Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-066
A Complex Case with Heavy Calcification: Move the Hard Rock Away
By Chi-Ting Lu, Shih-Hsien Sung
Presenter
Chi-Ting Lu
Authors
Chi-Ting Lu1, Shih-Hsien Sung1
Affiliation
Taipei Veterans General Hospital, Taiwan1,
View Study Report
TCTAP C-066
Coronary - Complex PCI - Calcified Lesion
A Complex Case with Heavy Calcification: Move the Hard Rock Away
Chi-Ting Lu1, Shih-Hsien Sung1
Taipei Veterans General Hospital, Taiwan1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 72-year-old male has a history of type 2 diabetes and hyperlipidemia. In the past six months, he developed intermittent chest tightness and exertional dyspnea, but he ignored it. However, progressive dyspnea and chest tightness occurred, and he came to our emergency department for help. On arrival, his vital signs were as follows: temperature of 36°C, pulse rate of 120 bpm, respiratory rate of 20 /min, blood pressure of 177 /112 mmHg, and oxygen saturation of 96% on room air.


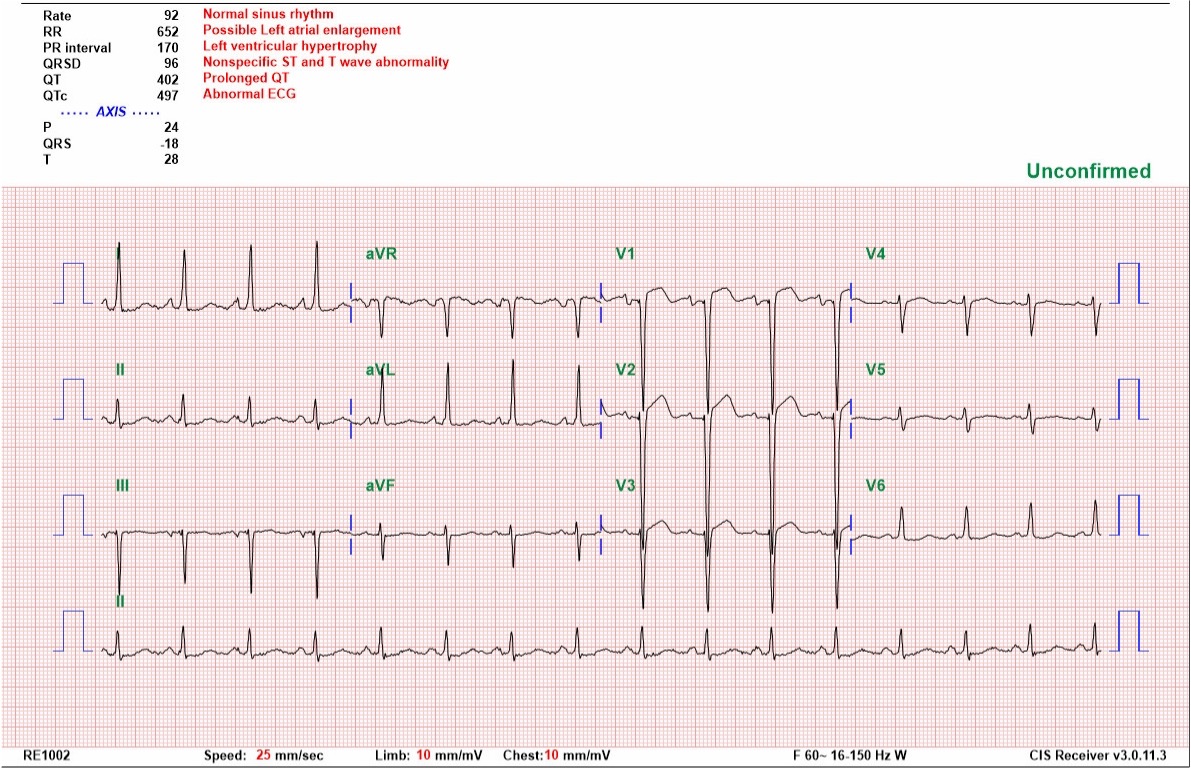
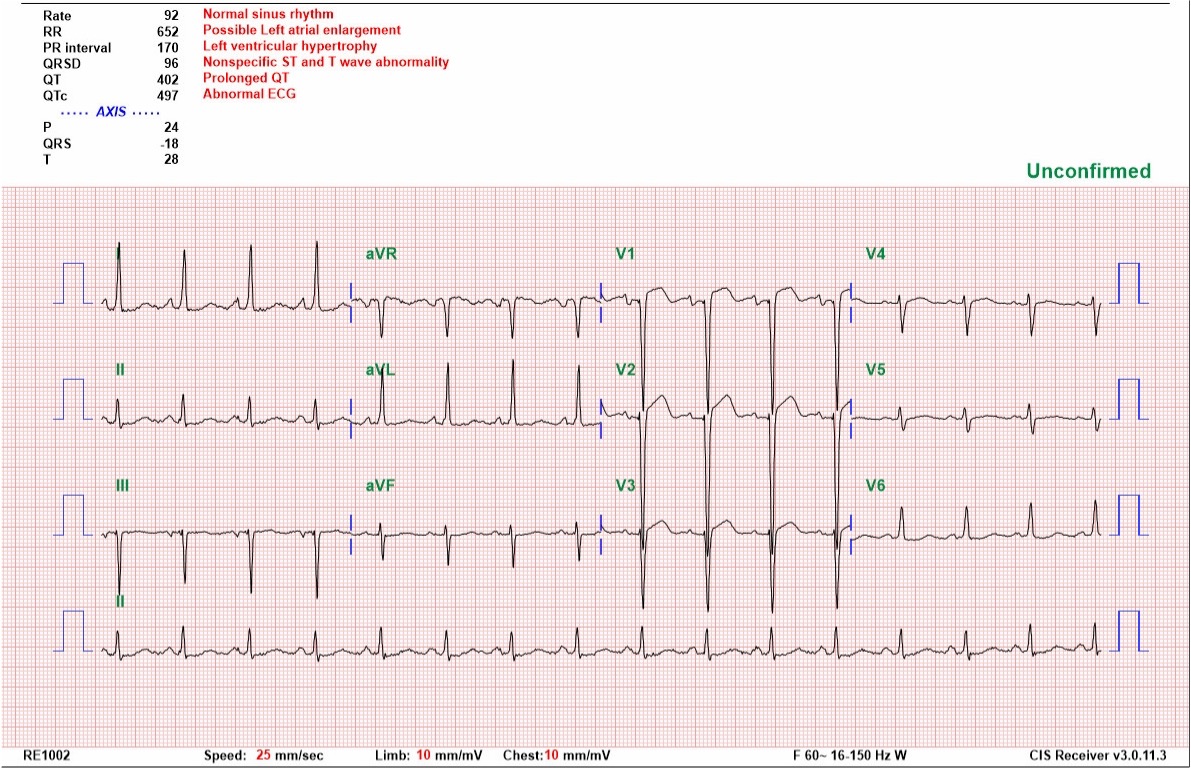
Relevant Test Results Prior to Catheterization
Laboratory studies on admission showed elevated NT-proBNP level to 6066 pg/mL and elevated cardiac enzyme level. Electrocardiography displayed Wellen’s syndrome. Chest radiography disclosed cardiomegaly and pulmonary edema. Echocardiography showed impaired LV systolic function (LVEF 30%) with septal and anterior wall hypokinesia. Acute decompensated heart failure and non-ST elevation myocardial infarction were impressed, and he was admitted to the ICU for close monitoring and management.
