Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-104
A Clinical Case of Six PCI Procedures for Repeated In-Stent Restenosis in the Left Main Ostium
By Naoki Shibata, Hoshito Karasawa, Yasuhiro Morita, Itsuro Morishima
Presenter
Naoki Shibata
Authors
Naoki Shibata1, Hoshito Karasawa1, Yasuhiro Morita1, Itsuro Morishima1
Affiliation
Ogaki Municipal Hospital, Japan1,
View Study Report
TCTAP C-104
Coronary - Complex PCI - In-Stent Restenosis
A Clinical Case of Six PCI Procedures for Repeated In-Stent Restenosis in the Left Main Ostium
Naoki Shibata1, Hoshito Karasawa1, Yasuhiro Morita1, Itsuro Morishima1
Ogaki Municipal Hospital, Japan1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
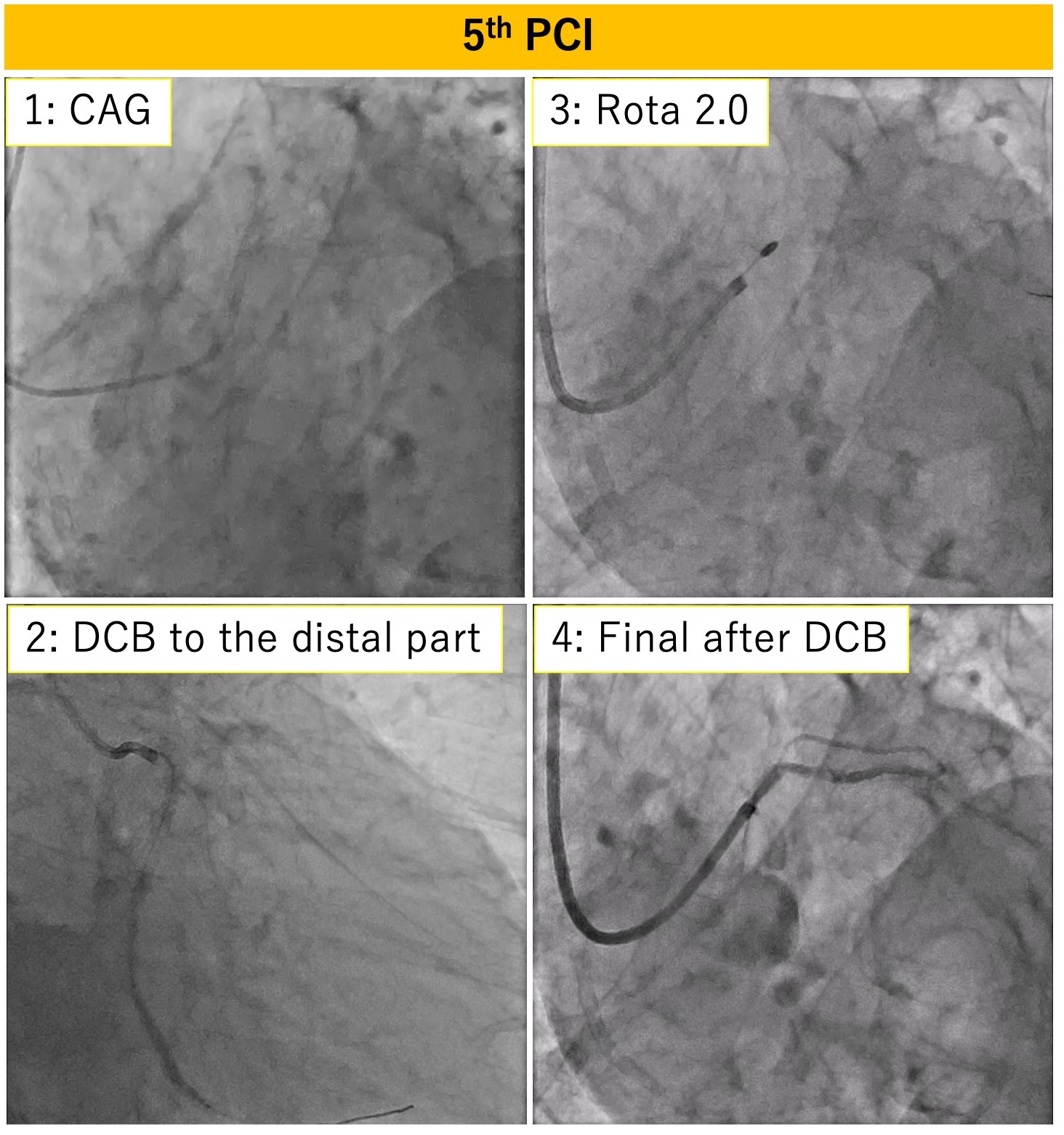
A man in his 70s underwent coronary artery bypass grafting with a left internal thoracic artery graft to the LAD 25 years ago. Five years ago, he received a DES from the LCX to the LMT ostium for angina. He experienced three episodes of ISR treated with POBA and DCB. Recently, effort angina appeared again.
