Lots of interesting abstracts and cases were submitted for TCTAP 2021 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don’t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
TCTAP A-021
Presenter
Hendy Bhaskara Perdana Putra
Authors
Hendy Bhaskara Perdana Putra1, Ragil Nur Rosyadi1, Benny Jovie1, Richardus Rukma Juslim1, Tjatur Bagus Gunarto1, Tony Elia Parengkuan1
Affiliation
Dr. Ramelan Navy Hospital Surabaya, Indonesia1
View Study Report
TCTAP A-021
Bifurcation/Left Main Diseases and Intervention
Safety and Efficacy of Two–stent Strategy Versus One–stent Strategy for Bifurcation Lesion: Meta-analysis with Time Frame Follow Up
Hendy Bhaskara Perdana Putra1, Ragil Nur Rosyadi1, Benny Jovie1, Richardus Rukma Juslim1, Tjatur Bagus Gunarto1, Tony Elia Parengkuan1
Dr. Ramelan Navy Hospital Surabaya, Indonesia1
Background
In the last two decades, the optimal revascularization strategy for bifurcation lesion remains discourse. Several studies have been generated. However, the results remain contradicting. Our meta-analysis aimed to evaluate safety and efficacy between two-stent and one-stent strategy for bifurcation lesion.
Methods
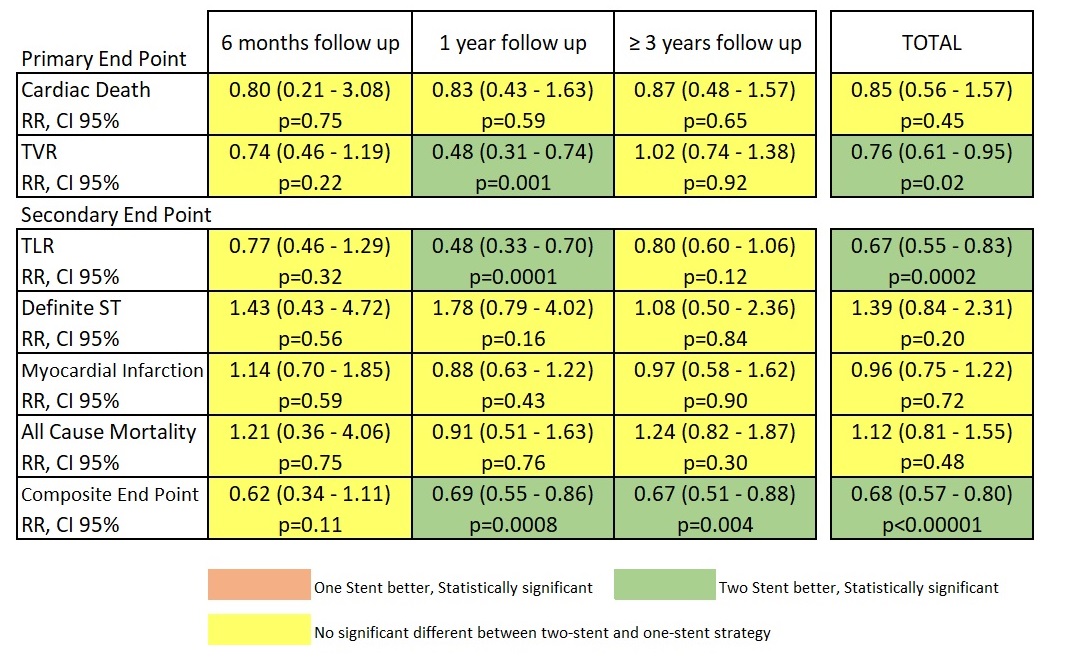
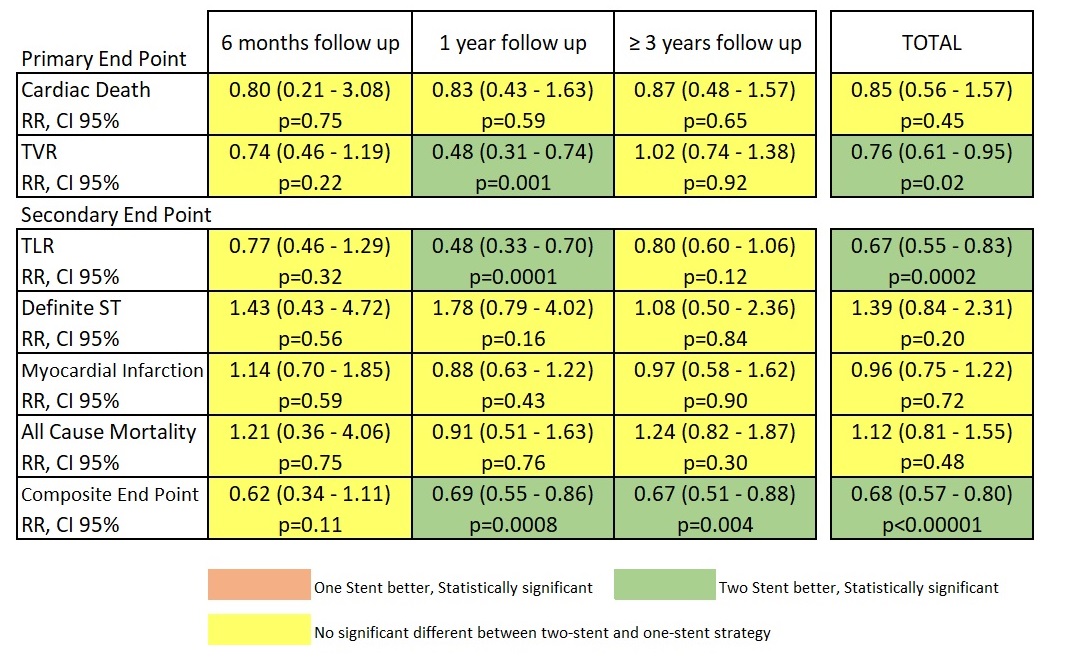
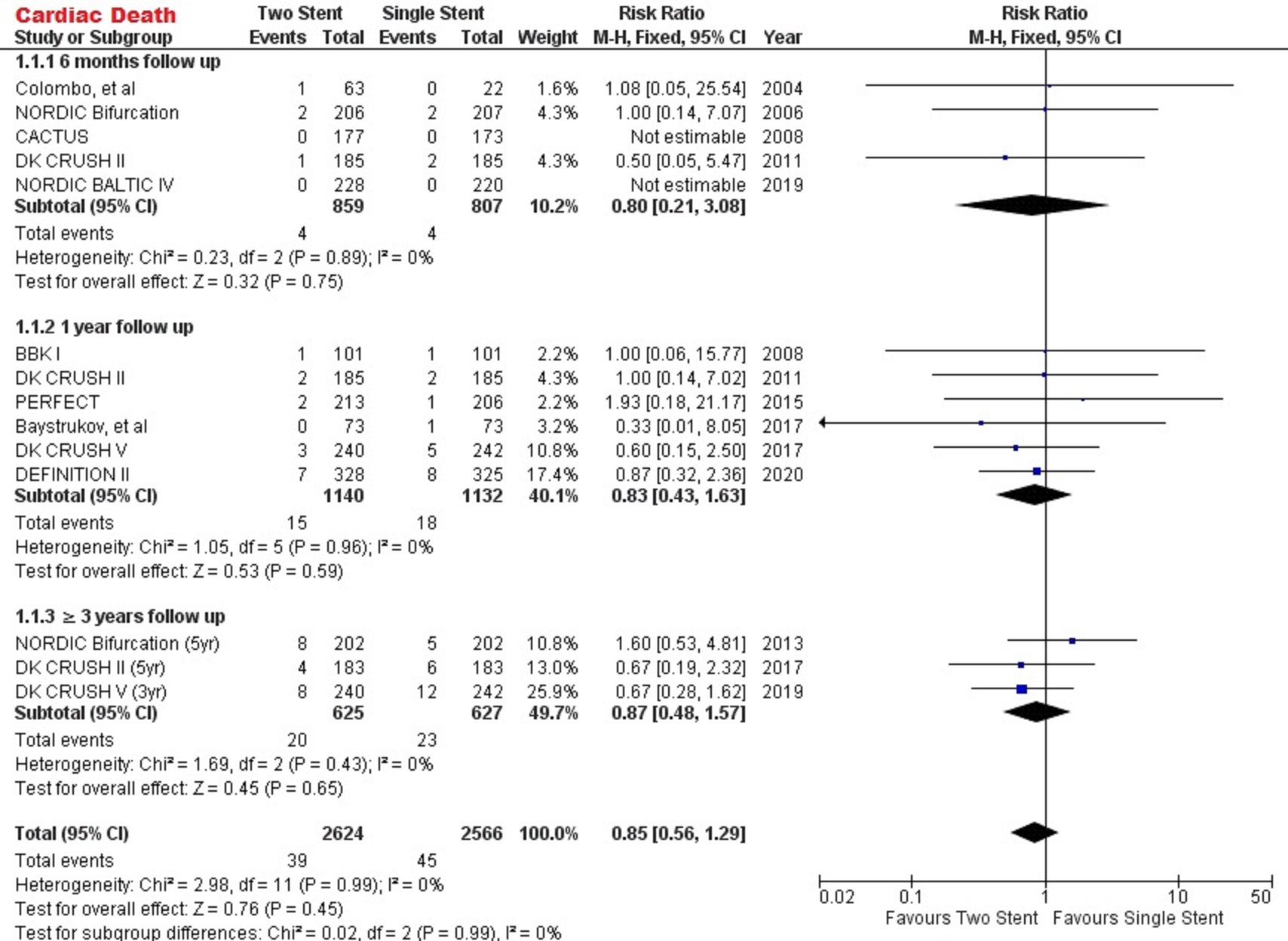
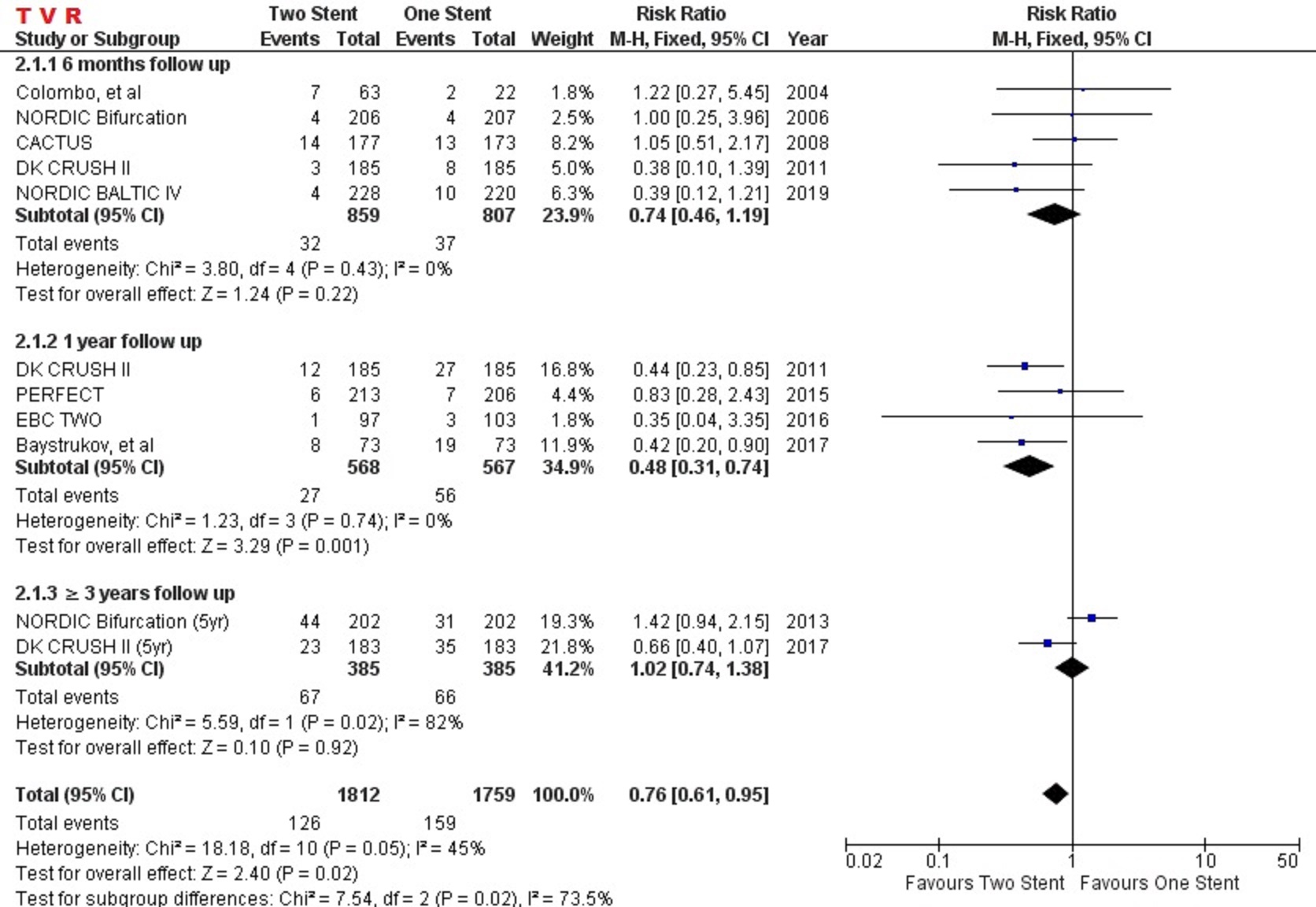
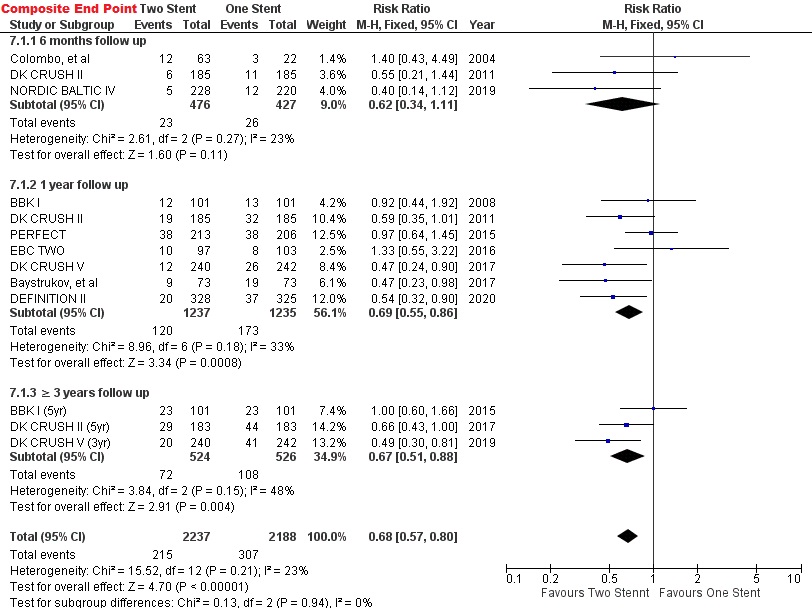
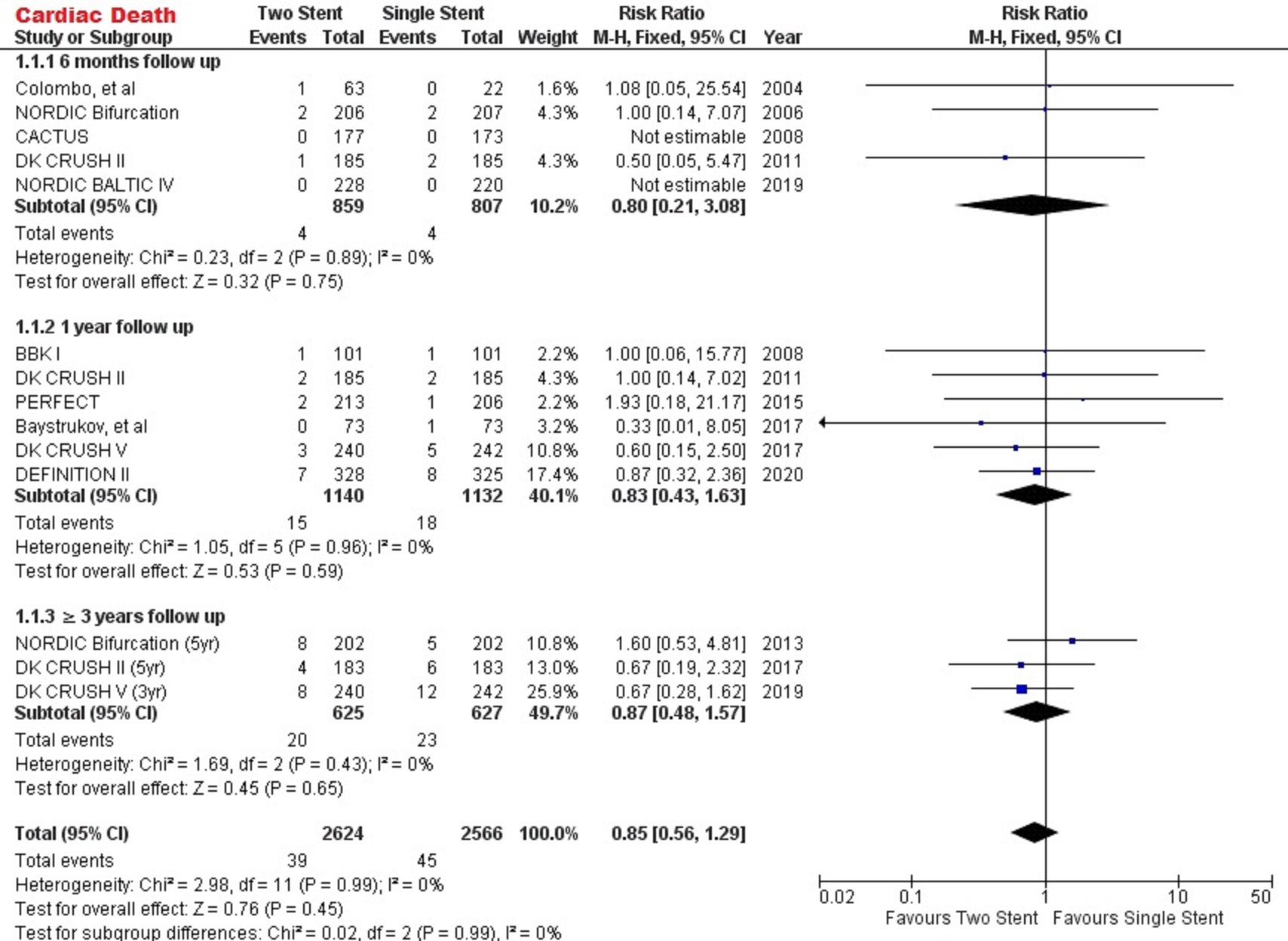
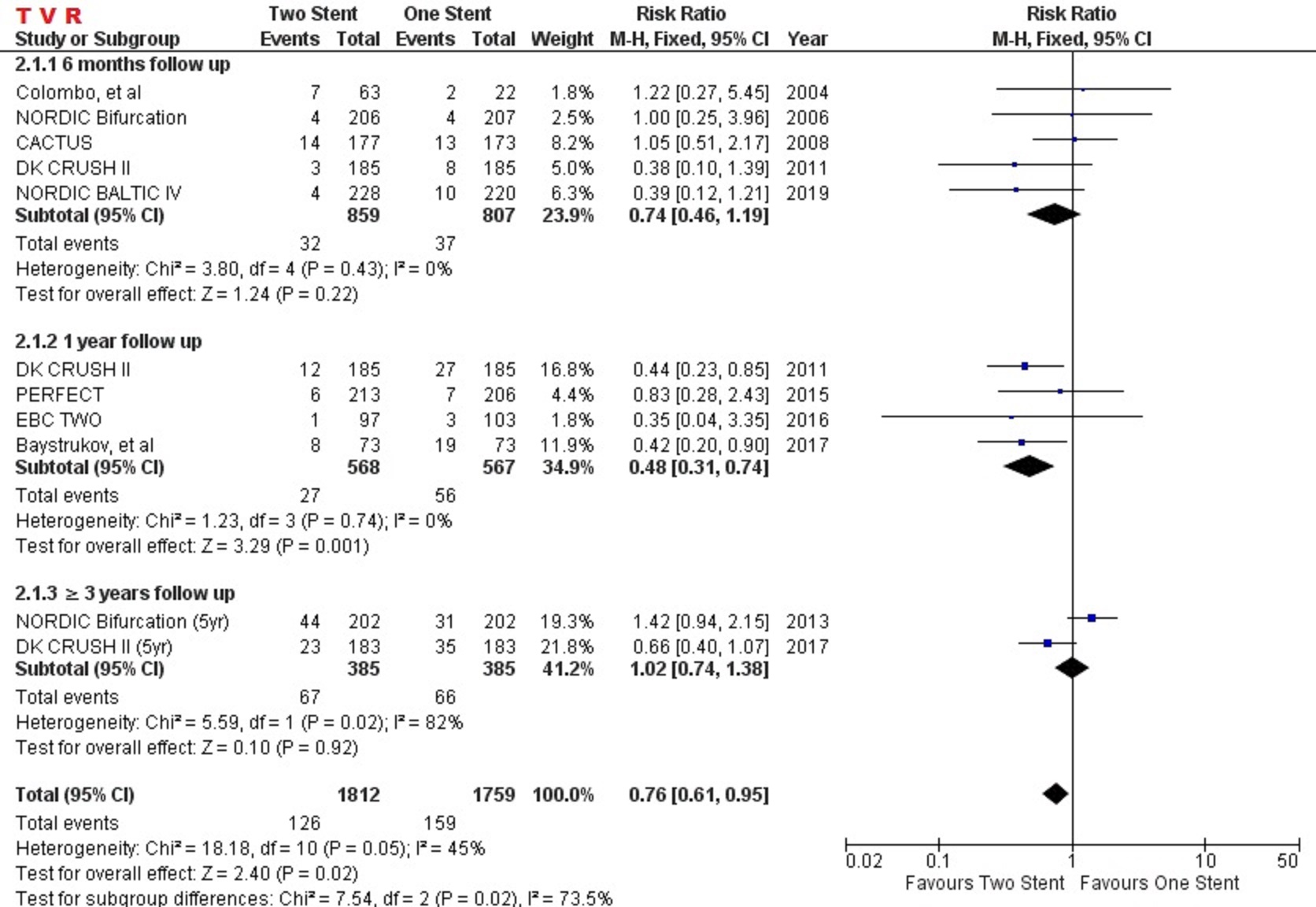
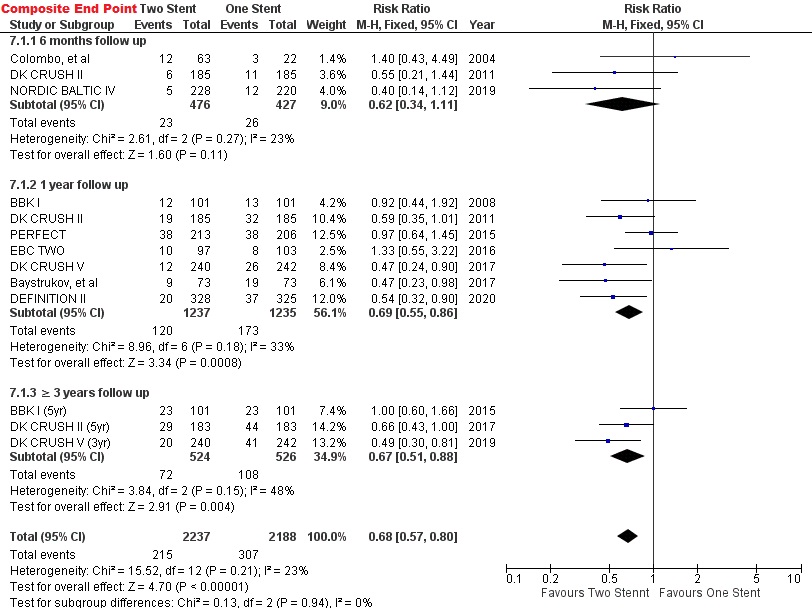
A systematic literature search of several electronic databases was performed. Inclusion criteria were randomized