Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-067
Going for the Crack
By Thurston Erng, Anish Hirachan
Presenter
THURSTON ERNG
Authors
Thurston Erng1, Anish Hirachan1
Affiliation
Hospital Serdang, Malaysia1,
View Study Report
TCTAP C-067
Coronary - Complex PCI - Calcified Lesion
Going for the Crack
Thurston Erng1, Anish Hirachan1
Hospital Serdang, Malaysia1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 71-year-old male with previousPCI LAD had NSTE-ACS. He had haematochezia and underwent polypectomy which wascomplicated with post-procedural bleeding. Despite transfusion, he developed chestpains with Troponin rise and ECG changes.


Relevant Test Results Prior to Catheterization
Relevant Catheterization Findings
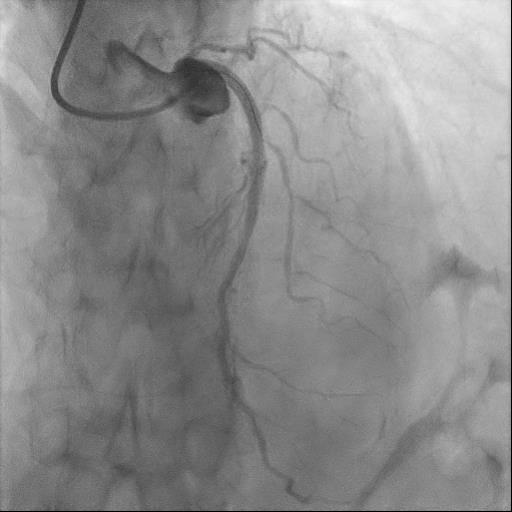
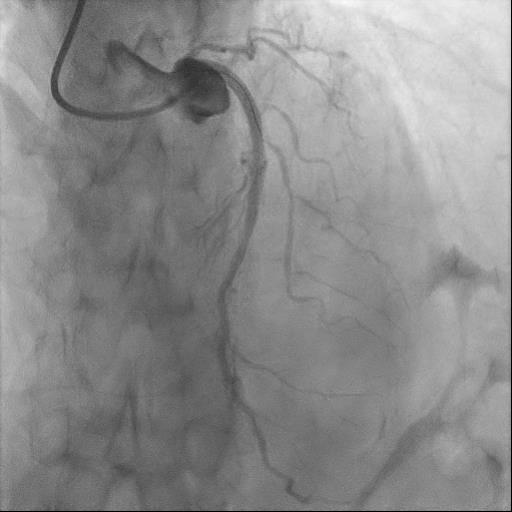
Coronary angiogram showed double-vessel disease. LM was short with ostial LAD calcific nodule and severely calcified proximal LAD and mid-LAD ISR. LCX was non-dominant but with severe disease and distal OM CTO. RCA was unobstructed.
Interventional Management
Procedural Step
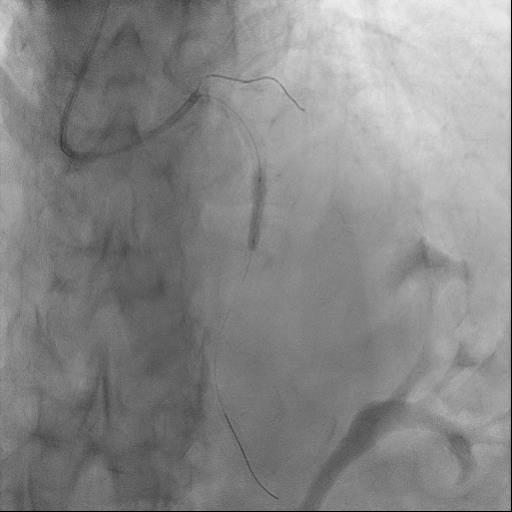
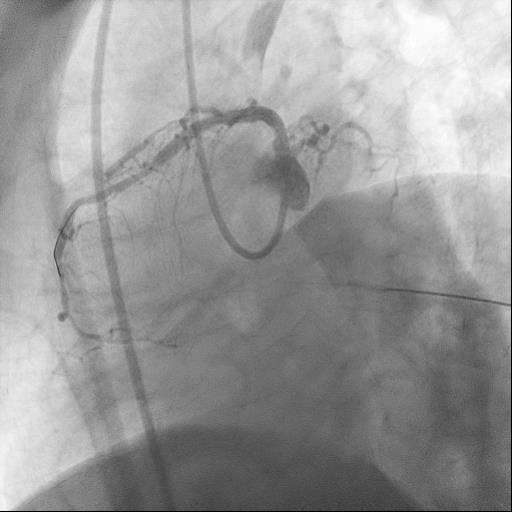
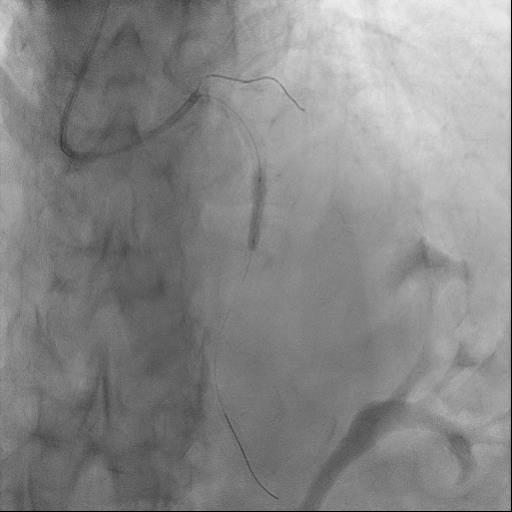
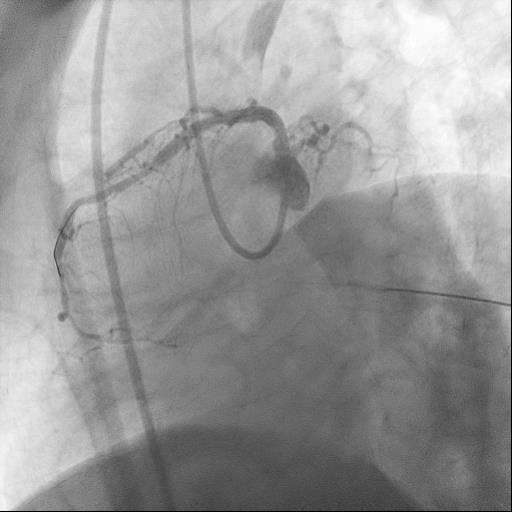