Relevant Test Results Prior to Catheterization
The patient has well-controlled diabetes and no renal dysfunction. However, the LVEF has decreased to 30%, and stress scintigraphy revealed ischemia in the lateral wall.
Relevant Catheterization Findings
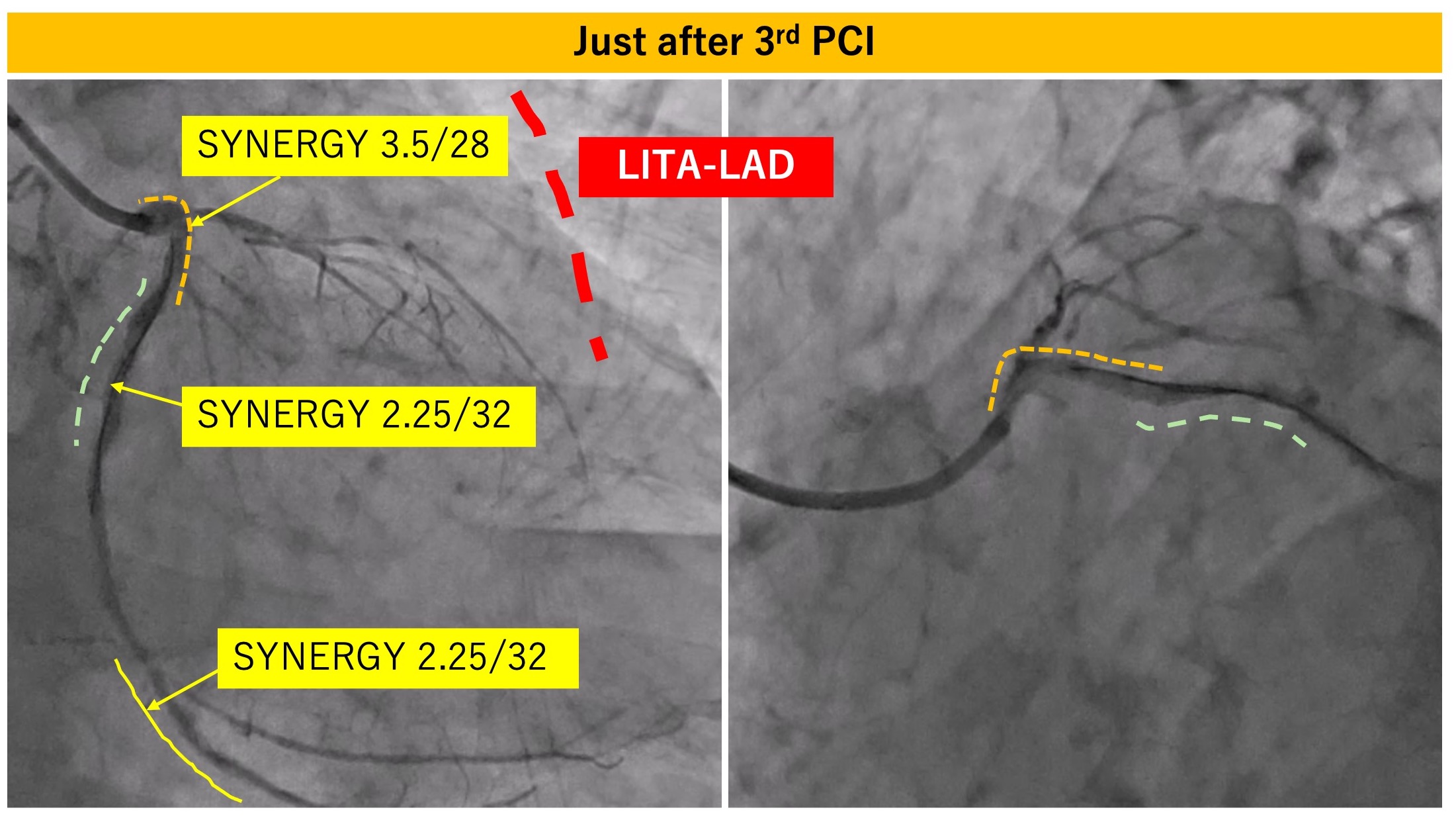
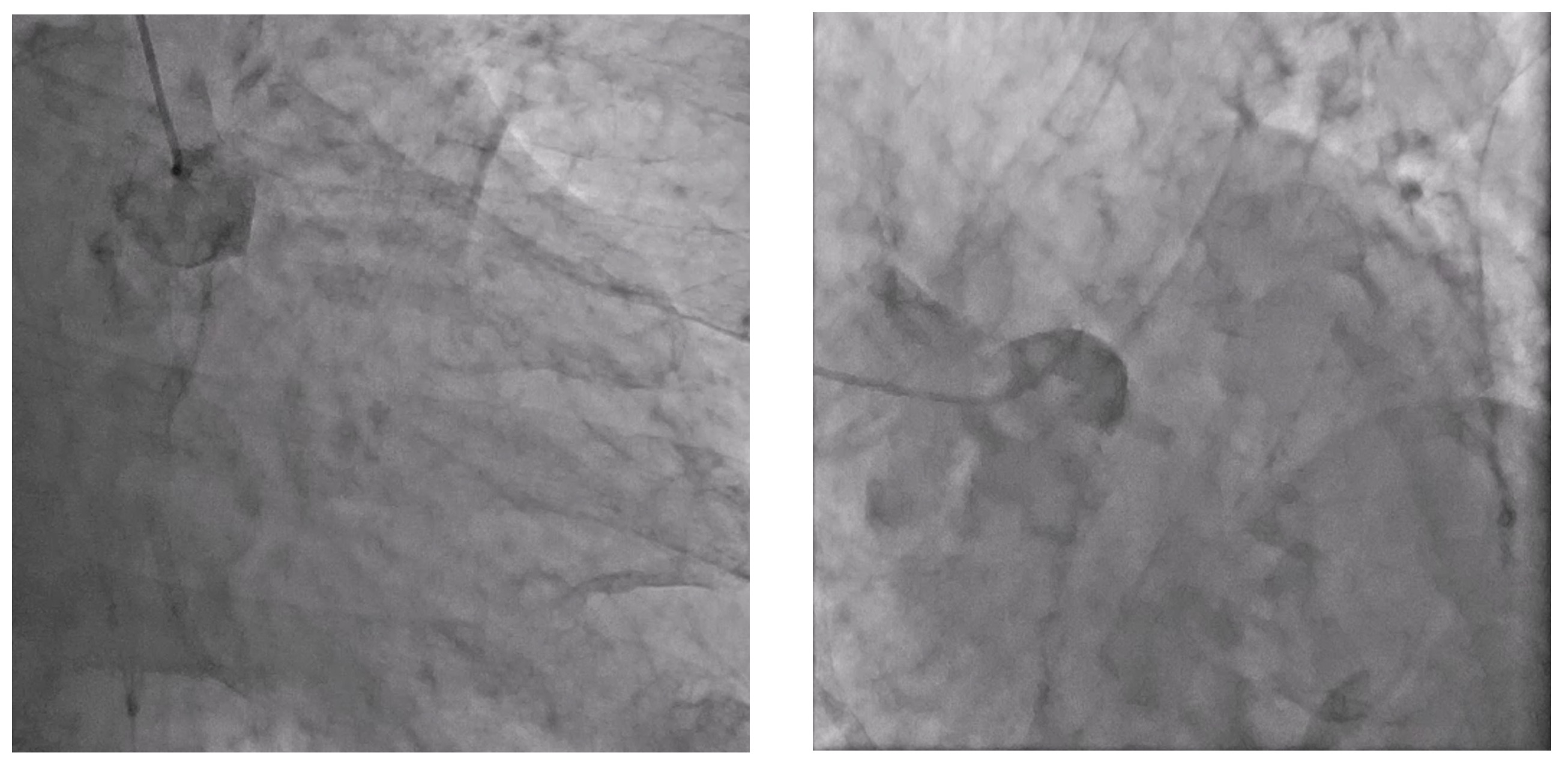
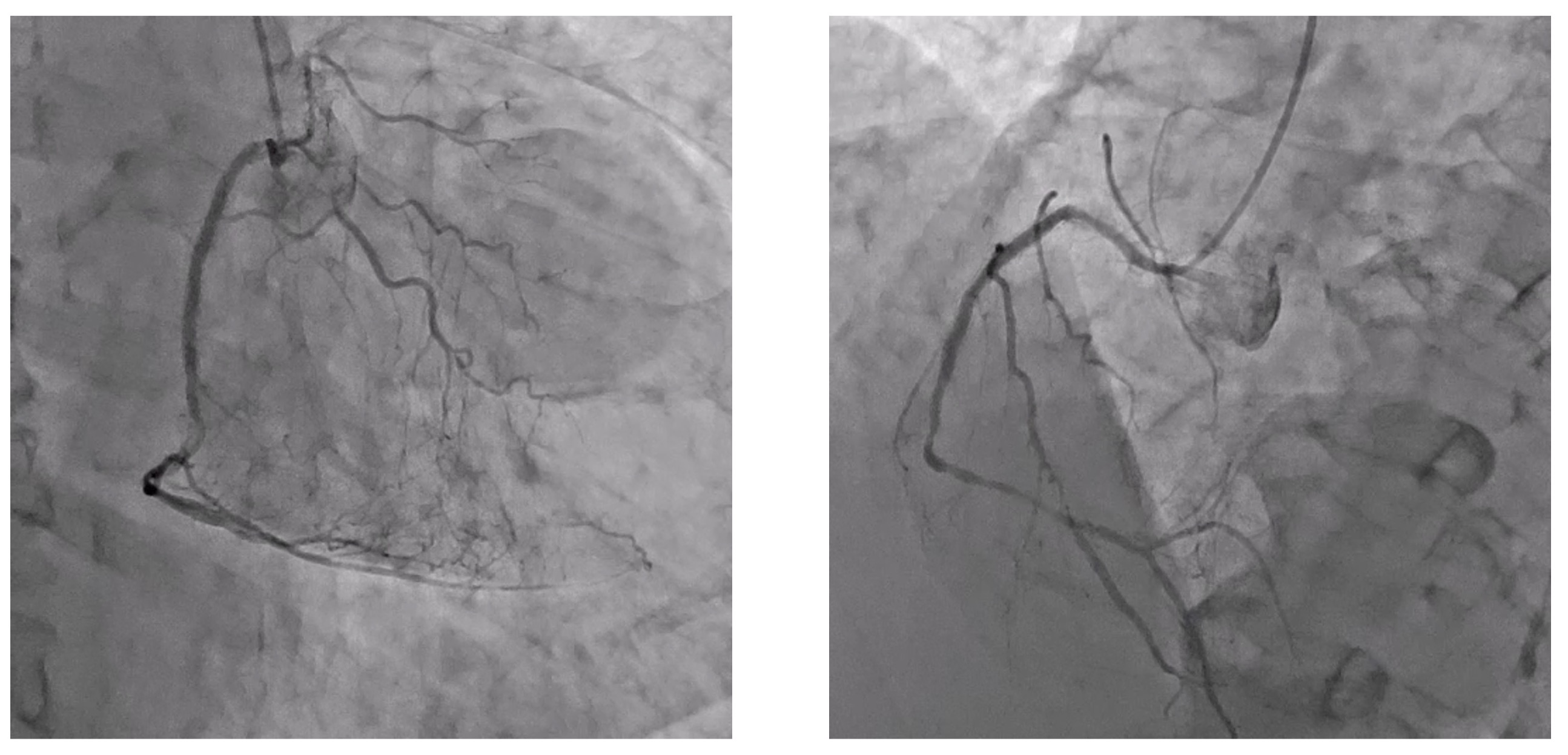
The right coronary artery shows no significant stenosis, and the LITA-LAD graft remains