching for baseline characteristics. The protocol was reviewed and approved by the Institutional Ethics and scientific committees and all participants provided informed consent.
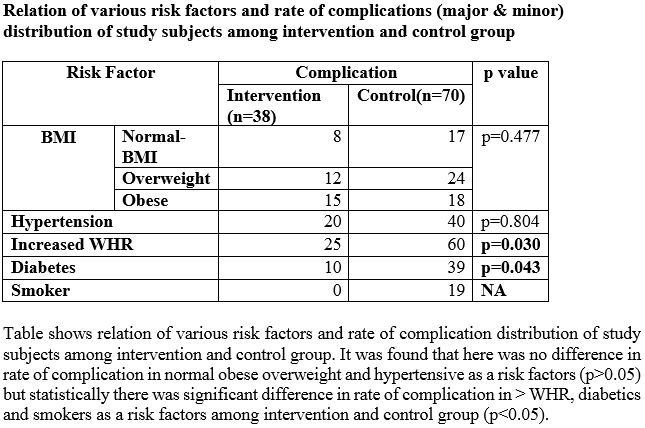
Results
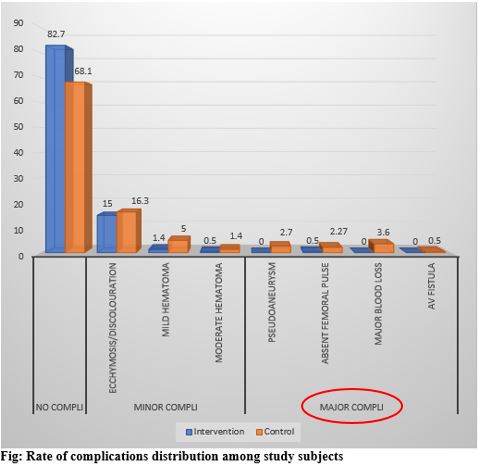
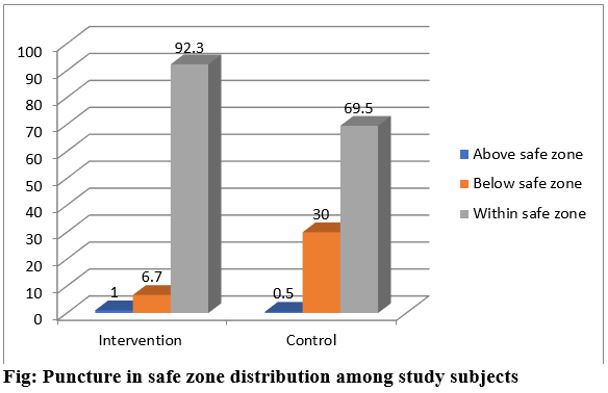
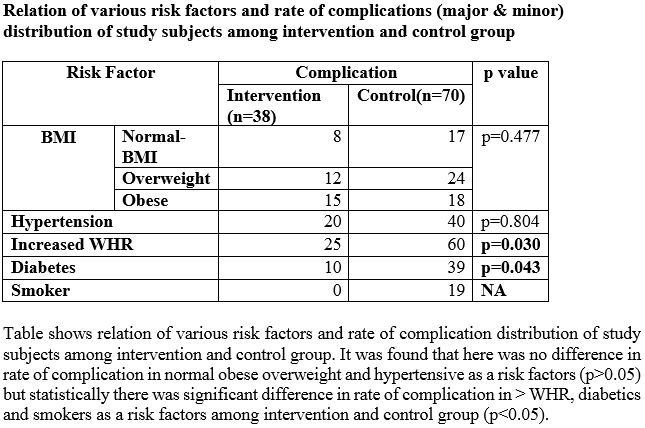
Out of 440 patients included in the study, 220 were in the intervention group and 220 in the control group. The two groups were matched for baseline characteristics like age, sex, Body Mass Index, Waist Hip Ratio, hypertension and diabetes and smoking. We categorized complications into major and minor. Bruising, ecchymosis, minor hematomas<2X2cm and moderate hematomas <5X5 cm in dimensions were considered minor complications. Of the 440 patients included in this study, only (5.6%) had some form of significant vascular access complications in the form of large hematomas, pseudoaneurysms and absent femoral pulses, suggesting the overall low prevalence of major complications. Strikingly however the number of such complications was only 0.05% in the intervention group compared to 9% in the control arm. When the two groups were analysed for complications (major and minor) and risk factors it was found that the rate of overall complications was significantly higher in those subjects with diabetes mellitus and increased waist-hip ratio with the control arm faring worse than the intervention arm.