We proceeded with PCI of LM-LADvia 6Fr right ulnar approach. Engagement with EBU 3.0 was challenging. Gentlepredilation with SC 2.0 x 15 mm balloon was performed. However, IVUS cathetercould not pass through. We then decided for rotational atherectomy with 1.5burr from ostial LAD to mid-LAD followed by predilation with NC 2.5 x 15 mm to 18atm. IVUS showed severe calcified nodule at ostial LAD and severe calcified ISRat proximal and distal ends of previous mid-LAD stent. As there were calcificareas which had not cracked, we opted for rotational atherectomy with 1.75burr, again from ostial LAD to mid LAD. Repeat IVUS showed improved luminalgain with minimal cracks in areas of concern. Further predilation with cuttingballoon 3.0 x 15 mm followed by NC 3.5 x 15 mm (up to 18 atm) were performed.Despite these, incomplete balloon expansion at both proximal and distal oldstents persisted. We then proceeded with Shockwave Intravascular Lithotripsy(IVL) using a 3.5 mm balloon [Figure 2]. LM-LAD were then stented with overlappingDES 3.5 x 38 mm and DES 4.0 x 24 mm. Postdilation was performed with NC 3.5 and4.0 to high pressures.
Case Summary
This case demonstrates a highlychallenging calcified case with multiple clinical and procedural complexities:(a) High bleeding risk (b) calcified ISR requiring rota-in-stent (c) ostial LADcalcific nodule with short LM (d) unyielding concentric calcium at ISR site (e)need for combined modalities of rotablation and lithotripsy for calciummodification.


