Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-187
When Seeing Is Not Believing
By An Shing Ang, Kwok Kong Loh
Presenter
An Shing Ang
Authors
An Shing Ang1, Kwok Kong Loh2
Affiliation
Woodlands Health, Singapore1, Tan Tock Seng Hospital, Singapore2,
View Study Report
TCTAP C-187
Coronary - Imaging & Physiology - FFR
When Seeing Is Not Believing
An Shing Ang1, Kwok Kong Loh2
Woodlands Health, Singapore1, Tan Tock Seng Hospital, Singapore2,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
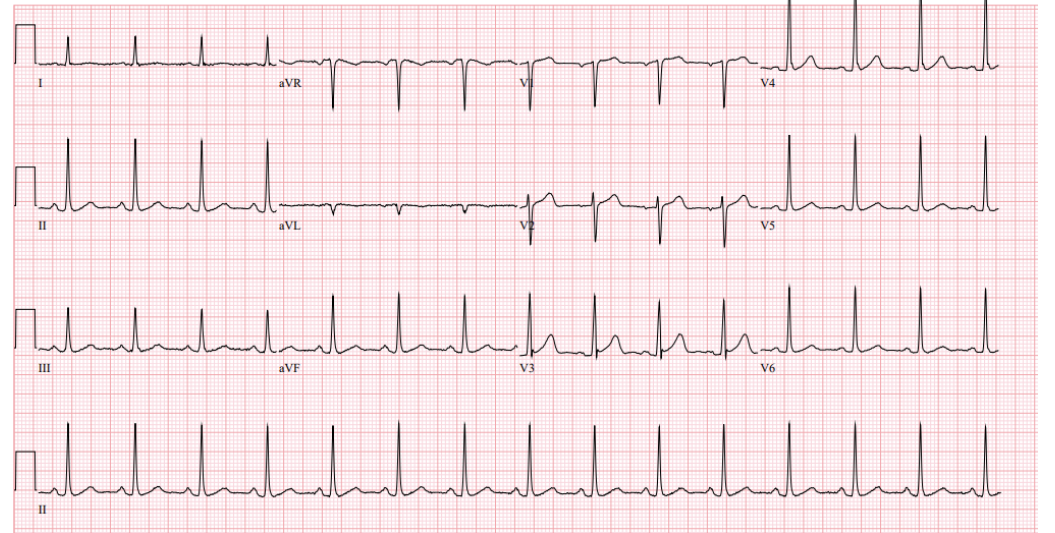
My patient is a 60 year old gentleman with cardiovascular risk factors of hypertension and hyperlipidemia.He was admitted for exertional angina, with central chest discomfort radiating to the jaw, associated with diaphoresis for the last 2 weeks. Physical examination was largely unremarkable with no audible murmurs on ascultation. An electrocardiogram revealed normal sinus rhythm with no ischemic changes.
Relevant Test Results Prior to Catheterization
The patient's baseline full blood counts and renal function tests were within normal limits.
His high-sensitive Troponin I ranged from 10-14ng/L (Reference <18ng/L).
Chest X-ray did not reveal any significant cardiomegaly or lung pathology.
Relevant Catheterization Findings
His coronary angiogram showed a right dominant circulation.
