
Jung-Min Ahn
Asan Medical Center, Korea (Republic of)
In the Ī░TAVR: Current Status and Future PerspectiveĪ▒ session at TCTAP 2025, Dr. Jung-Min Ahn (Asan Medical Center, Korea) presented a comprehensive lecture on transcatheter aortic valve replacement (TAVR) in patients with bicuspid aortic valve (BAV), addressing the key anatomical, procedural, and clinical challenges that distinguish BAV from the more commonly studied tricuspid aortic valve.
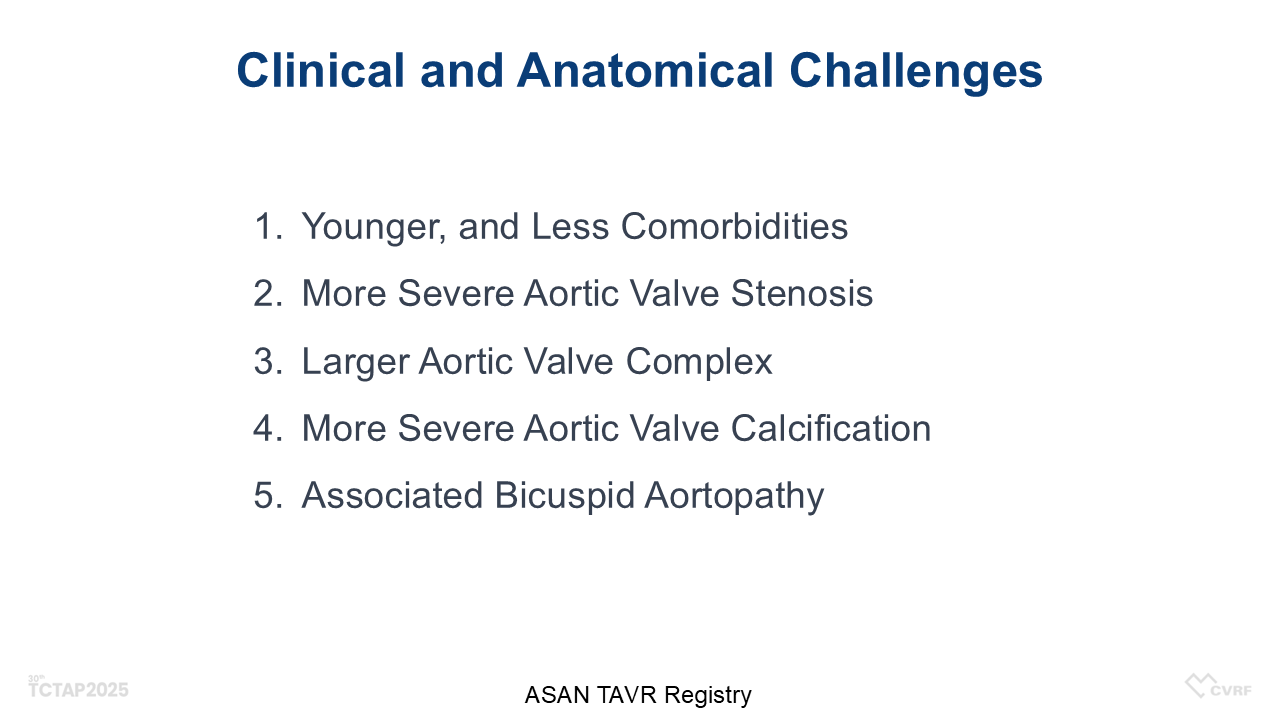
Although early randomized trials in TAVR excluded BAV patients due to their complex anatomy, recent evidence—including results from PARTNER III and other contemporary registries—has supported TAVRĪ»s effectiveness even in low-risk populations. Notably, the average patient age in current TAVR cohorts has decreased from 82–84 years in early trials to around 74 years today, increasing the prevalence of BAV cases encountered in real-world practice. BAV patients are typically younger, more often male, and have fewer comorbidities. However, their anatomical profile is more challenging: severe aortic stenosis with higher transvalvular gradients, larger and more asymmetric valve complexes, and substantially greater calcification volume compared with tricuspid aortic stenosis. These features raise both periprocedural and long-term risks, necessitating a more cautious approach to valve sizing and deployment.
The Asan Medical Center data demonstrated that in BAV cases, operators more frequently performed both pre- and post-dilatation and tended to implant larger valves than in tricuspid cases. Despite these differences, echocardiographic outcomes—including effective orifice area and transvalvular gradients—were similar at two-year follow-up. Rates of death and stroke were also comparable.
To better understand the safety and efficacy of TAVR in BAV patients, Dr. Ahn presented results from a comprehensive meta-analysis comparing outcomes between BAV and TAV aortic stenosis patients. Among over 13,000 patients from 34 studies, procedural complications were significantly more frequent in BAV TAVR recipients. Notably, the risk of moderate-or-worse paravalvular leakage was increased by 59%, while the rate of permanent pacemaker implantation showed no significant difference. However, aortic root injury occurred 81% more often in BAV cases. Major bleeding rates were comparable between the two groups.
Furthermore, the meta-analysis identified a small but statistically significant increase in early adverse events in BAV patients: the 30-day mortality risk was elevated by 34%, and the risk of stroke increased by 27% compared to TAV patients. These findings underscore the importance of anatomical assessment and individualized procedural strategies in BAV TAVR.

Dr. Ahn concluded, Ī░While BAV remains a complex entity, TAVR has proven to be both feasible and effective, but requires individualized planning with careful attention to anatomy, calcium distribution, and valve sizing.Ī▒ This session emphasized the critical role of imaging-guided, anatomy-specific strategies in optimizing TAVR outcomes for this unique and increasingly encountered patient population.
TAVR: Current Status and Future Perspective
Saturday, April 26, 9:50 AM-11:10 AM
Coronary Theater, Level 1
Edited by

Jinho Lee, MD
Kyung Hee University Medical Center, Korea (Republic of)
