Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-057
Optimizing Complex PCI Outcomes in Calcified Coronary Disease Using Intravascular Imaging
By Muhammad Azlan Aseri, Mohd Aizuddin Mohd Zulastri, Syed Saleh Syed Sheikh, Ahmad Syadi Mahmood Zuhdi, Imran Zainal Abidin
Presenter
Muhammad Azlan Aseri
Authors
Muhammad Azlan Aseri1, Mohd Aizuddin Mohd Zulastri1, Syed Saleh Syed Sheikh1, Ahmad Syadi Mahmood Zuhdi1, Imran Zainal Abidin1
Affiliation
University Malaya Medical Centre, Malaysia1,
View Study Report
TCTAP C-057
Coronary - Complex PCI - Calcified Lesion
Optimizing Complex PCI Outcomes in Calcified Coronary Disease Using Intravascular Imaging
Muhammad Azlan Aseri1, Mohd Aizuddin Mohd Zulastri1, Syed Saleh Syed Sheikh1, Ahmad Syadi Mahmood Zuhdi1, Imran Zainal Abidin1
University Malaya Medical Centre, Malaysia1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
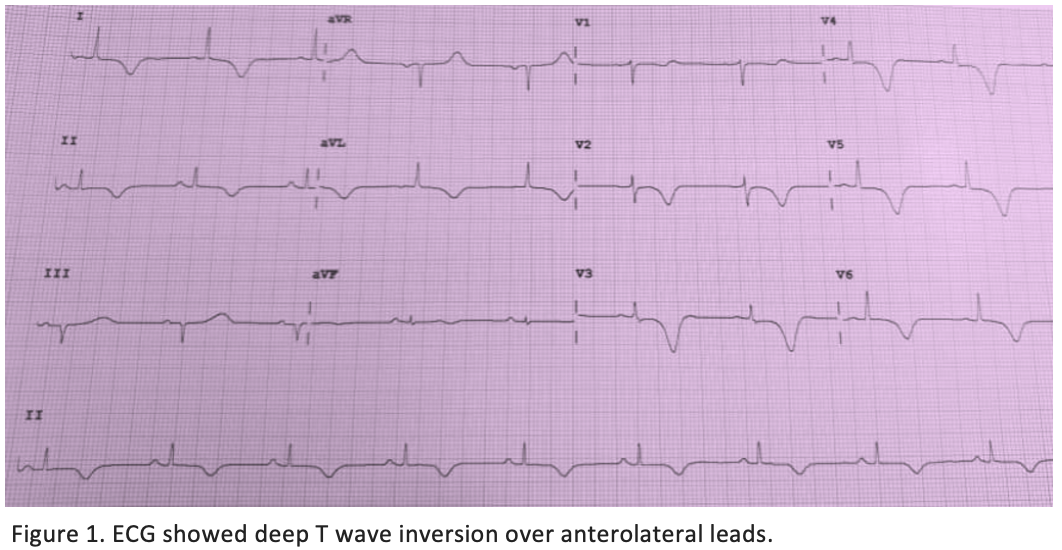
A 63-year-old lady with underlying hypertension and strong family history of ischaemic heart disease (IHD) presented with severe left-sided chest pain associated with palpitation and diaphoresis. Cardiovascular examinations were unremarkable. The electrocardiogram (ECG) showed Wellen type B pattern ( Figure 1). She was diagnosed with Wellens Syndrome and had a coronary angiogram done during admission.
Relevant Test Results Prior to Catheterization
Blood tests revealed normal blood counts, renal function, liver function, and coagulation profiles. High-sensitivity-troponin-I was elevated at 3677 ng/L, indicating significant myocardial injury. Echocardiography demonstrated anterior wall hypokinesia with preserved ejection fraction and normal valves.
