Lots of interesting abstracts and cases were submitted for TCTAP 2021 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don’t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
TCTAP A-003
Presenter
Hashrul Rashid
Authors
Hashrul Rashid1, Michael Michail2, Abdul Rahman Ihdayhid2, Jasmine Chan2, Nancy Khav2, Sean Tan2, Arthur Nasis3, James Cameron3, Stephen Nicholls3, Rob Gooley3
Affiliation
Monash University, Australia1, Monash Health and Monash University, Australia2, MonashHeart and Victorian Heart Institute, Australia3
View Study Report
TCTAP A-003
Valvular Intervention: Aortic
Prosthesis Geometrical Predictors of Leaflet Thrombosis following Transcatheter Aortic Valve Replacement with Intra-annular Prostheses
Hashrul Rashid1, Michael Michail2, Abdul Rahman Ihdayhid2, Jasmine Chan2, Nancy Khav2, Sean Tan2, Arthur Nasis3, James Cameron3, Stephen Nicholls3, Rob Gooley3
Monash University, Australia1, Monash Health and Monash University, Australia2, MonashHeart and Victorian Heart Institute, Australia3
Background
Leaflet thrombosis (LT) following transcatheter aortic valve replacement (TAVR) is a recognised entity. The association between prosthesis geometry [expansion, implant depth and commissural alignment (CA)] with LT is unclear.
Methods
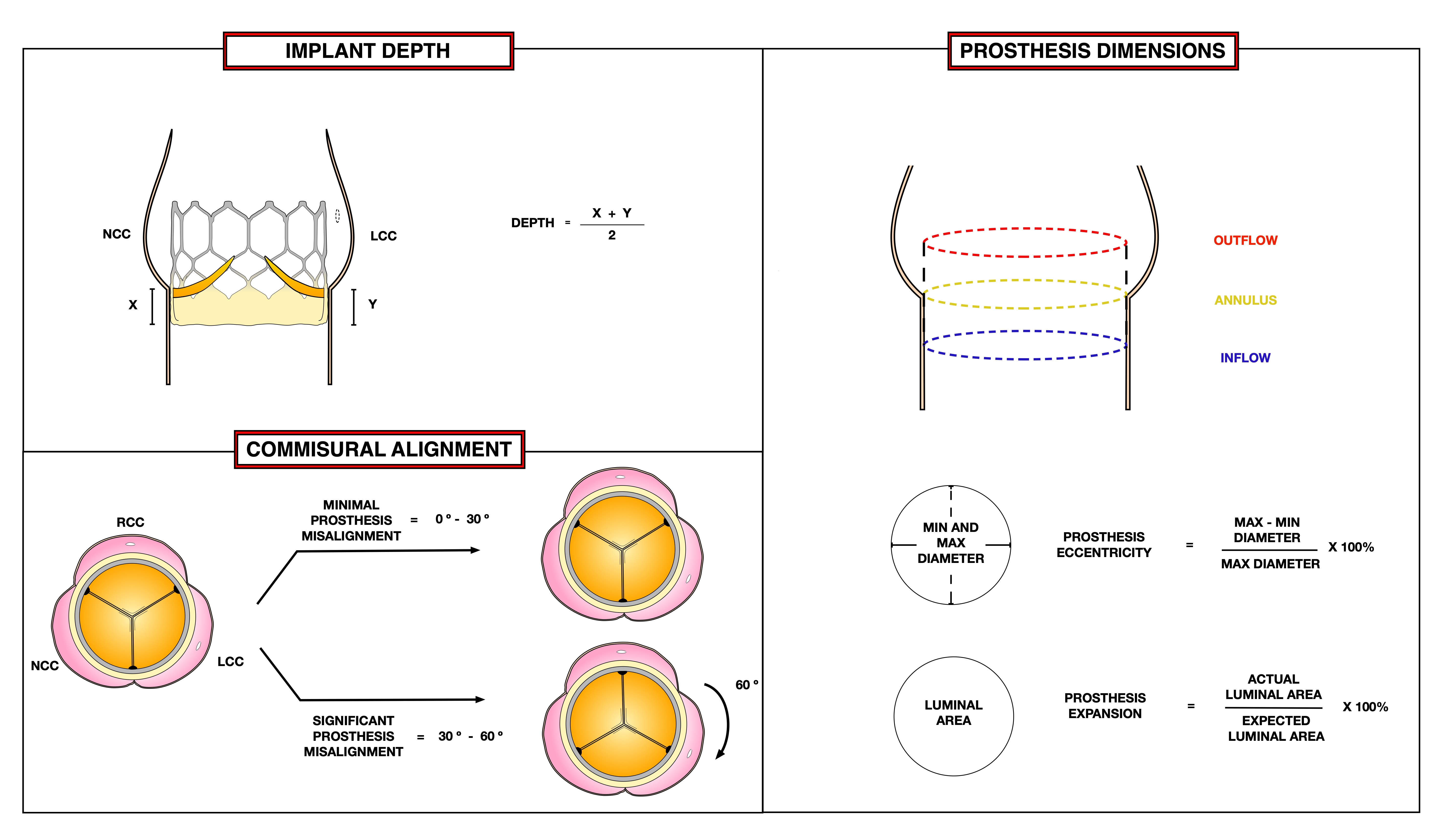
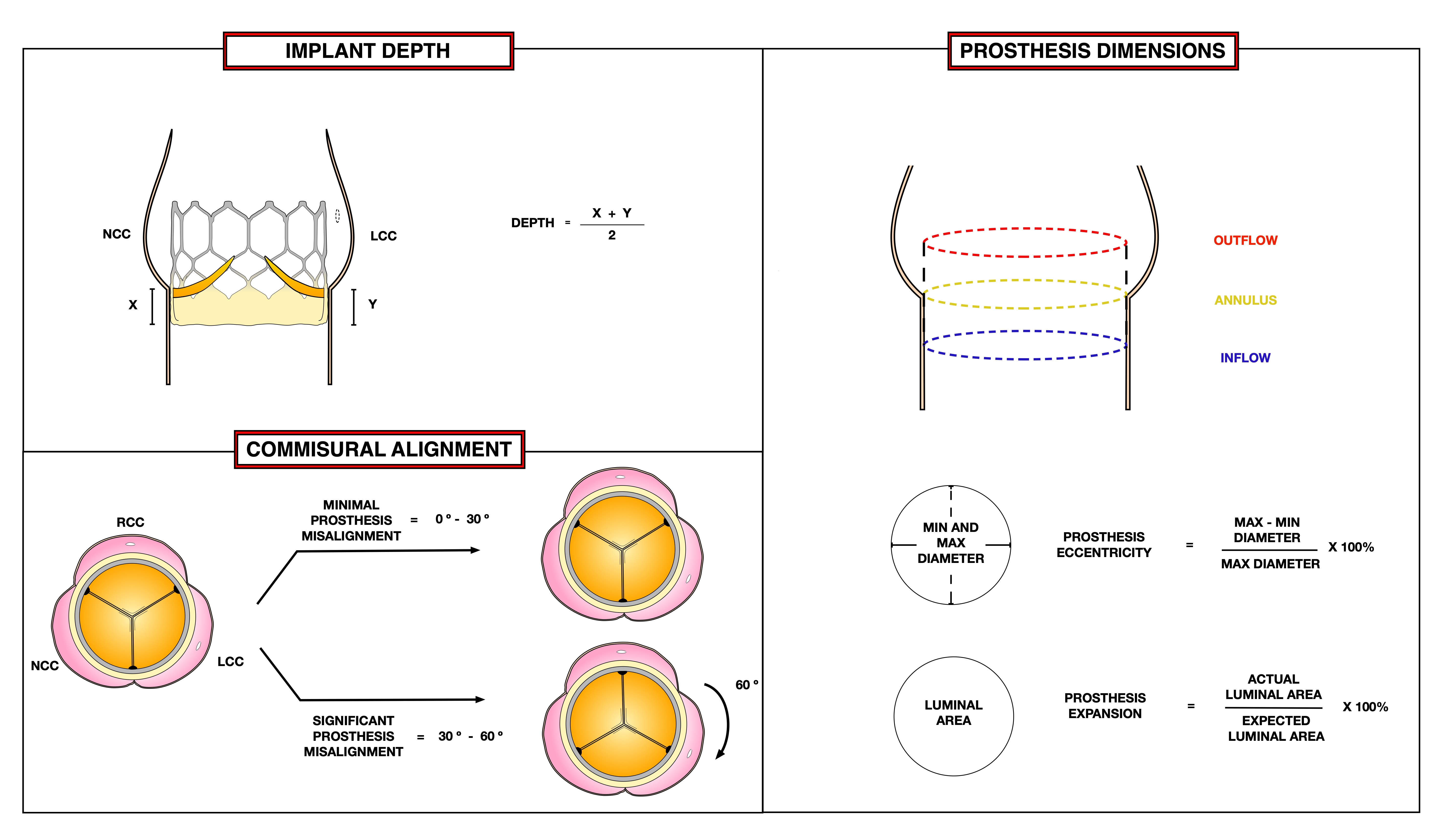
Patients that received an intra-annular TAVR prosthesis and prospectively planned post-procedural computed tomography (CT) with a 320-slice scanner were included. LT, defined as at least 50% restricted leaflet motion, was assessed with a dedicated 3Mensio workstation by two