Relevant Catheterization Findings
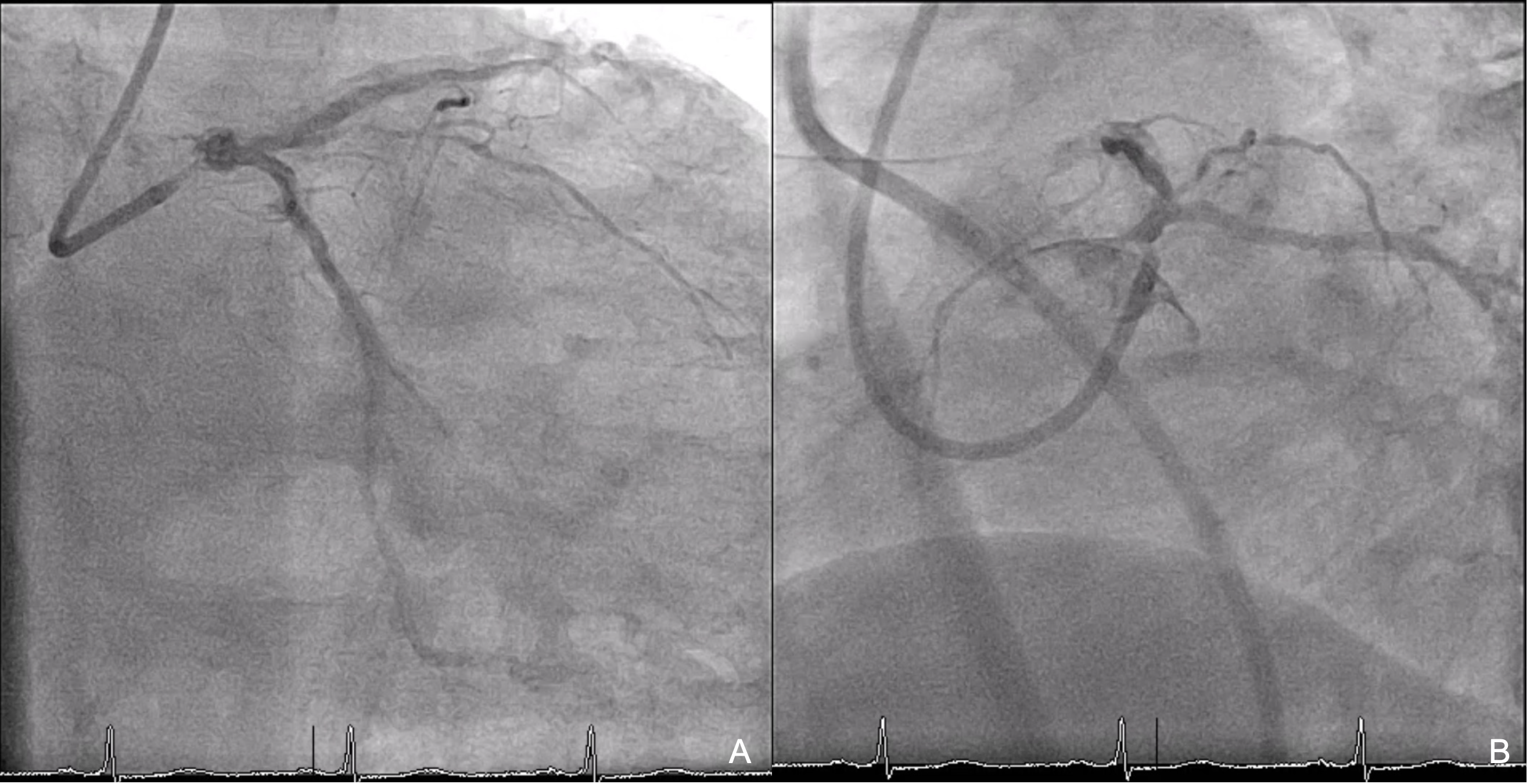
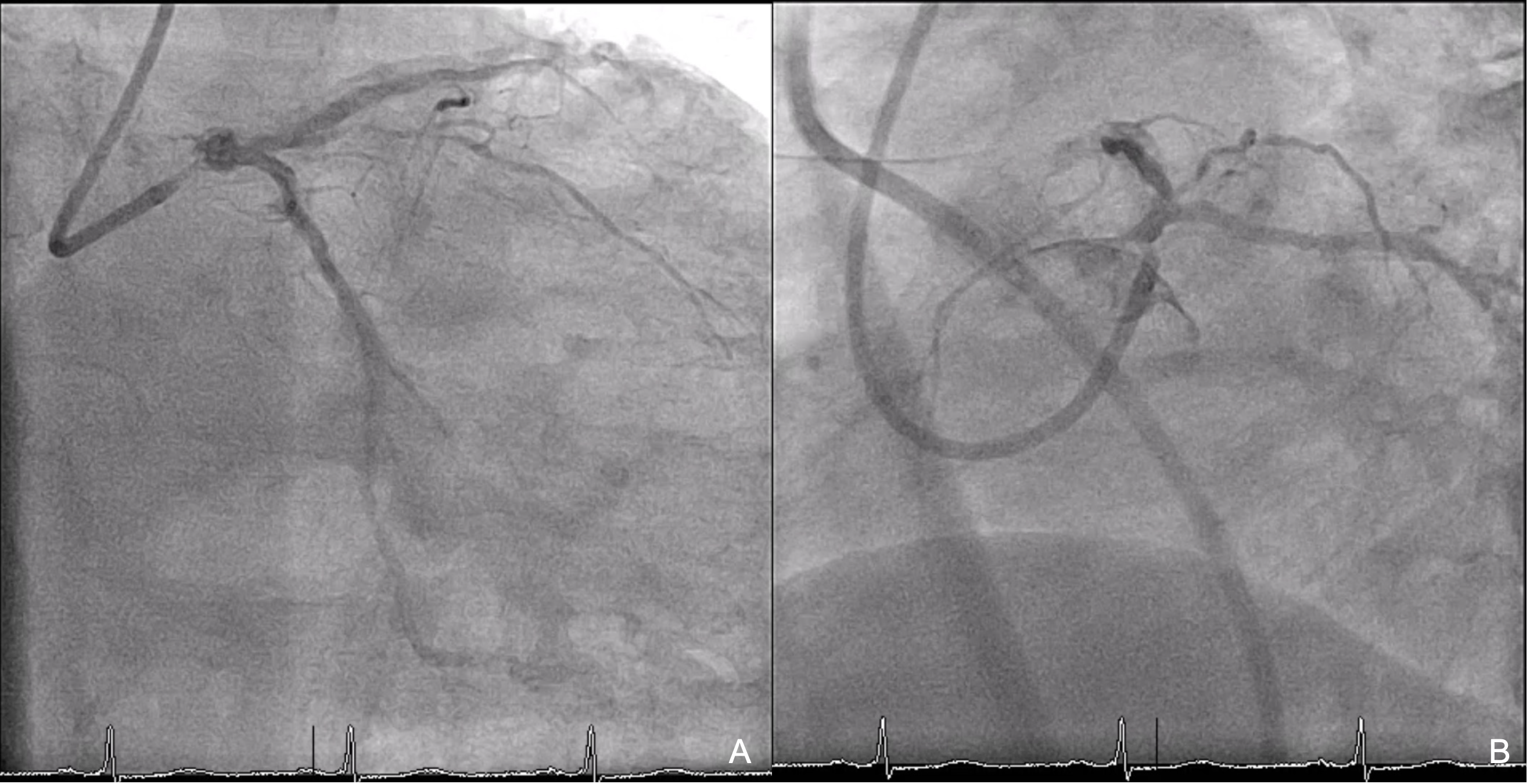
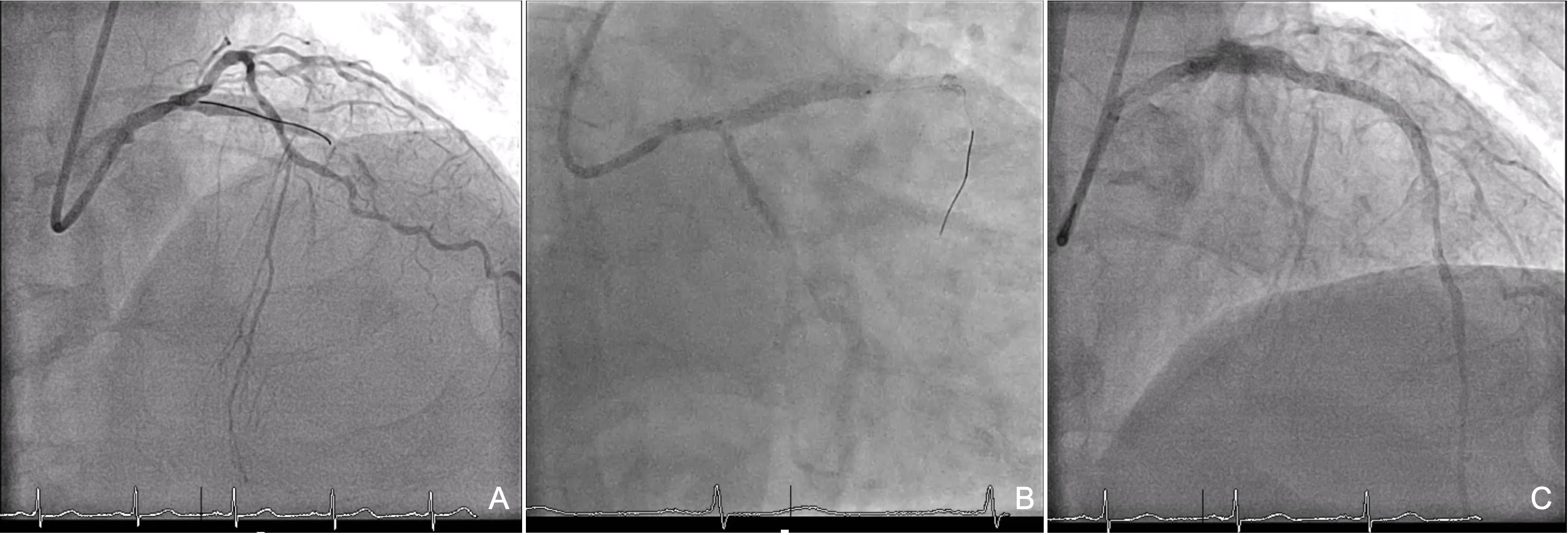
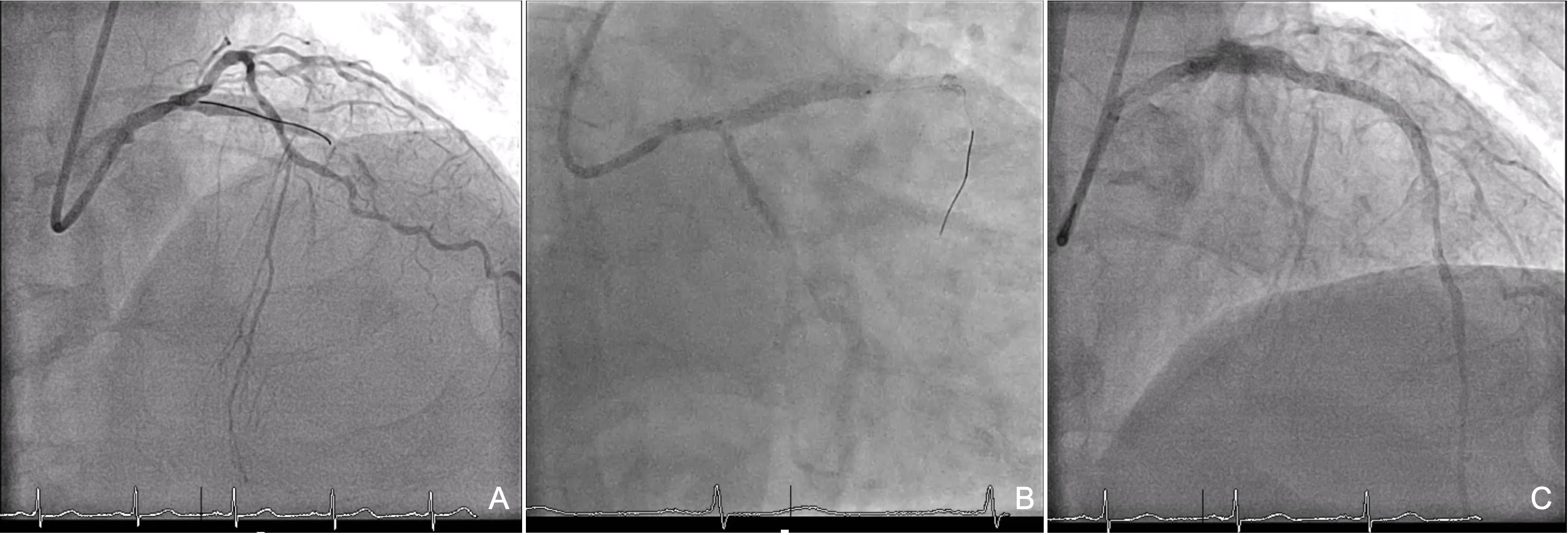
The CAG performed via the right radial artery revealed coronary artery disease (CAD) with double vessel disease (DVD) with diffusely heavily calcified left anterior descending coronary artery (LAD) with chronic total occlusion (CTO) over the middle LAD and bridging collateral, and stenosis up to 80% over a posterolateral branch of the right coronary (RCA).
Interventional Management
Procedural Step
