Lots of interesting abstracts and cases were submitted for TCTAP 2021 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don’t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
TCTAP A-043
Presenter
Cheng-Wei Liu
Authors
Cheng-Wei Liu1, Min-I Su2
Affiliation
Tri-Service General Hospital, Taiwan1, Mackay Memorial Hospital, Taiwan2
View Study Report
TCTAP A-043
Peripheral Vascular Disease and Intervention
Neutrophil-to-Lymphocyte Ratio Associated with an Increased Risk of Mortality in Patients with Critical Limb Ischemia
Cheng-Wei Liu1, Min-I Su2
Tri-Service General Hospital, Taiwan1, Mackay Memorial Hospital, Taiwan2
Background
The neutrophil-to-lymphocyte ratio(NLR) is associated with poor prognoses in cancer and peripheral artery disease patients. Its association with mortality has not been comprehensively explored in critical limb ischemia(CLI) patients. We investigated the association between the NLR and clinical outcomes in CLI patients.
Methods
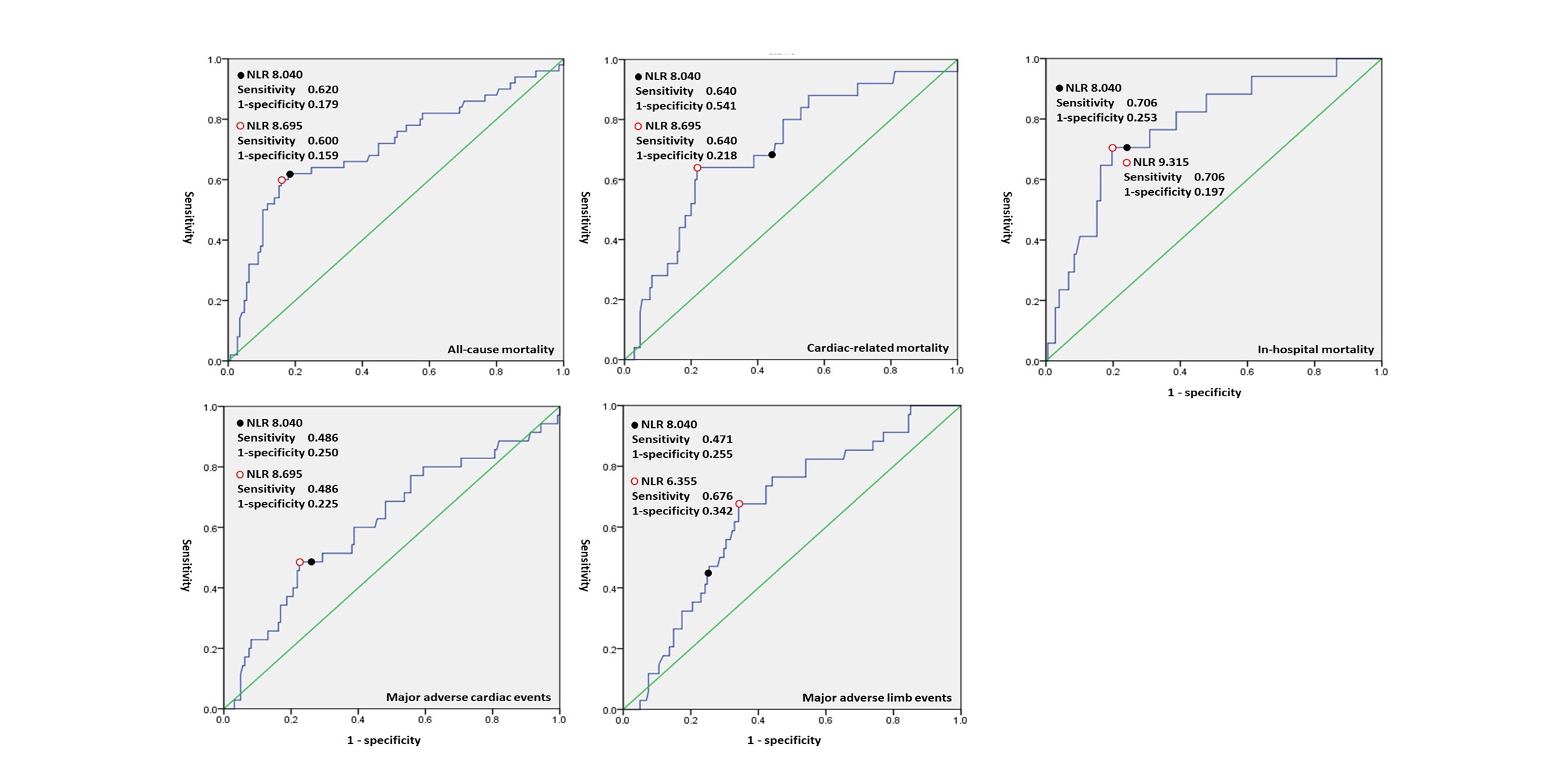
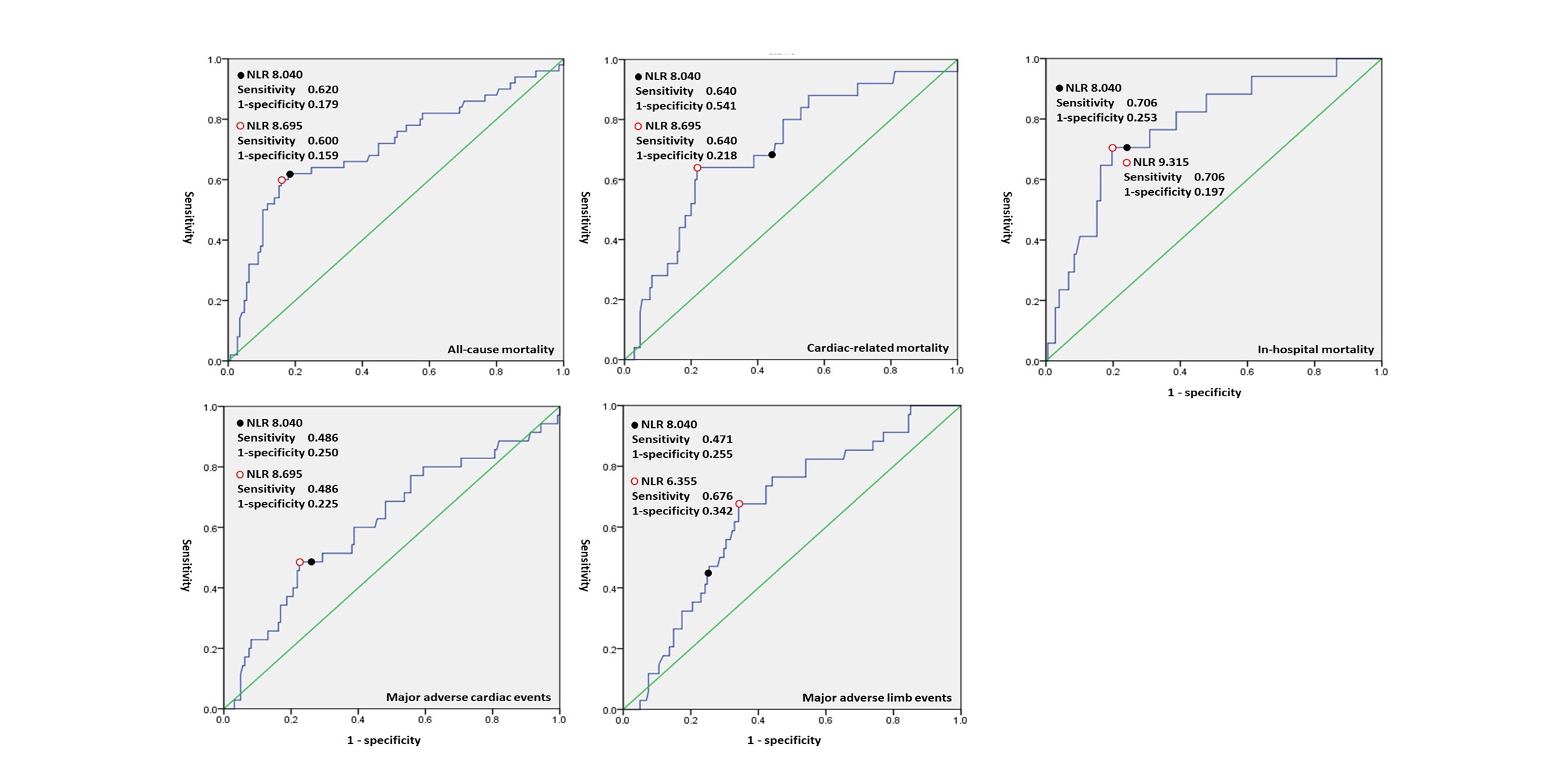
We retrospectively enrolled consecutive CLI patients between 1/1/2013 and12/31/2018. Receiver operating characteristic curve analysis determined the NLRcut-offs for study outcomes, namely, 1-year in-hospital, all-cause, cardiac-related mortality, and major adverse cardiovascular events(MACEs); and major adverse limb events(MALEs).