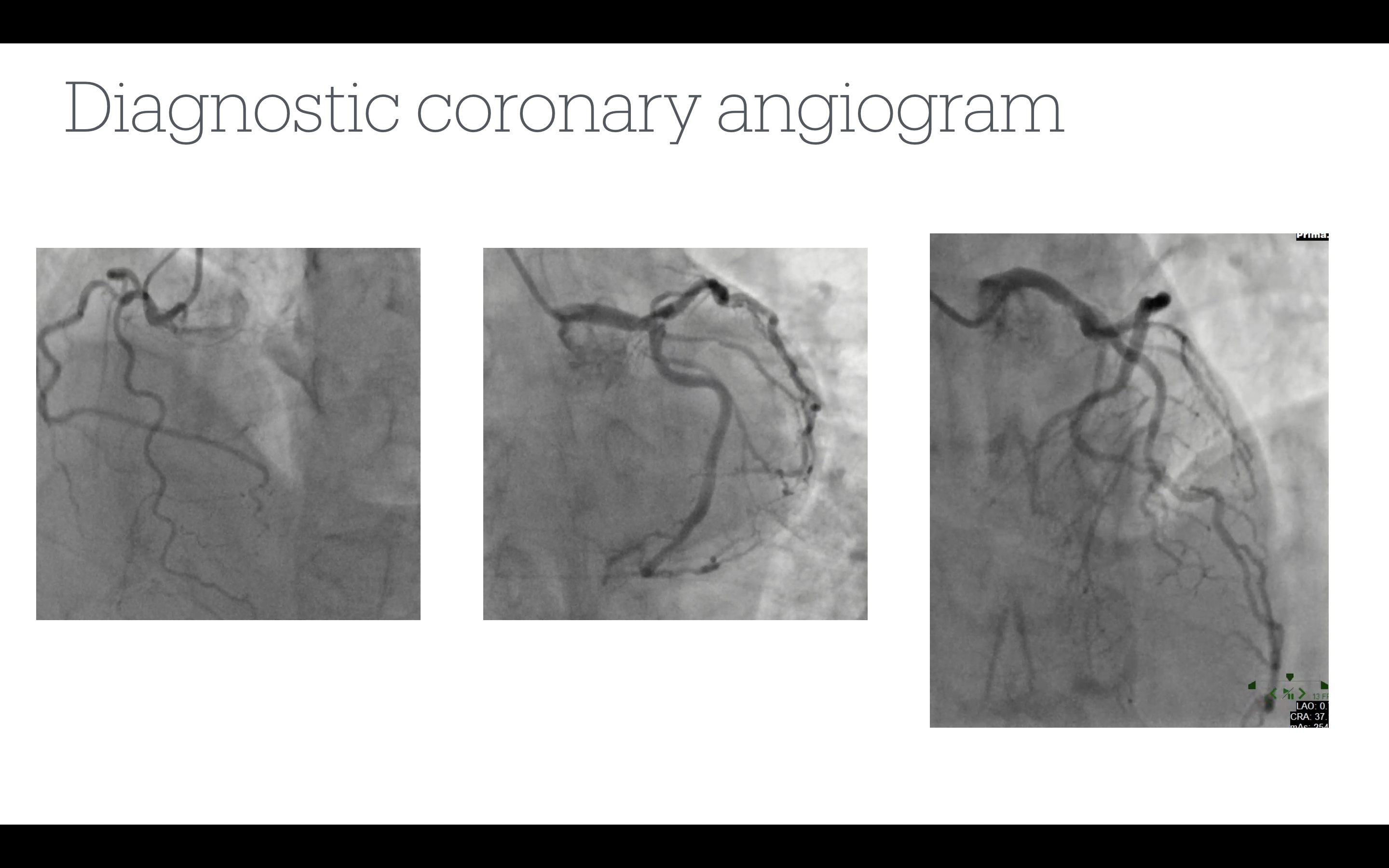
There was an ostial LAD moderate lesion (best seen in the caudal views) and mid-LAD diffuse moderate disease.
The left circumflex artery was a large artery with no apparent flow-limiting stenosis.
The right coronary artery was a medium-sized artery that was tortuous and had no apparent flow-limiting stenosis.
