Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-117
A Case of Complex PCI and Cardiogenic Shock: A Shifting Risk-Benefit Ratio
By Joseph O'Brien, Gavin Manmathan, Derek Chew, James Sapontis
Presenter
Joseph O'Brien
Authors
Joseph O'Brien1, Gavin Manmathan1, Derek Chew1, James Sapontis1
Affiliation
Victorian Heart Hospital, Australia1,
View Study Report
TCTAP C-117
Coronary - Complex PCI - Left Main
A Case of Complex PCI and Cardiogenic Shock: A Shifting Risk-Benefit Ratio
Joseph O'Brien1, Gavin Manmathan1, Derek Chew1, James Sapontis1
Victorian Heart Hospital, Australia1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
An 80-year-old man was referred for inpatient percutaneous intervention (PCI) to calcified left main (LMCA) and left anterior descending (LAD) arteries with known triple vessel disease that had been declined surgical revascularization since 2012. However, with five subsequent NSTEMI presentations and consistent effort angina, he was accepted for high-risk PCI. He examined frail. Despite presenting with pulmonary edema, he had been diuresed to euvolemia with normal heart rate and blood pressure.
Relevant Test Results Prior to Catheterization
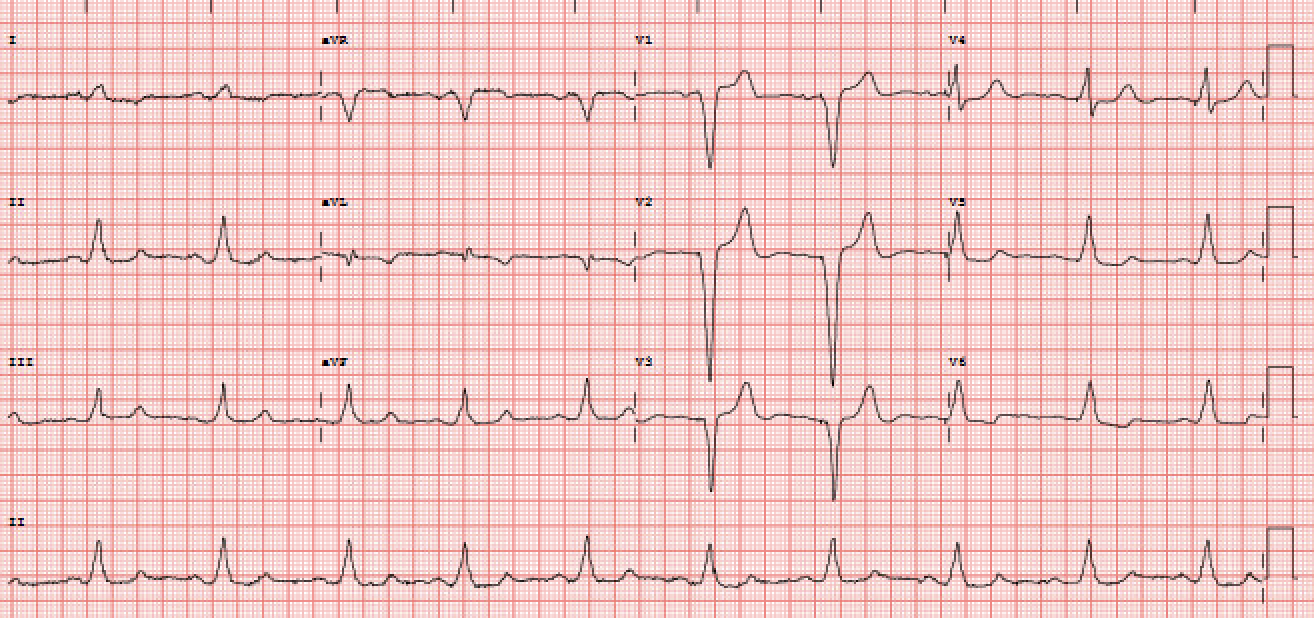
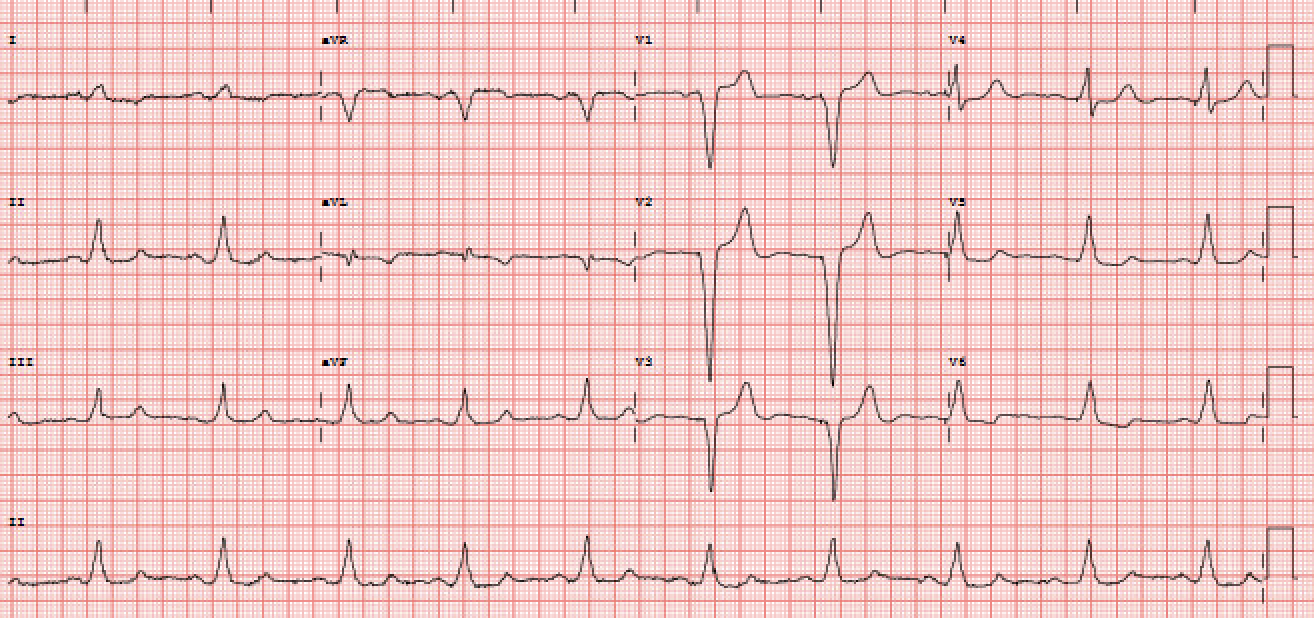
His high-sensitivity troponin peaked at 3644 ng/dL in the context of a creatinine of 1.3 mg/dL, hemoglobin of 10.7 g/dL, and GFR of 54 mL/min/1.73m2. Transthoracic echocardiography showed moderately reduced left ventricular ejection fraction (35-40%), mild pulmonary hypertension (pulmonary artery systolic pressure of 44 mmHg), and moderate aortic and mitral regurgitation. Angiography from two years prior showed heavily calcified triple vessel disease with LMCA involvement. His EKG was paced.
Relevant Catheterization Findings
The LMCA contained heavily calcified, severe, distal stenosis across the ostium of the left circumflex artery (LCx). The LAD was heavily calcified throughout its course with severe, mid-to-apical stenosis. The LCx and RCA both contained severe ostial stenoses. The left ventricular end-diastolic pressure at the commencement of the case was severely elevated at 24 mmHg. In conclusion, there was mild progression of his severe, triple vessel disease seen two months prior.