clinical trial and comparing one-stent and any two-stent strategy. The primary endpoint was cardiac death and target vessel revascularization (TVR). Secondary endpoints included target lesion revascularization (TLR), definite stent thrombosis, myocardial infarction (MI), all-cause mortality, and composite endpoint (MACE/TLF). The period of follow-up included: 6 months, 1-year, and ≥ 3-year follow up. Risk ratio and 95% confidence interval (CI) were calculated with fixed or random-effects model as appropriate.
Results
A total of 11 RCT were selected, with 3.622 patients were pooled in our analysis. After 3-year of follow-up, one-stent and two-stent strategy had a similar outcome in cardiac death (RR=0.87 [95% CI, 0.48-1.57], p=0.65) and TVR (RR=1.02 [95% CI, 0.74-1.38], p=0.92). However, two-stent strategy had an opportunity to decrease the risk of TVR and TLR in the 1-year by 52% (RR:0.48 [95% CI, 0.31-0.74], p=0.001) and (RR:0.48 [95% CI, 0.33-0.70], p=0.0001). Two-stent strategy also significantly reduced the risk of composite endpoint (MACE/TLF) in 1-year (RR:0.69 [95% CI, 0.55-0.86], p=0.0008) and after 3-year (RR:0.67 [95% CI, 0.51-0.88], p=0.004) follow-up.The other endpoints (definite stent thrombosis, MI, and all-cause mortality) were comparable between one-stent and two-stent strategy during 6-month, 1-year, and more than 3-year follow-up.
Conclusion
Safety and efficacy between one-stent and two-stent strategy were comparable. However, two-stent strategy has shown consistency in reducing the risk of composite endpoint (MACE/TLF) in 1-year and after 3-year follow-up.