Interventional Management
Procedural Step
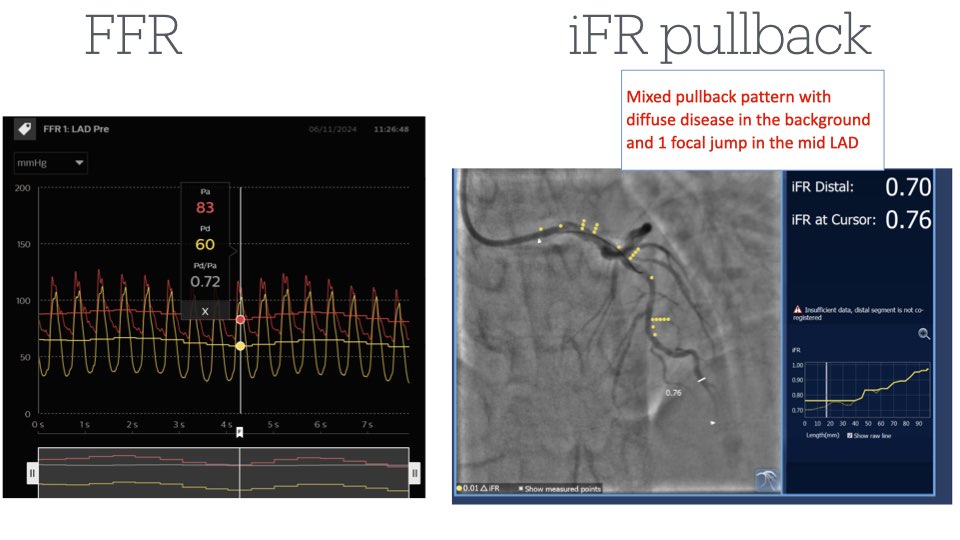
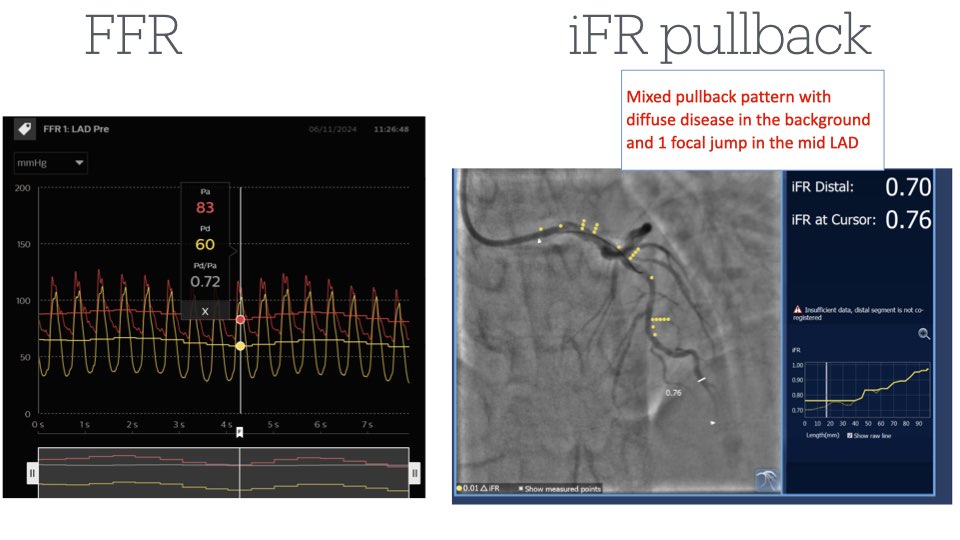
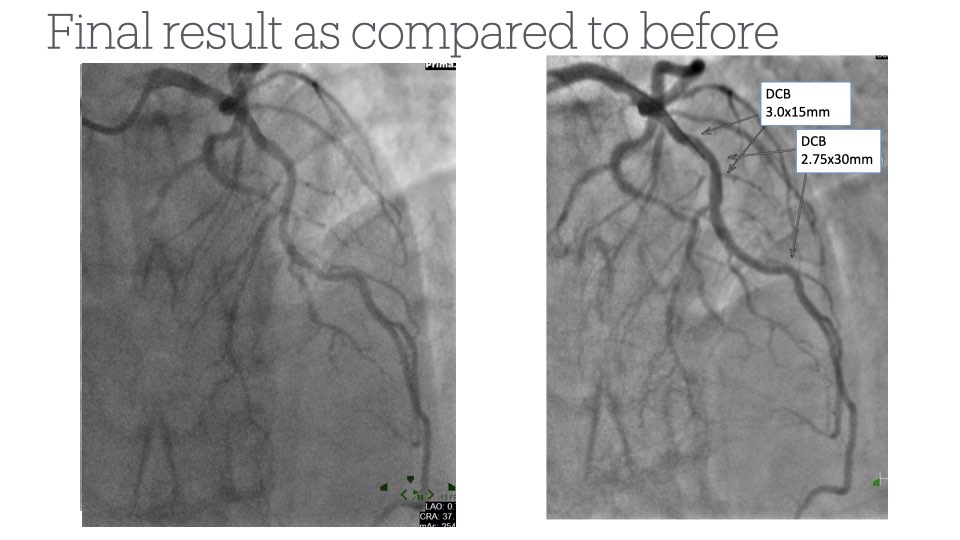
We decided to perform a hemodynamic assessment and IVUS examination of the LAD. The minimal lumen area of the ostial LAD was 7.2mm2. However, unexpectedly, the minimal lumen area of the mid-LAD was only 3.9mm2.The fractional flow reserve (FFR) was 0.72, and the instantaneous wave-free ratio (iFR) was 0.70. We performed an iFR pullback, which showed diffuse disease with two focal jumps in the mid-LAD, corresponding to the tightest mid-LAD lesions. The mid-LAD