The LMCA was engaged with a 6 Fr EBU 3.5 guide catheter; a Runthrough Hypercoat guide wire (GW) failed to be advanced to the distal LAD. A 1.8 Fr 180 cm Finecross microcatheter (MC) was used with its tip placed distally to the middle LAD CTO cap, and the GW was successfully advanced to distal LAD. Due to uncrossable lesions, a total of 9 runs of rotational atherectomy (RA) were performed over proximal to distal LAD using a 1.5 mm Rota burr with a RotaFloppy GW, with a rotational speed of 150 k to 165 k rpm. Post-RA intravascular ultrasound (IVUS) showed cracked circumferential calcification from distal LAD to ostium with reverberation sign. After adequate lesion preparation, distal to ostial LAD was stented with two sequential drug-eluting stents, followed by post-dilation. Post-stenting IVUS showed good stent expansion and apposition; there was no stent edge dissection. However, the angiogram showed dissection over distal LAD. Balloon inflation was performed with a 2.25 mm semi-compliant (SC) BC at distal LAD at nominal pressure for 30 seconds. However, after several minutes of monitoring, the angiogram still showed dissection with limited flow. Another 2.25 mm drug-eluting stent was deployed over distal LAD. The final angiogram showed good results with TIMI 3 blood flow. The patient tolerated the procedure well without immediate complications and was discharged uneventfully the next day. He reported no adverse event during follow-up in the following months.
Case Summary
Intravascular imaging devices offer significant advantages in PCI for chronic total occlusion (CTO) lesions with diffusely heavy calcification, enabling calcium assessment, real-time guidewire navigation, and optimized stenting strategies. Severe calcification in atherosclerotic plaques is a major factor contributing to suboptimal PCI outcomes, making thorough lesion preparation through debulking and modification crucial. Rotational atherectomy (RA) is widely used for heavily calcified lesions, particularly in uncrossable cases. IVUS provides critical insights into guidewire bias and optimal burr sizing, enhancing procedural efficacy and safety.


