
Seung-Jung Park
Asan Medical Center, Korea (Republic of)
At TCTAP 2025, during the "Bifurcation PCI: New Concept and Approaches" session, Dr. Seung-Jung Park (Asan Medical Center, Korea) delivered a lecture redefining the approach to bifurcation PCI in the wake of the ISCHEMIA study. Focusing on both non-left main (non-LM) and left main (LM) bifurcation lesions, he emphasized that these two entities demand fundamentally different strategies—simplification for the former, and individualized precision for the latter. His message for non-LM bifurcation was clear and bold: Ī░DonĪ»t touch small side branches.Ī▒
Citing results from the ISCHEMIA trial and subsequent meta-analyses, Dr. Park emphasized that percutaneous coronary intervention (PCI) confers no survival advantage over optimal medical therapy (OMT) in stable ischemic heart disease—even in patients with multivessel disease or severe ischemia. This shift in philosophy calls for a more judicious and physiology-driven approach to PCI, especially in bifurcation settings.
In non-LM bifurcations, over 80% of side branches were found to supply less than 10% of the myocardial mass. These "small" branches—defined as those with a reference vessel diameter <2.5 mm—contribute minimally to ischemic burden and can be safely ignored during intervention. Ī░Small side branches should not be stented, regardless of angiographic stenosis,Ī▒ Dr. Park stated. Instead, main branch stenting alone often suffices, aligning with the minimalist strategy backed by physiologic and anatomic rationale.
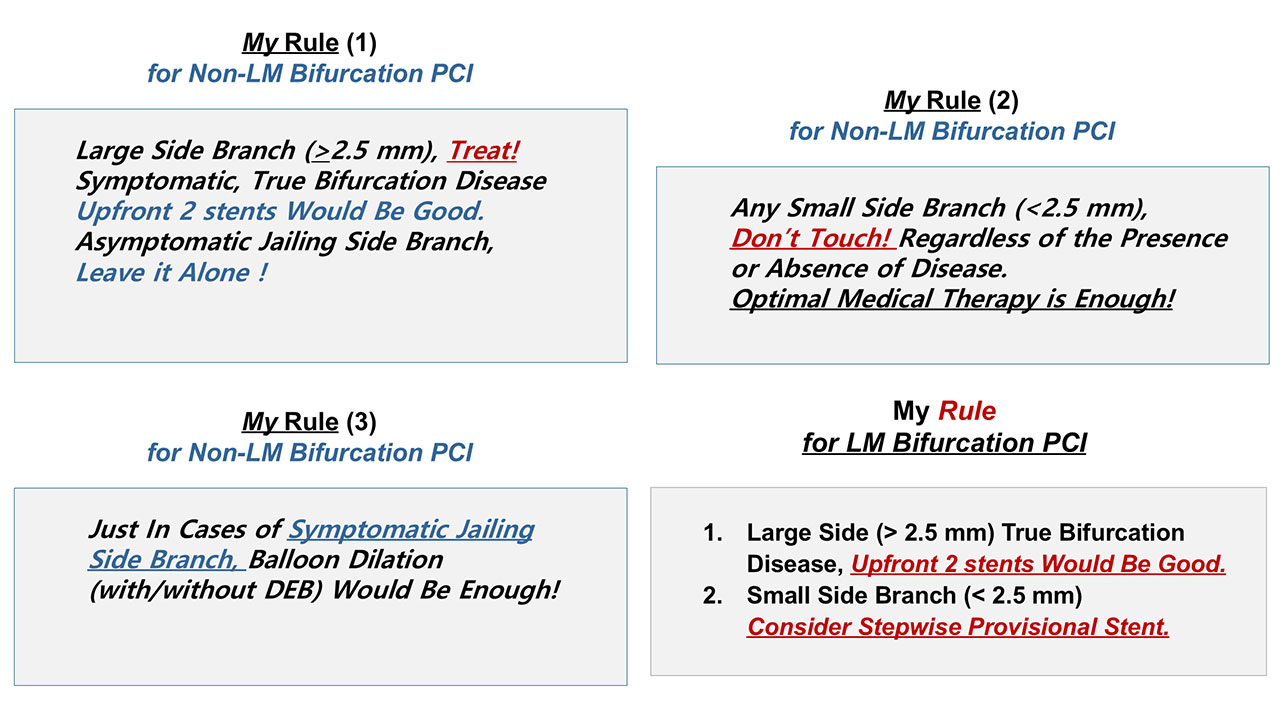
Conversely, for large side branches (>2.5 mm)—especially in true bifurcation lesions (Medina 1,1,1 or 0,1,1)—he advocated upfront two-stent strategies. Still, Dr. Park underscored that unnecessary treatment of jailed side branches, even when angiographically narrowed, should be deferred unless functionally significant.
For LM bifurcations, Dr. Park clarified that a separate strategy is warranted. Unlike non-LM lesions, LM disease often involves larger branches with substantial myocardium at risk. Here, intravascular imaging and FFR play pivotal roles in guiding one- versus two-stent strategies. When the left circumflex artery (LCX) is large and disease is truly bifurcated, upfront two-stenting is justified and can reduce the risk of side branch occlusion without compromising outcomes.
Dr. Park concluded by summarizing his clinical rules:
- DonĪ»t touch small side branches (<2.5 mm) in non-LM bifurcations.
- Only treat jailed branches if symptomatic or functionally significant.
- Use upfront two-stenting for large, true bifurcation lesions.
Bifurcation PCI: New Concept and Approaches
Friday, April 25, 2:00 PM-4:00 PM
Presentation Room 2, Level 1
Edited by

Hoyun Kim, MD
Bucheon Sejong Hospital, Korea (Republic of)