vessel diameter was approximately 2.5-3.0mm. We subsequently pre-dilated the mid-LAD with a 2.5x15mm scoring balloon with good POBA results. We deployed a 2.75x30mm drug-coated balloon and a 3.0x15mm drug-coated balloon in the mid-LAD.
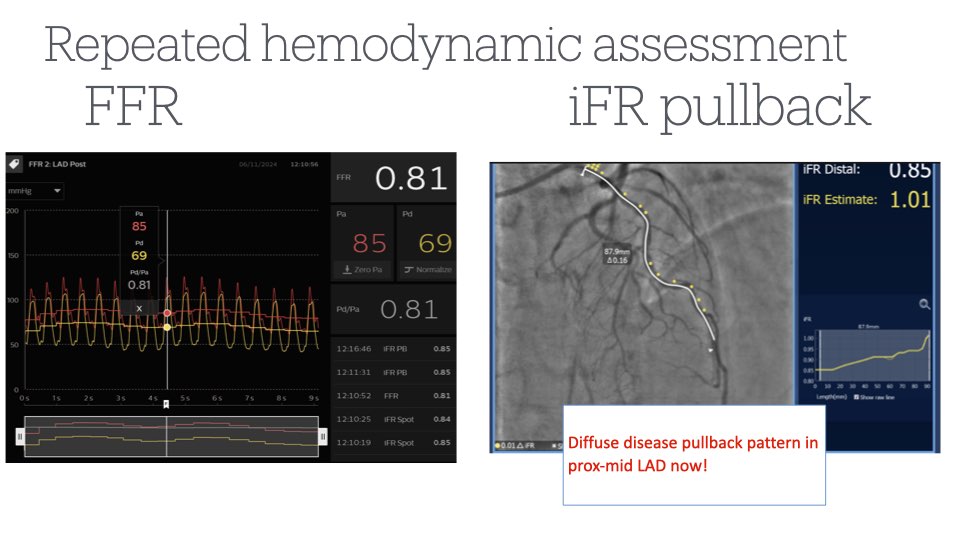
Repeat hemodynamic assessment now showed an improvement of FFR from 0.72 to 0.81 and iFR from 0.70 to 0.85. The iFR pullback now showed diffuse disease with no focalities in the LAD. Repeat IVUS also showed improvement of MLA from 3.9mm2 to 5.2mm2. We decided to accept this result and monitor the patient's symptoms in the outpatient setting.