Relevant Catheterization Findings
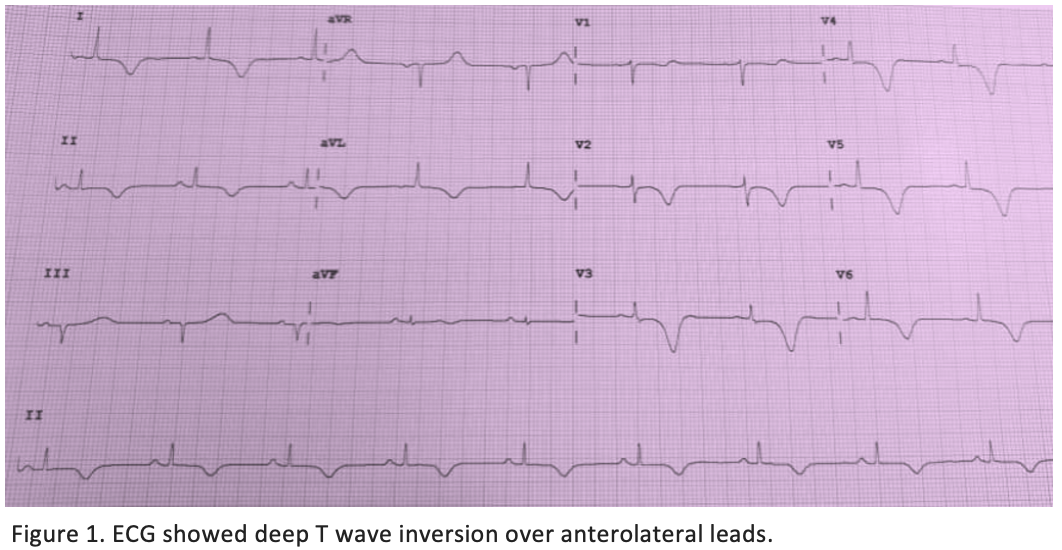
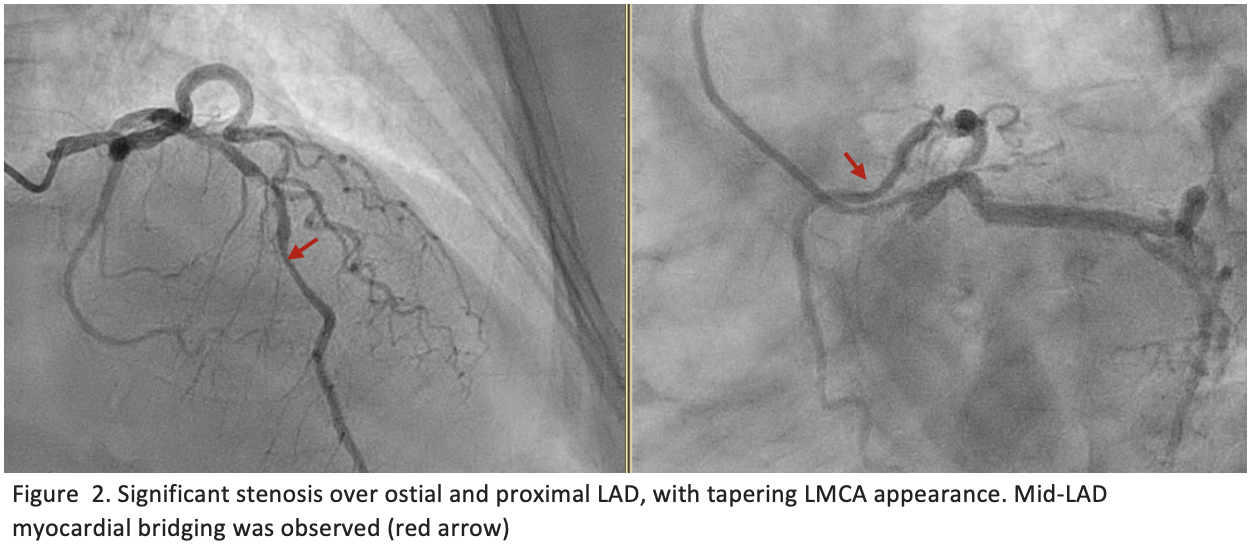
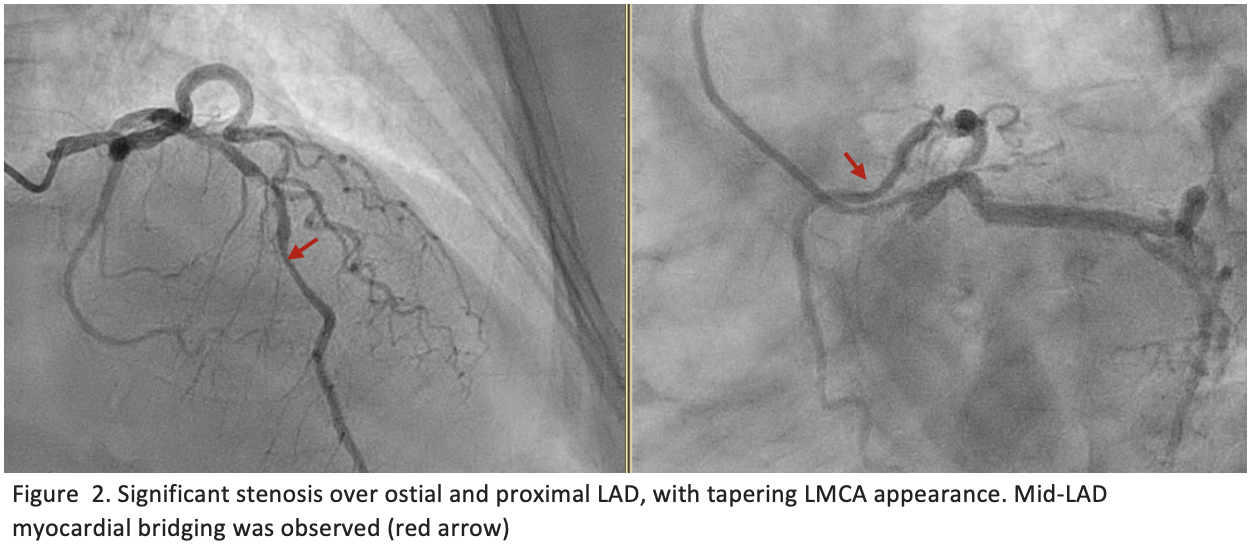
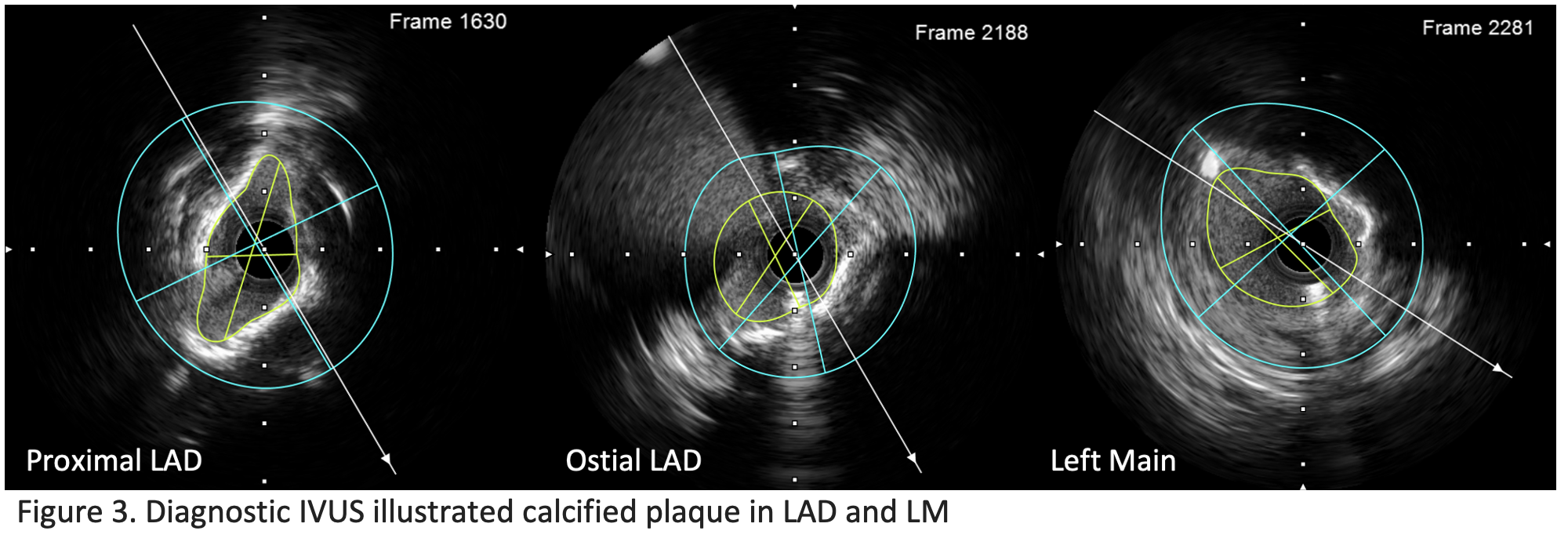
Angiogram (Figure 2) showed calcified proximal left anterior descending (LAD) with 80% stenosis extending to the left main (LM) with mid-LAD myocardial bridging. IVUS (Figure 3) revealed the tightest lesion at