Interventional Management
Procedural Step
From right femoral access, an intravascular ultrasound (IVUS) run was performed showing critical, distal LMCA disease extending throughout the proximal-to-mid LAD, which was heavily calcified in a concentric fashion. Rotational atherectomy was performed with sequentially-sized burrs. Firstly, a 1.75 mm burr was used in the LMCA into the ostial LAD. Secondly, a 1.25 mm burr was run through the mid LAD. A 2.5 mm x 20 mm drug-eluting stent (DES) was then deployed in the mid-LAD and post-dilated with a 2.75 mm non-compliant (NC) balloon. Intravascular lithotripsy (IVL) was performed from mid LAD to mid LMCA using a 3.0 mm balloon. Overlapping 3.5 mm x 32 mm and 4.0 mm x 16 mm DES were deployed from the mid LAD back to mid LMCA. A final IVUS run demonstrated good stent symmetry and apposition. Post-dilatation was performed in a tapering fashion in the mid LAD with a 2.75 mm NC balloon and the mid LMCA with a 4.5 mm NC balloon. Final angiography demonstrated a good result with TIMI 3 flow to the distal vessel and no dissection, residual stenosis in the stented segments, nor thrombosis.
At the end of the case, the patient went into shock and had a pulseless electrical activity arrest. His pacemaker failed to capture, and in accordance with his wishes no CPR was performed and the patient died.
At the end of the case, the patient went into shock and had a pulseless electrical activity arrest. His pacemaker failed to capture, and in accordance with his wishes no CPR was performed and the patient died.
Case Summary
Our case offers a clinical dilemma. A man is experiencing daily pain on 4 classes of anti-anginal therapy so debilitating he was chair-bound. He had been discussed over twelve years and was designated medical management due to the high-risk nature of his lesions. After repeat presentations, the man was offered high-risk PCI to calcified lesions in his LMCA and LAD. With the assistance assistance of two rotational atherectomy burrs, intravascular ultrasound, and intravascular lithotripsy, three overlapping drug-eluting stents were placed producing an excellent angiographic and physiological result. Despite this, he died during transfer to his inpatient bed with electromechanical dissociation.