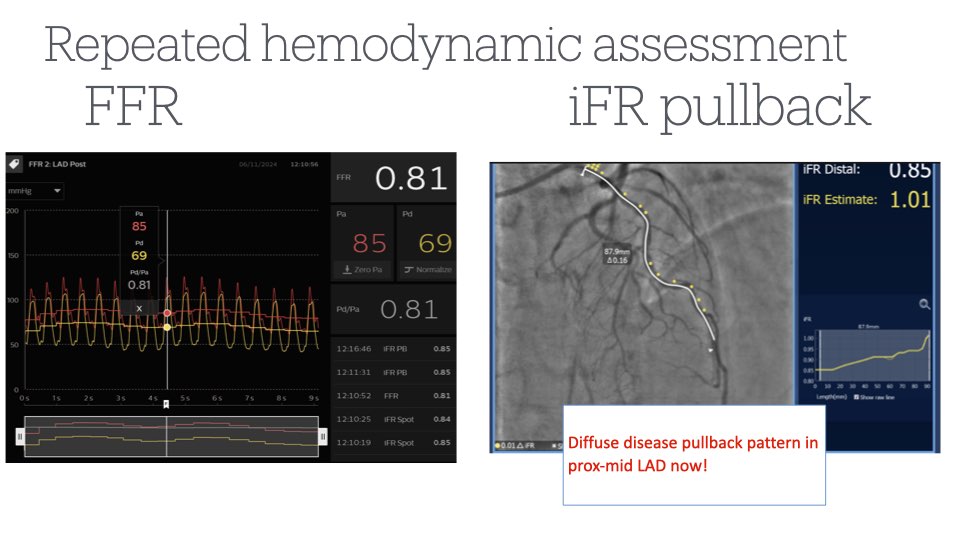
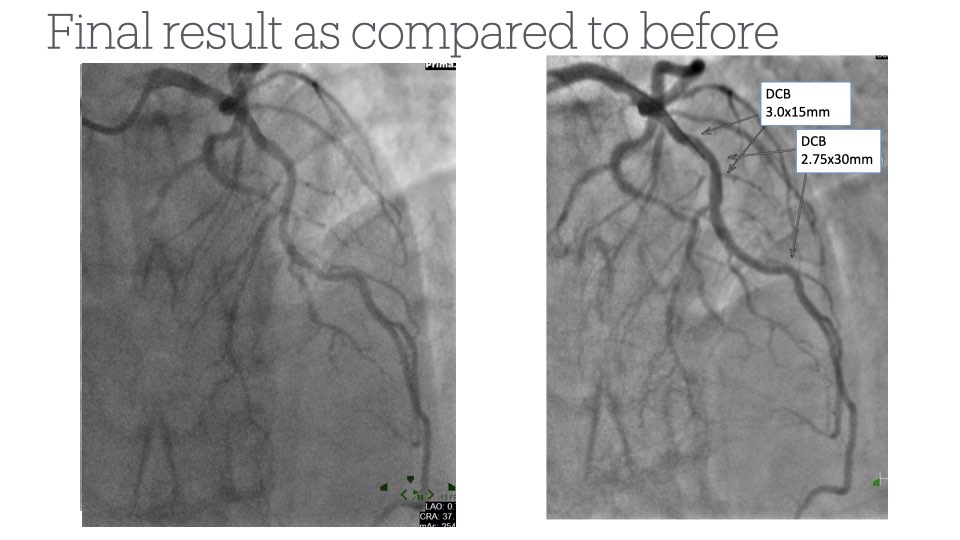
Repeat hemodynamic assessment now showed an improvement of FFR from 0.72 to 0.81 and iFR from 0.70 to 0.85. The iFR pullback now showed diffuse disease with no focalities in the LAD. Repeat IVUS also showed improvement of MLA from 3.9mm2 to 5.2mm2. We decided to accept this result and monitor the patient's symptoms in the outpatient setting.
Case Summary
This case showcases the importance of hemodynamic and IVUS assessments of "moderate"-looking lesions, especially in patients with typical symptoms.
Performing hemodynamic and IVUS assessments elucidated significant LAD disease and allowed us to choose our targets for PCI to achieve the best hemodynamic result for the patient.
While the iFR remained in the significant range (0.85), the FFR improved to more than 0.80. We removed the localities in the patient's LAD disease, which we felt was an acceptable endpoint for PCI. Moreover, performing DCB angioplasty allowed us to avoid putting any metal in the patient's arteries.