proximal LAD (80% plaque burden) with a minimum lumen area (MLA) of 3.69 mm² and eccentric calcification (90–270°) with a calcium nodule. Ostial LAD and distal LM had 70% stenosis, with eccentric plaque. Lesion length was 43 mm, with vessel sizes of 3.5 mm (distal LAD) and 5.0 mm (LM).
Interventional Management
Procedural Step
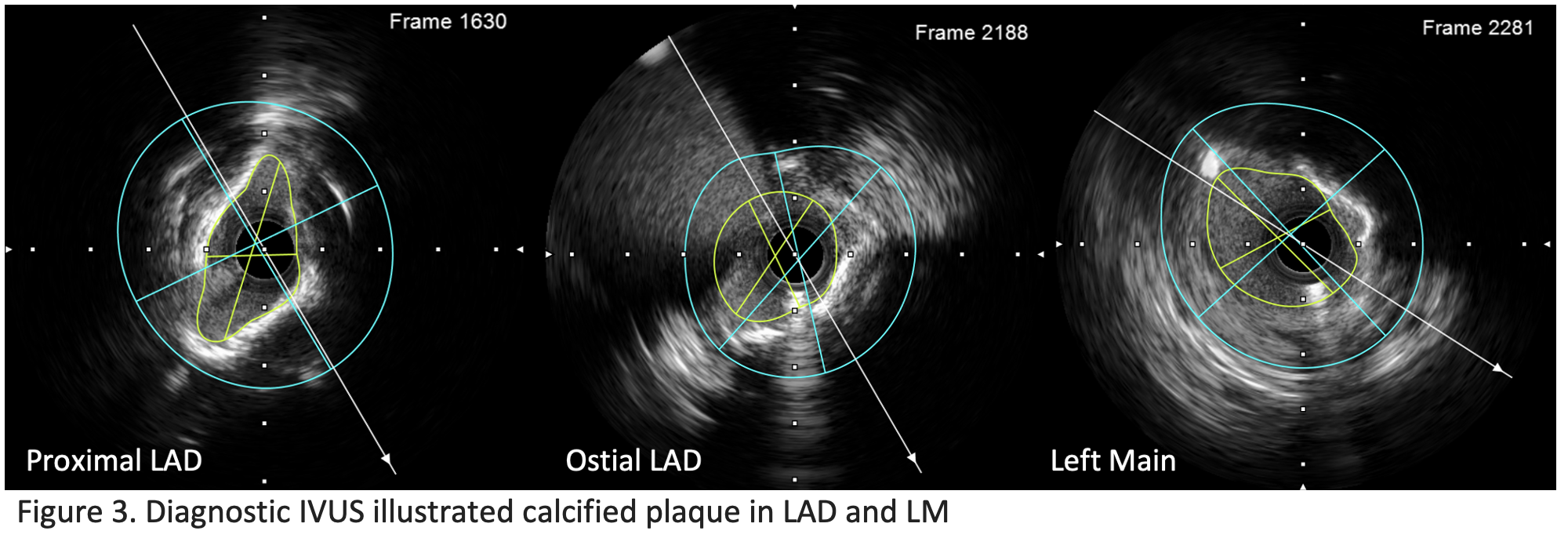
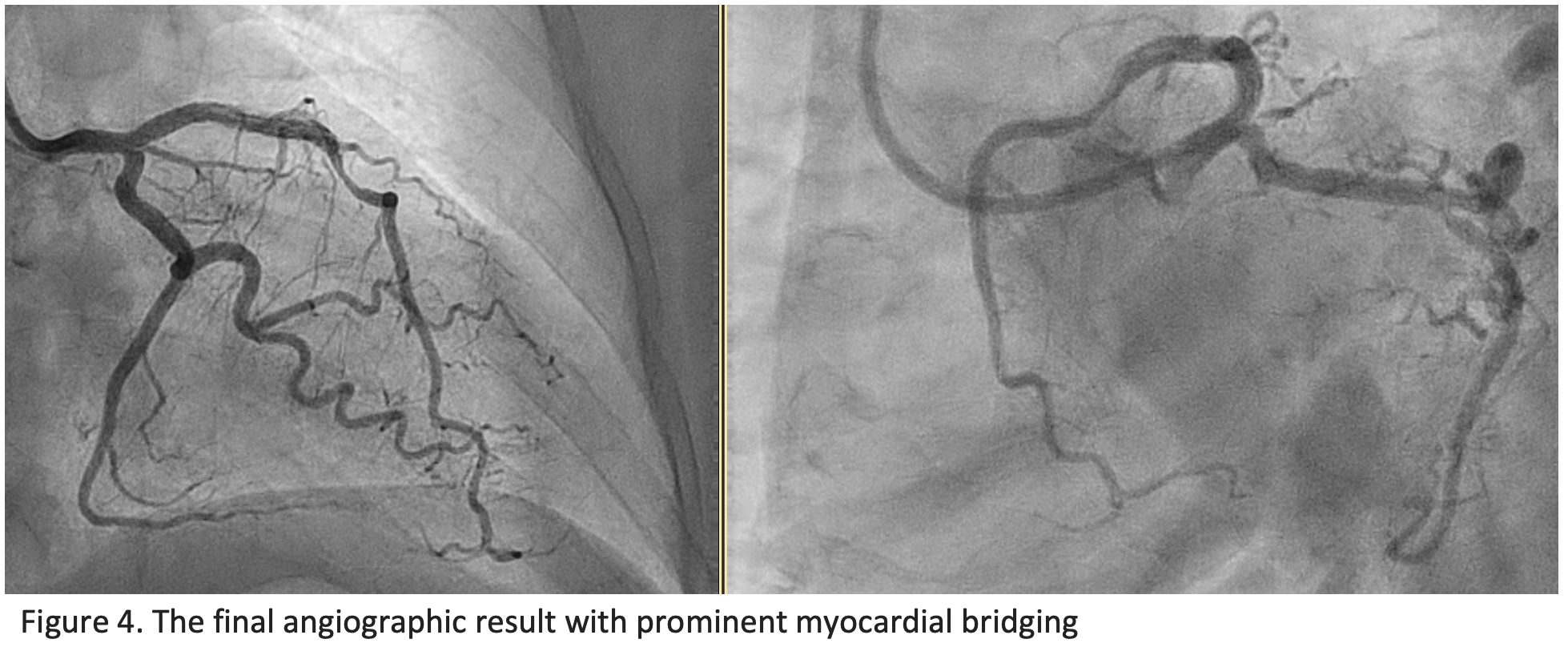