patent. However, the LMT is occluded from its ostium.
Interventional Management
Procedural Step
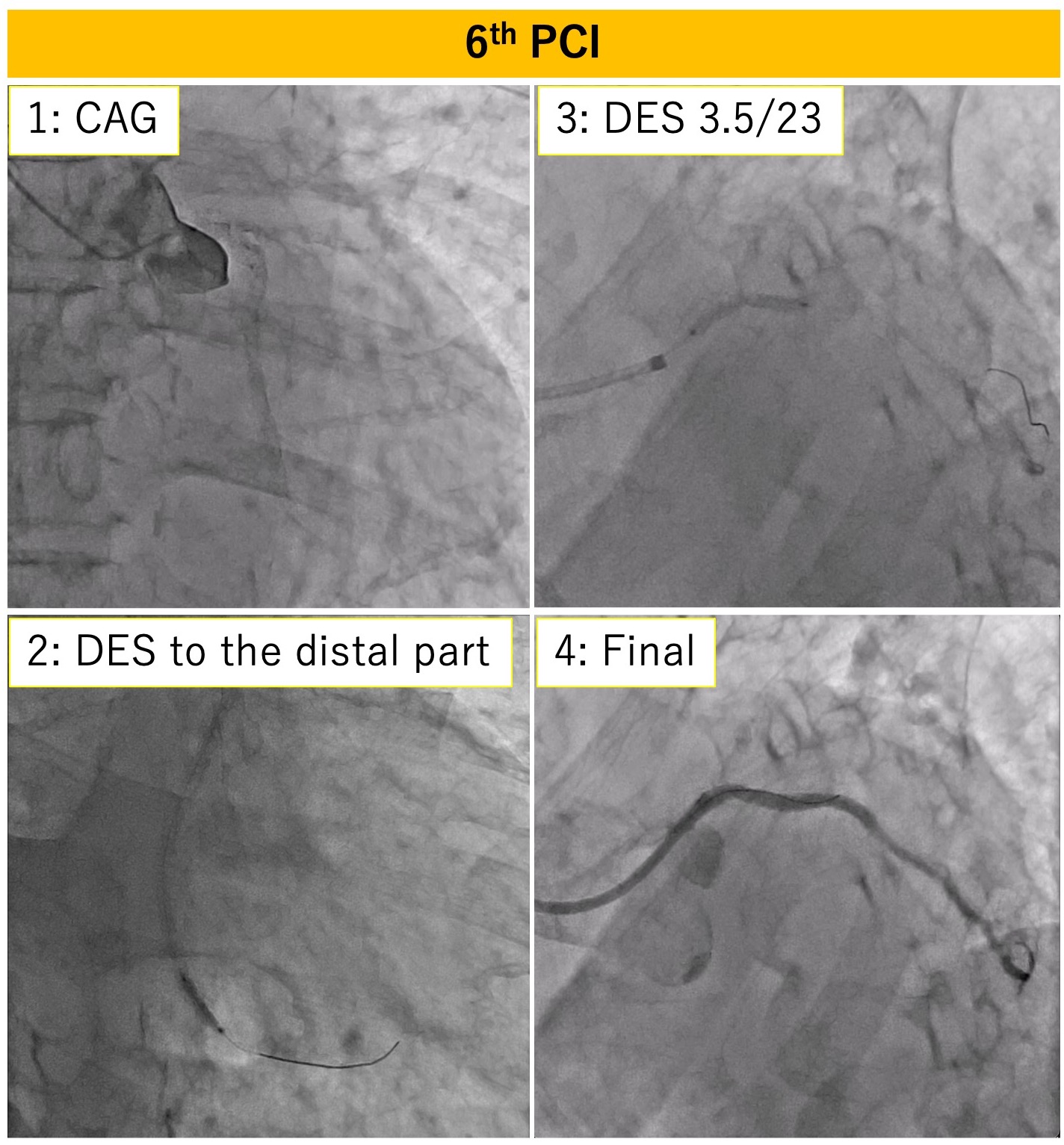
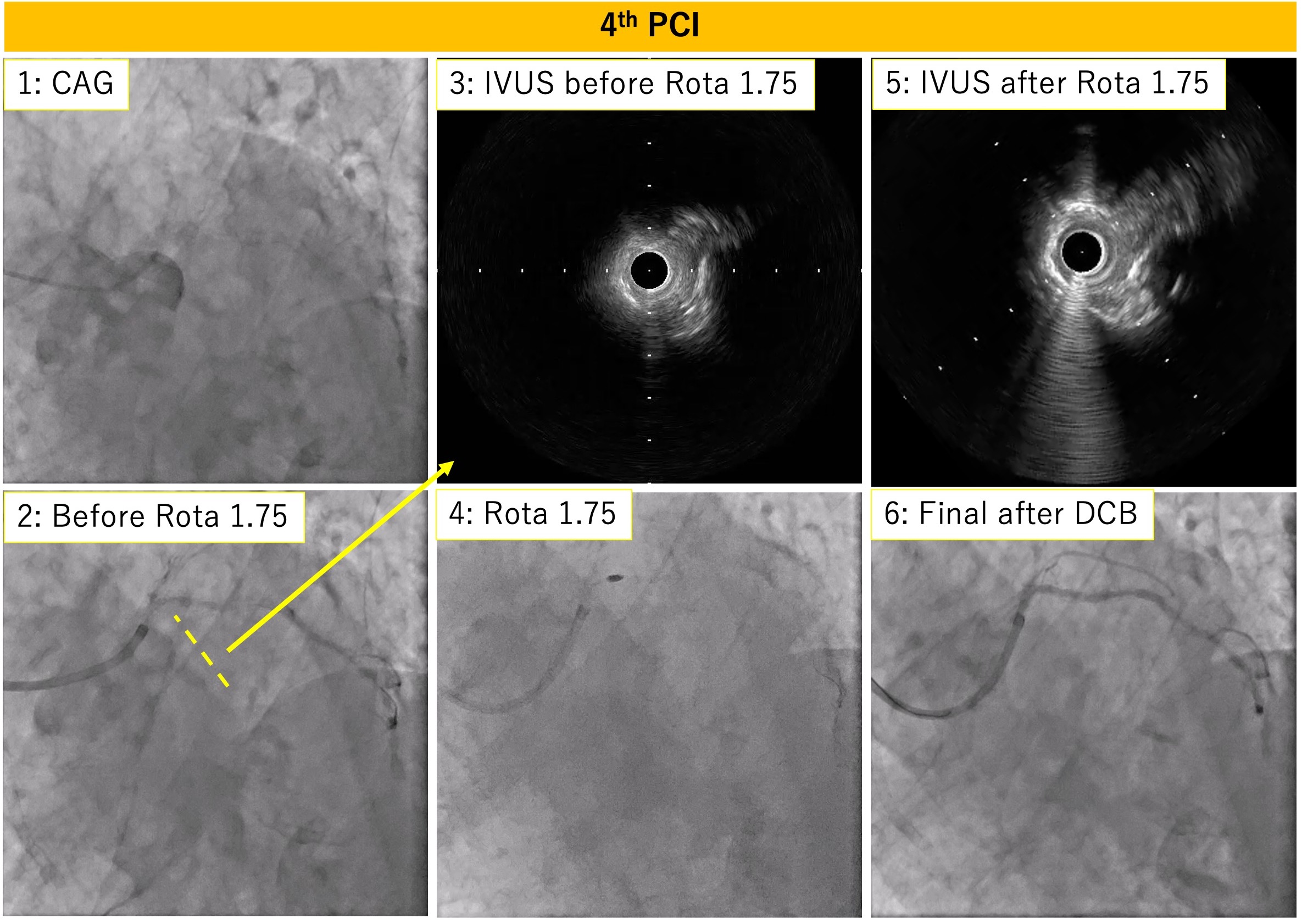
During the fourth intervention, total in-stent