
Jung-Min Ahn
Asan Medical Center, Korea (Republic of)
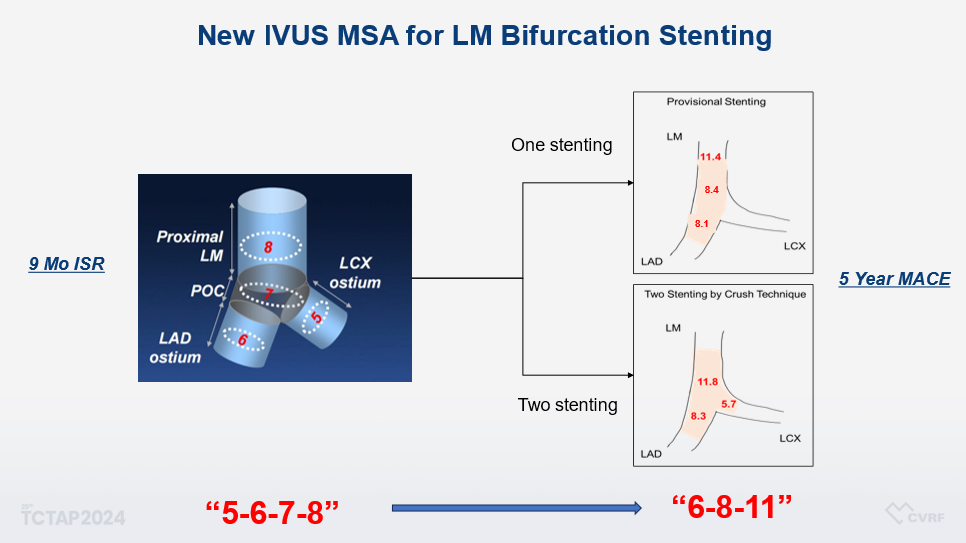
At the TCTAP 2025 Hot Topics session, Professor Jung-Min Ahn of Asan Medical Center presented a transformative lecture titled Ī░Rule of 6-8-11 for Left Main Upfront 2-Stenting,Ī▒ unveiling a novel, intravascular ultrasound (IVUS)-based framework to guide percutaneous coronary intervention (PCI) in unprotected left main (LM) bifurcation disease. Drawing on a wealth of institutional experience bolstered by new long-term data, Prof. Ahn proposed the Ī░6-8-11Ī▒ rule—a clinically validated evolution of the earlier Ī░5-6-7-8Ī▒ guideline.
He began by tracing the evolution of LM revascularization from coronary artery bypass grafting (CABG) to PCI, referencing key evidence from the MAIN-COMPARE registry and the 10-year results of the PRECOMBAT trial. These findings, showing comparable mortality between PCI and CABG, have redefined the role of PCI in complex LM anatomy.
Prof. Ahn then shifted focus to what he termed the Ī░next frontierĪ▒ in LM intervention: optimization through imaging-defined minimal stent area (MSA). Citing long-term data, including recently published findings in Circulation: Cardiovascular Interventions (2024), he demonstrated that IVUS-derived MSAs at three critical segments—the distal LM, left anterior descending (LAD) ostium, and left circumflex (LCX) ostium—are linearly correlated with the risk of major adverse cardiac events (MACE) over five years. Specifically, under-expansion below 11.8 mm®„ in the distal LM, 8.3 mm®„ in the LAD ostium, and 5.7 mm®„ in the LCX ostium was significantly associated with increased long-term risk. In contrast, the simplified Ī░5-6-7-8Ī▒ thresholds demonstrated limited prognostic discrimination. These findings, Prof. Ahn argued, underscore the need to move beyond angiographic benchmarks toward outcome-driven, segment-specific targets—the foundation of the Ī░6-8-11Ī▒ rule.
Turning to real-world application, Prof. Ahn outlined how these targets can be systematically incorporated into contemporary two-stent strategies, particularly in crush and DK-crush techniques. He emphasized that achieving Ī├8 mm®„ in the LAD ostium and Ī├6 mm®„ in the LCX ostium should not be aspirational but mandatory procedural endpoints. Failure to meet these thresholds, he warned, may predispose patients to ischemic complications, target lesion revascularization, or mortality. Ī░IVUS-first, optimize always,Ī▒ he declared, advocating a fundamental shift in operator mindset.
Adding further weight to the argument, Prof. Ahn presented newly analyzed data from 829 patients who underwent IVUS-guided single-stent crossover LM PCI at Asan Medical Center. The analysis identified optimal MSA cutoffs of 11.4 mm®„ for the proximal LM, 8.4 mm®„ for the distal LM, and 8.1 mm®„ for the LAD ostium in predicting 5-year MACE. Notably, under-expansion in the proximal LM was associated with an almost twofold increase in adverse events. In contrast, simultaneous under-expansion in the distal LM and LAD ostium conferred even higher risk. These results reinforce the critical value of segment-specific MSA targets and validate IVUS as a tool for imaging and precision-guided intervention.
Prof. Ahn concluded with a compelling message: Ī░It is not enough to simply implant a stent. What matters is how well you implant it.Ī▒ He emphasized that imaging alone does not improve outcomes unless used to guide optimization. He proposed that the Ī░6-8-11Ī▒ rule offers a simple yet evidence-based algorithm to elevate the standard of care in LM bifurcation PCI.
As bifurcation strategies grow more sophisticated, Prof. AhnĪ»s lecture served both as a synthesis of state-of-the-art data and a challenge to the interventional community: to abandon outdated thresholds and embrace a new era of precision PCI. Anchored in long-term clinical outcomes, the Ī░6-8-11Ī▒ rule is poised to become a cornerstone of modern LM revascularization.
Bifurcation PCI: New Concept and Approaches
Friday, April 25, 2:00 PM-4:00 PM
Presentation Room 2, Level 1
Edited by

Ju Hyeon Kim, MD
Asan Medical Center, Korea (Republic of)