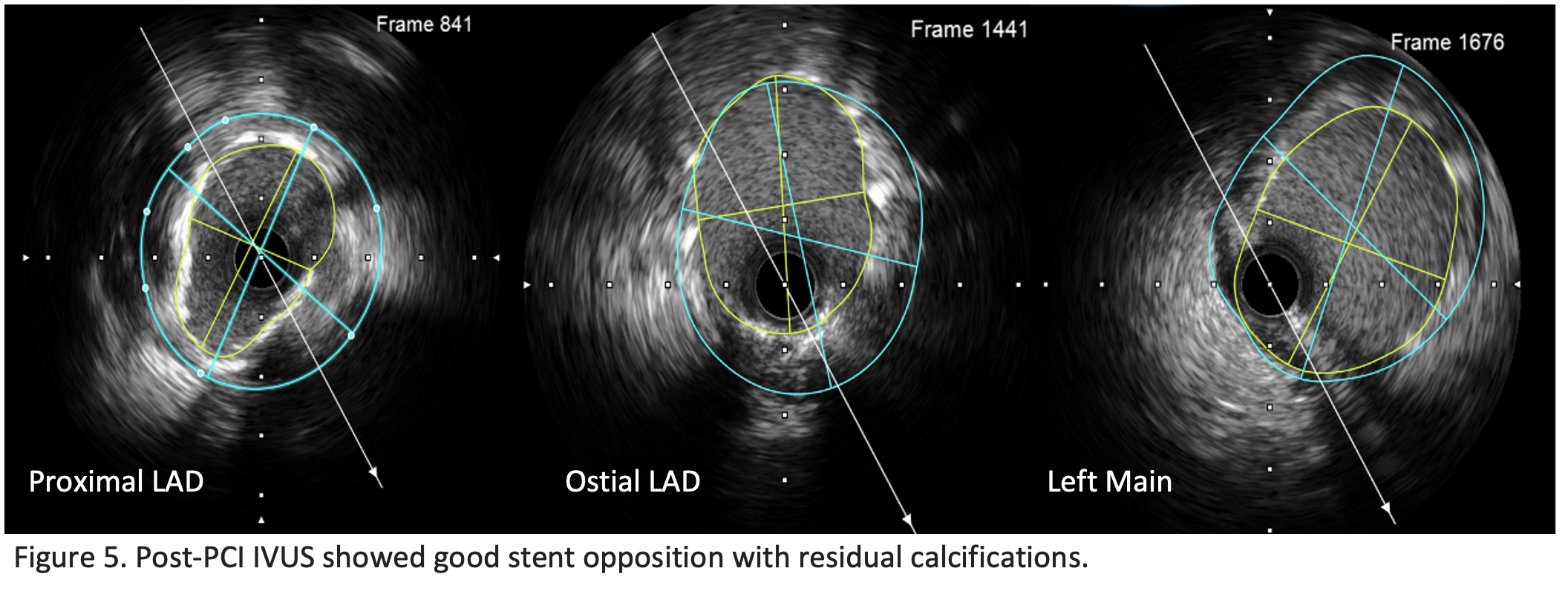
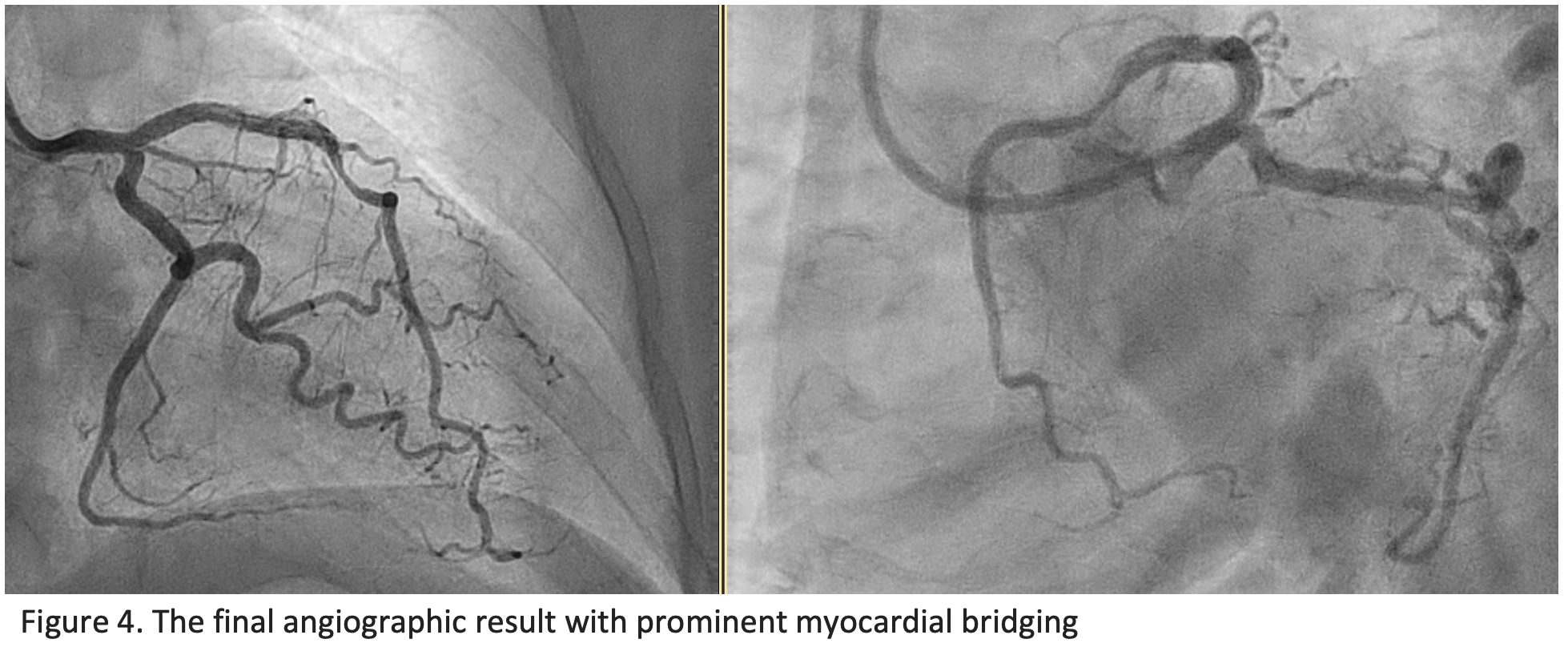
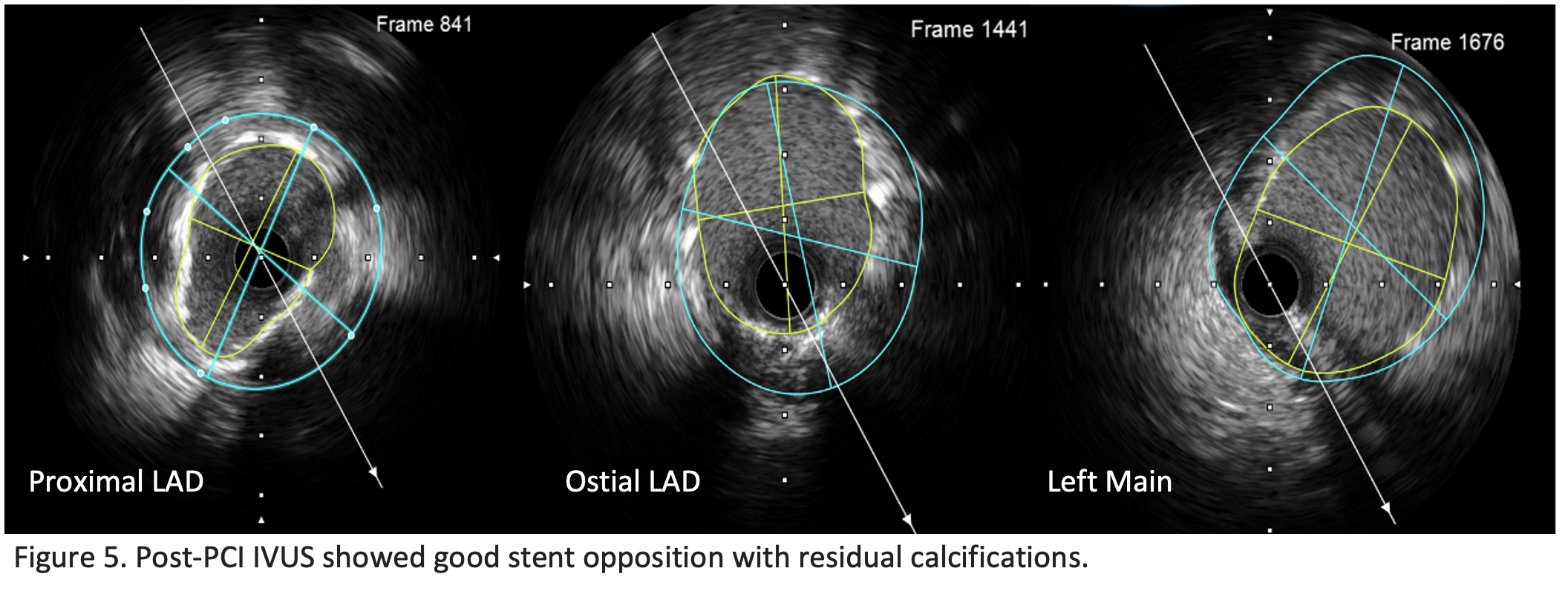
Proceeding with PCI necessitated conversion to femoral access due to severe radial vasopasm. XB 3.0 guiding catheter was used, and LAD and left circumflex (LCx) were wired with Asahi Sion. Serial pre-dilatation over proximal LAD to LM was performed using NC balloon (NC Trek Neo 