occlusion was identified at the LMT ostium. Using a Gaia Next 2 wire, the lesion was crossed successfully. While a semicompliant balloon could pass, a cutting balloon could not, and IVUS revealed stent under-expansion as the cause. Rotational atherectomy with a 1.75 mm burr was performed, followed by POBA with a 3 mm compliant balloon, and the procedure was finalized with drug-coated balloon DCB therapy.
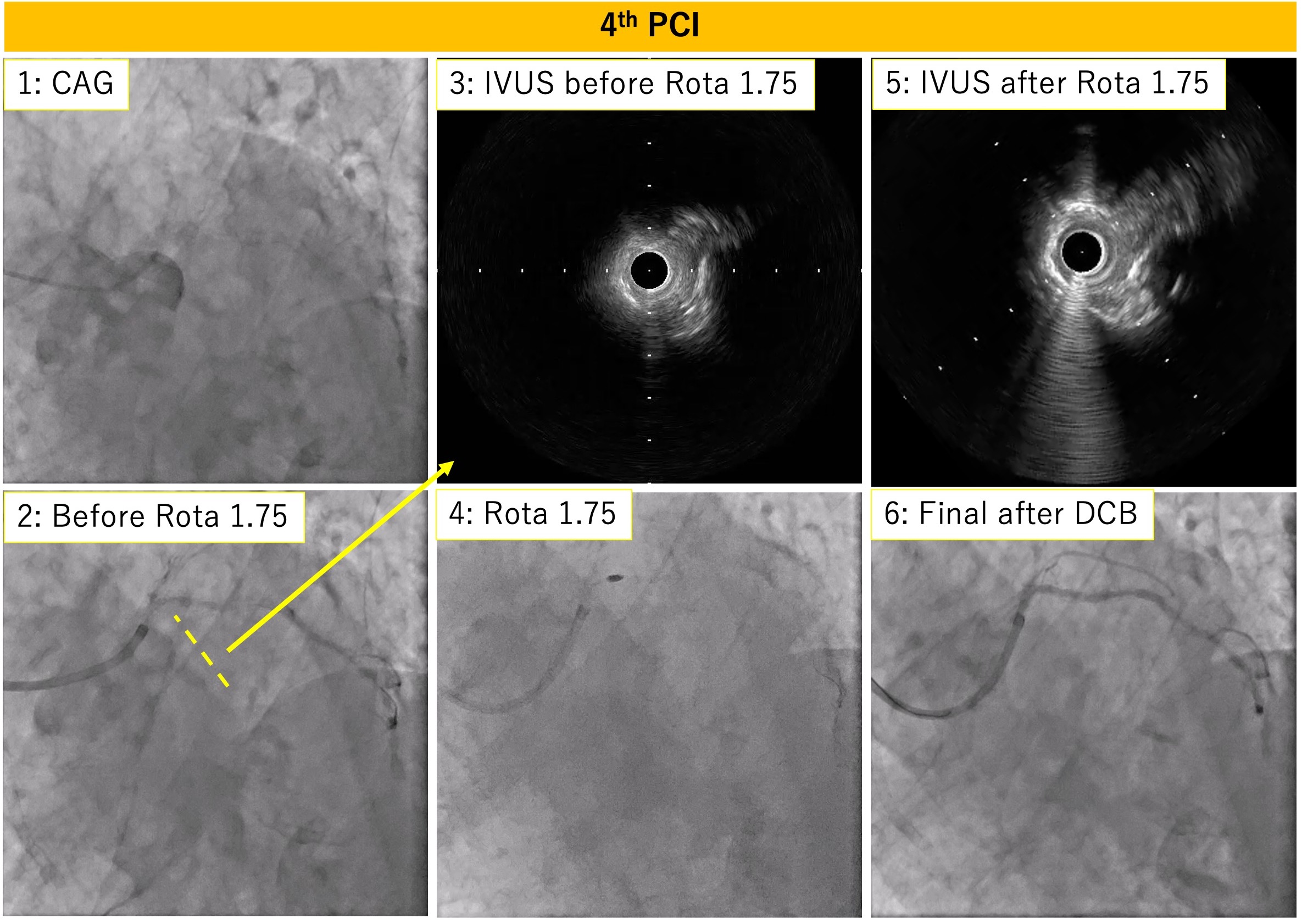