Of the total 20 major complications reported in the study,19 happened in the control group, of which, in 15(80%) cases the puncture was below the safe zone. More strikingly pseudoaneurysms (n=6) were present only in the control group. Using the new technique safe zone punctures were significantly higher in the intervention group (89.1% Vs 39.74%, p<0.001) compared to the control group with consistently lower rates of complications. When it came to difficult groins in overweight/obese patients (defined as BMI>25kg/m2 and Waist to Hip Ratio(WHR) >0.9) it showed that the new technique assured a safe zone puncture in 80% of the cases. This invariably translated into lesser number of vascular access site complications.
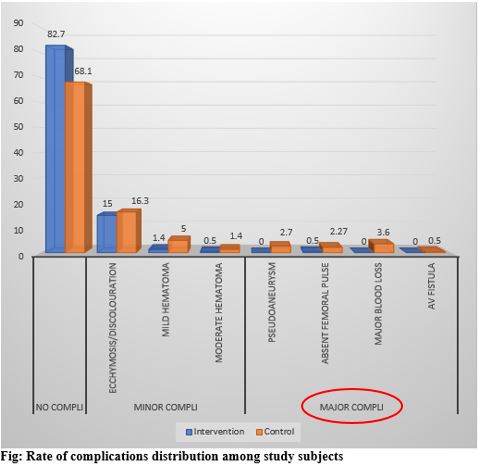
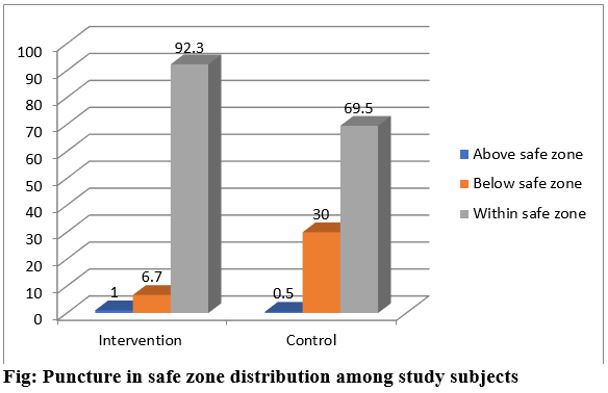
Of the total 20 major complications reported in the study,19 happened in the control group, of which, in 15(80%) cases the puncture was below the safe zone. More strikingly pseudoaneurysms (n=6) were present only in the control group. Using the new technique safe zone punctures were significantly higher in the intervention group (89.1% Vs 39.74%, p<0.001) compared to the control group with consistently lower rates of complications. When it came to difficult groins in overweight/obese patients (defined as BMI>25kg/m2 and Waist to Hip Ratio(WHR) >0.9) it showed that the new technique assured a safe zone puncture in 80% of the cases. This invariably translated into lesser number of vascular access site complications.
Conclusion
This was the first prospective randomized controlled study comparing a fluoroscopically guided puncture technique using predetermined landmarks vs. the conventional palpatory method to puncture the femoral artery. The study compared the rate of complications between the two methods with respect to risk factors like history of hypertension, diabetes, smoking, gender and increased WHR. The overall rate of complications(minor and major) was lower in the fluoroscopy guided group compared to conventional group and it was statistically significant (p<0.05) and the same trend was observed in case of major complications. This benefit was conferred due to our ability to hit the safe zone more consistently with the fluoroscopic method. Study findings conclude that this fluoroscopy guided femoral artery puncture technique is a safe, quick and convenient method to reduce vascular access site complications. This technique has particular benefits amongst high risk subjects like patients with increased WHR, diabetics and smokers where such underlying conditions may affect the access and anatomy of the femoral artery. This technique also nullifies the effect of anatomical variations on the rate of vascular access site complications as it ensures the presence of bony prominence in the form of head of femur behind the puncture site in the majority of cases thereby ensuring reliable hemostasis in an overwhelming majority of patients thereby reducing major complication rates in the intervention group to 0.5%. The technique was easy to master and execute, for entry level operators and the results were highly reproducible.
In an era of radial dominance, this simple, easy-to-master technique should help beginners in decreasing the number of access site complications.
In an era of radial dominance, this simple, easy-to-master technique should help beginners in decreasing the number of access site complications.