experienced CT readers. Prosthesis expansion and eccentricity was measured at prosthesis inflow, annulus and outflow. Prosthesis misalignment was defined as CA, the average angle deviation between native and prosthesis leaflet commissure, greater than 30°.
Results
Prevalence of LT was 13.7% in 117 patients [13/93 cases (14.0%) for Lotus valves and 3/24 cases (12.5%) for Sapien 3 valves]. None of the patients with LT were on anticoagulation therapy (0.0% vs 22.7%, p<0.01). Other baseline and procedural characteristics were similar in both groups. There were no differences in prosthesis area or eccentricity at any prosthesis level. Patients with LT had reduced annulus expansion (89.4±5.2% vs 97.0±4.4%, p<0.01), greater prosthesis misalignment (81.3% vs 48.5%, p=0.02) and deeper implant depths (6.3±1.7mm vs 4.3±1.5mm, p<0.01). On ROC analysis, implant depth of 5.7mm was the best cut-off for the occurrence of LT (AUC = 0.81). On multivariate analysis, predictors of LT were annulus under-expansion (Odds ratio [OR] 1.4; 95% confidence interval [CI] 1.2–1.7, p=0.03), prosthesis misalignment (OR 6.8; 95%CI 1.1–45.5, p=0.04) and implant depth (OR 1.9; 95%CI 1.1–3.2 , p=0.03). Anticoagulation therapy was a protective factor for LT (OR 0.2; 95%CI 0.1–0.4, p<0.01).
Conclusion
Geometrical prostheses predictors of LT were reduced annulus expansion, lower implant depth and greater prosthesis misalignment. Implant depth of 5.7mm was the optimal cut-off for the occurrence of LT. Anticoagulation therapy was a protective factor for LT. These factors may be important considerations during procedural planning for TAVR.