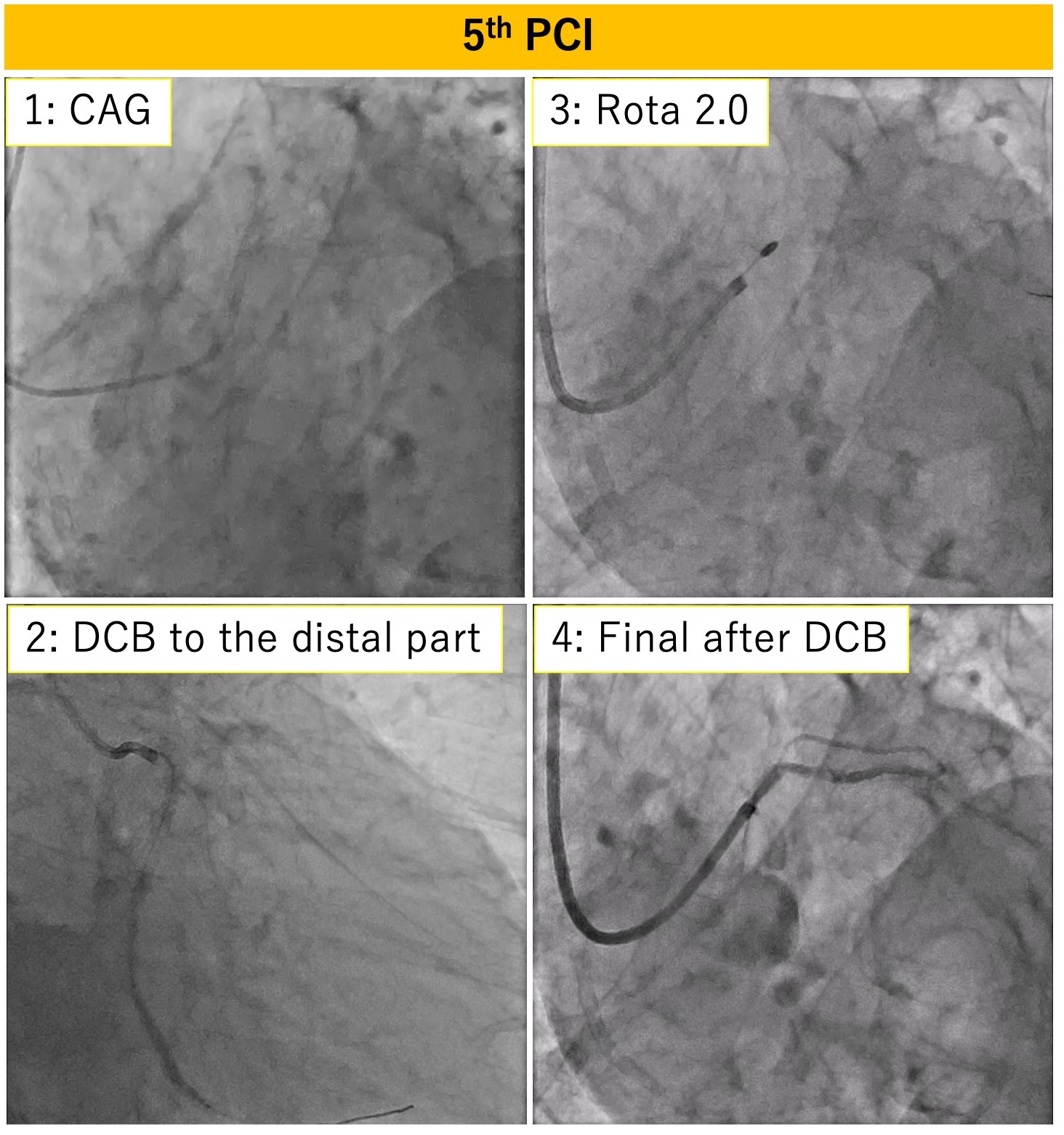
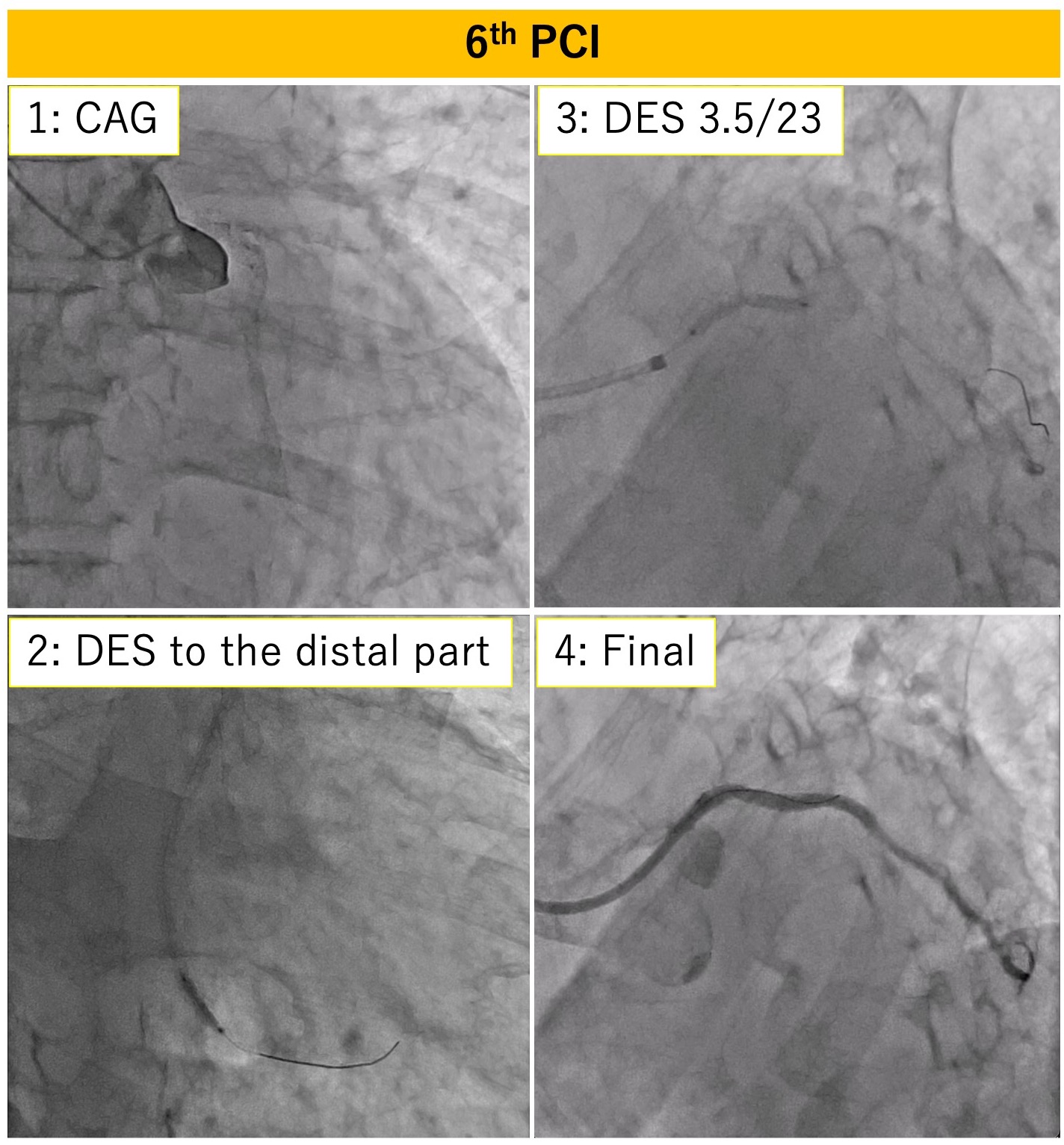
Case Summary
This case highlights the challenges of treating repeated in-stent occlusion in the LMT ostium, which required careful selection of guiding catheters, appropriate rotational atherectomy burr sizes, and effective management of slow flow phenomena. We report this case to share our experience in managing this complex condition and overcoming its associated procedural difficulties.