3.0 x 15 mm) and scoring balloon (Aperta NSE 3.0 x 13 mm), achieving satisfactory calcium crack on IVUS. Drug-eluting stent (DES) Biofreedom Ultra 3.5 x 36 mm was delivered to proximal LAD and further post-dilated with NC Raiden 3.5 x 15 mm. Another overlapping stent Biofreedom Ultra 4.0 x 19 mm was placed in proximal LAD to LM. Proximal optimization technique (POT) utilized the POT-Side-POT method in which LM POT was performed first using NC Raiden 4.5 x 10 mm, followed by dilatation of ostial LCx through stent strut with Rise NC 3.5 x 15 mm, and lastly followed by LM POT again with NC Raiden 4.5 x 10 mm. The distal segment of LAD stent was further optimized using Aperta NSE 3.5 X 13 mm. The final angiographic result was good, however with prominent myocardial bridging seen (Figure 4). Post-PCI IVUS (Figure 5) revealed good stent opposition with residual under-expansion of distal stent segment due to calcification. Minimum stent area (MSA) over proximal LAD, ostial LAD, and LM were 7.57 mm2, 9.45 mm2, and 12.86 mm2, respectively. There was no stent edge dissection.
Case Summary
This case demonstrates the challenge of managing calcified left main and proximal LAD lesions, highlighting the critical role of intravascular imaging for lesion assessment and procedural optimization. The imaging-guided stent placement ensured good outcomes despite residual calcification. Landmark trials like EXCEL, NOBLE, and ISAR-CALC emphasize the importance of tailored PCI strategies in left main disease and calcified lesion preparation, underscoring this case’s relevance in improving patient care in complex scenarios.