Results
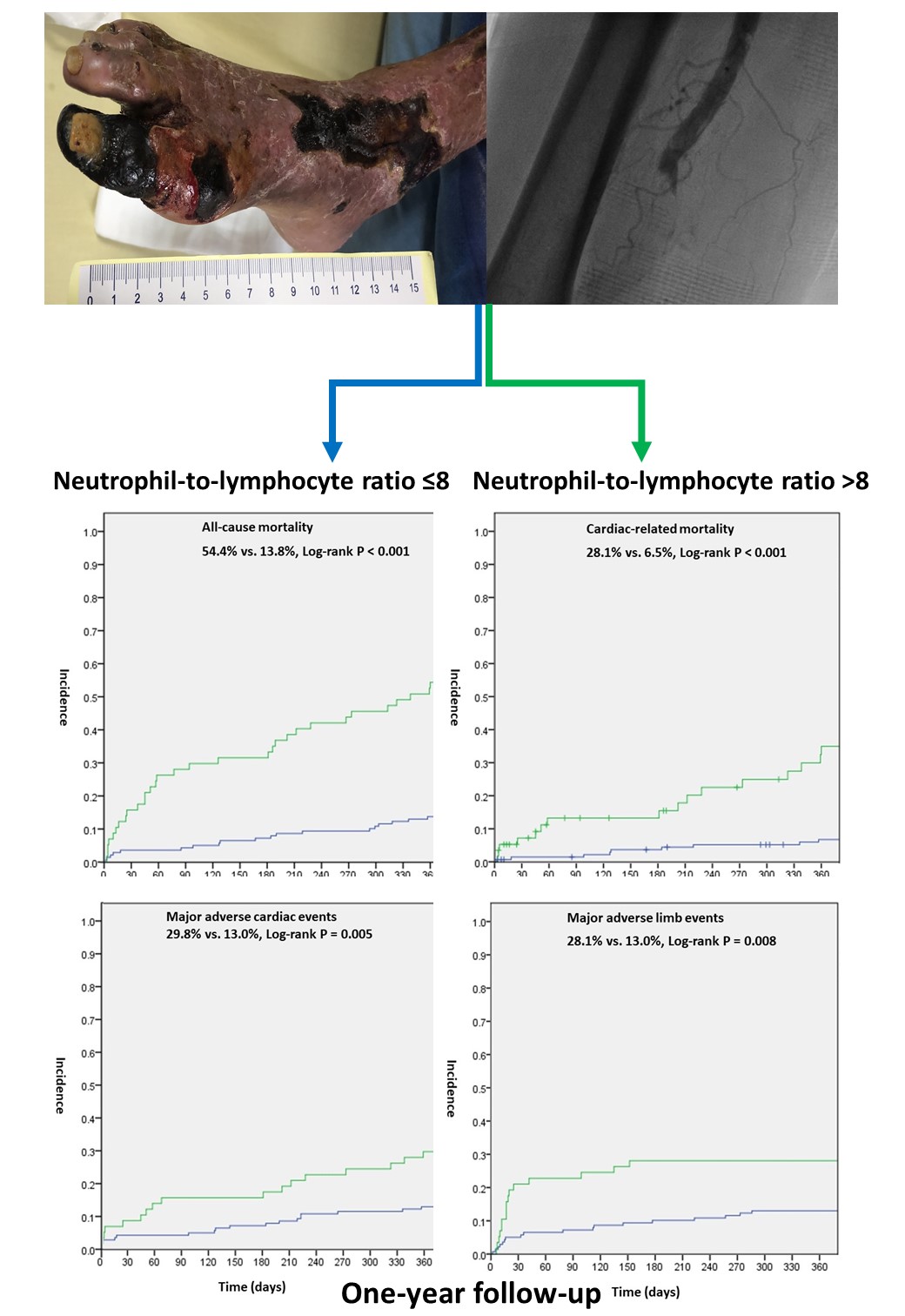
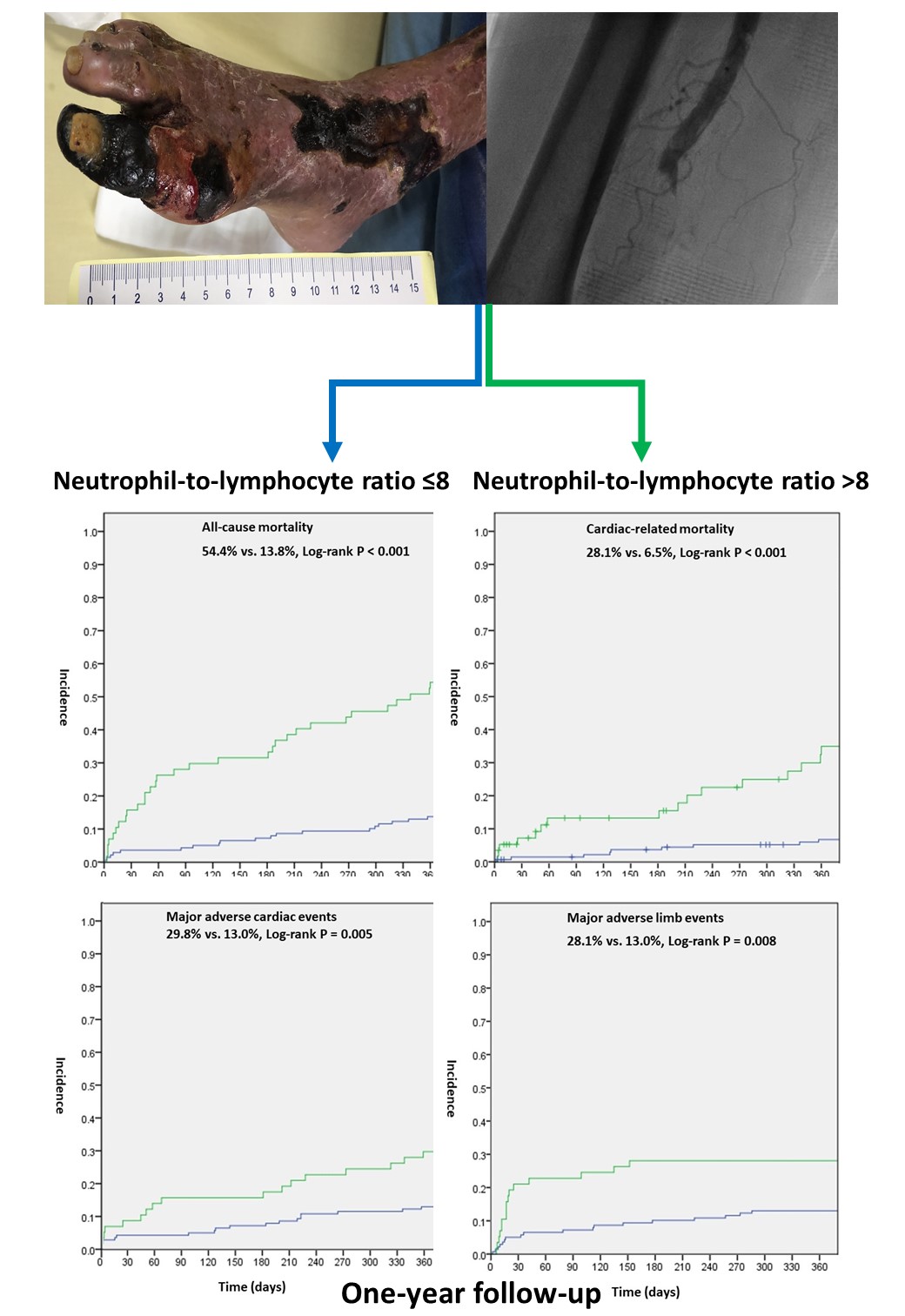
Among 195 patients (age, 74.0 years, SD: 11.5; 51.8% male; body mass index, 23.4 kg/m2, SD: 4.2), 14.4% exhibited acute limb ischemia. After 1 year, patients with a NLR>8 had higher in-hospital mortality (21.1%vs. 3.6%, P<0.001), all-cause mortality (54.4% vs. 13.8%, P < 0.001),cardiac-related mortality (28.1% vs. 6.5%, P<0.001), MACE (29.8% vs. 13.0%,P=0.008), and MALE (28.1% vs. 13.0%, P=0.021) rates than those with a NLR<8. In multivariate logistic regression, NLR ≥8 was significantly associated with all-cause (P<0.001) andcardiac-related (adjusted HR: 5.286, 95% CI: 2.075-13.47, P<0.001)mortality, and NLR ≥6 was significantly associated with MALEs (adjusted HR: 2.804, 95% CI: 1.292-6.088,P=0.009). Each increase in the NLR increased all-cause (adjusted HR: 1.028, 95%CI: 1.008-1.049, P=0.007) and cardiac-related (adjusted HR:1.027, 95%CI:0.998-1.057, P=0.073) mortality. The NLR was not significantly associated with in-hospital mortality or MACEs.
Conclusion
CLI patients with high NLRs had significantly higher risks of 1-year all-cause and cardiac-related mortality and MALEs. The NLR can be used for prognostic prediction in these patients.


