Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-069
Extraordinary Lesions Require Extraordinary Measures: A Chance Worth the Risks?
By Chiquita Febby Pragitara, Chevanka Ursula Ayunindya, Muammar Emir Ananta, Arief Wibisono, Evit Ruspiono, Tri Astiawati, Adriyawan Widya Nugraha, Fitranti Suciati Laitupa
Presenter
Chiquita Febby Pragitara
Authors
Chiquita Febby Pragitara1, Chevanka Ursula Ayunindya2, Muammar Emir Ananta3, Arief Wibisono1, Evit Ruspiono1, Tri Astiawati1, Adriyawan Widya Nugraha1, Fitranti Suciati Laitupa1
Affiliation
Dr. Iskak General Hospital, Indonesia1, Airlangga University, Indonesia2, Cempaka Putih Jakarta Islamic Hospital, Indonesia3,
View Study Report
TCTAP C-069
Coronary - Complex PCI - CTO
Extraordinary Lesions Require Extraordinary Measures: A Chance Worth the Risks?
Chiquita Febby Pragitara1, Chevanka Ursula Ayunindya2, Muammar Emir Ananta3, Arief Wibisono1, Evit Ruspiono1, Tri Astiawati1, Adriyawan Widya Nugraha1, Fitranti Suciati Laitupa1
Dr. Iskak General Hospital, Indonesia1, Airlangga University, Indonesia2, Cempaka Putih Jakarta Islamic Hospital, Indonesia3,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 72 year-old man was referred to our emergency room with anteroseptal ST-elevation myocardial infarction (STEMI). He reported severe chest pain radiating to the back and left shoulder, accompanied by diaphoresis, which had persisted for the past 7 hours. He admitted to having a similar attack 3 months earlier and had been experiencing mild exertional chest pain for a year. His only identified coronary artery disease risk factor was smoking. BP 180/90 mmHg, HR 86 bpm, SpO2 98%, VAS 10, BMI 20.81
Relevant Test Results Prior to Catheterization
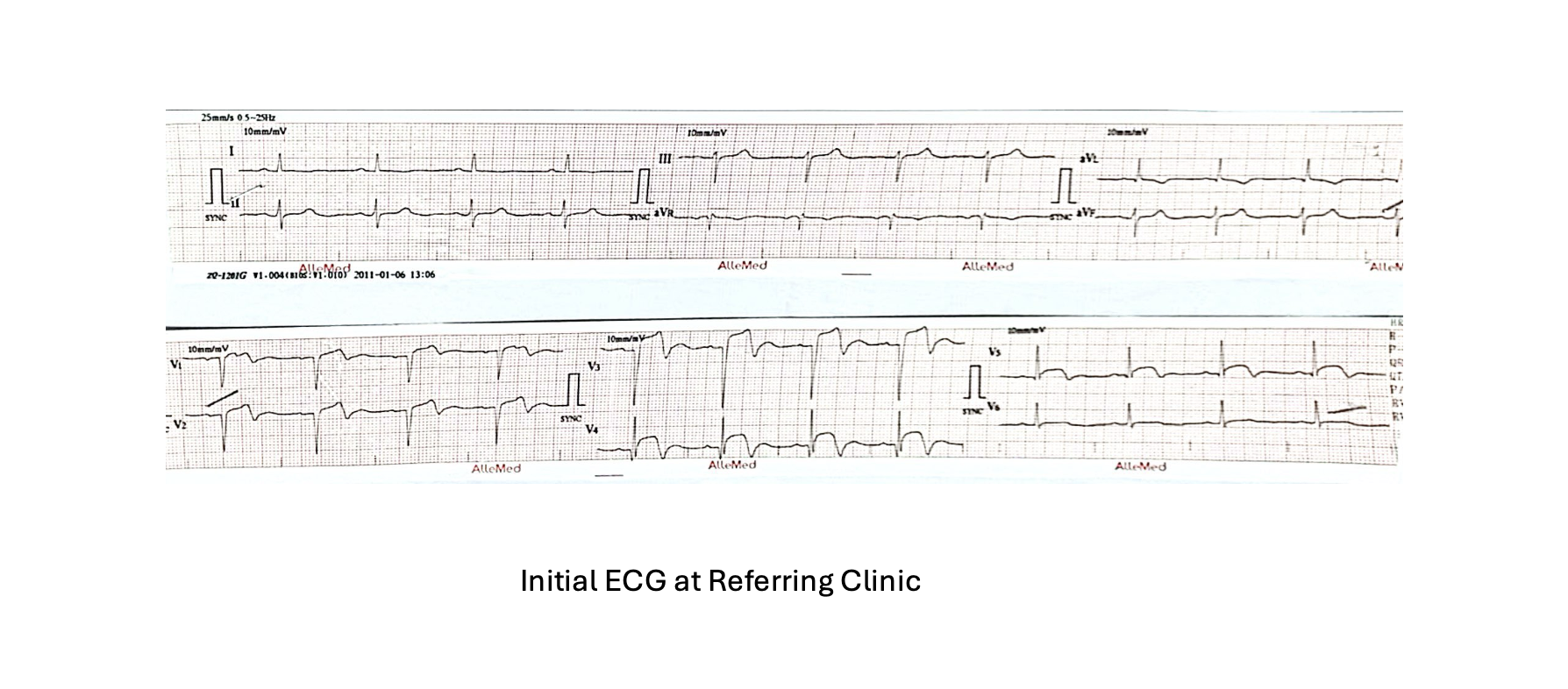
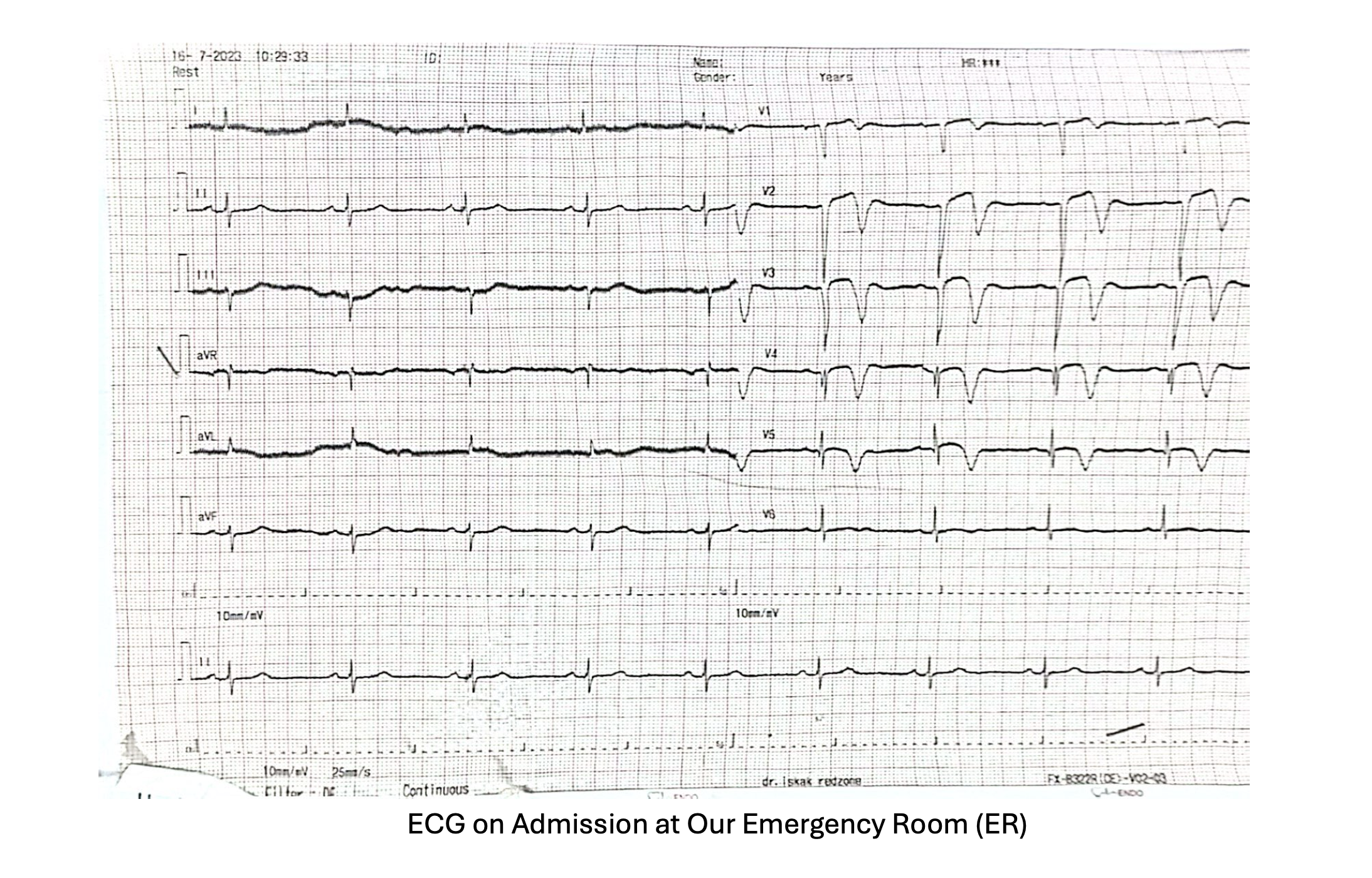
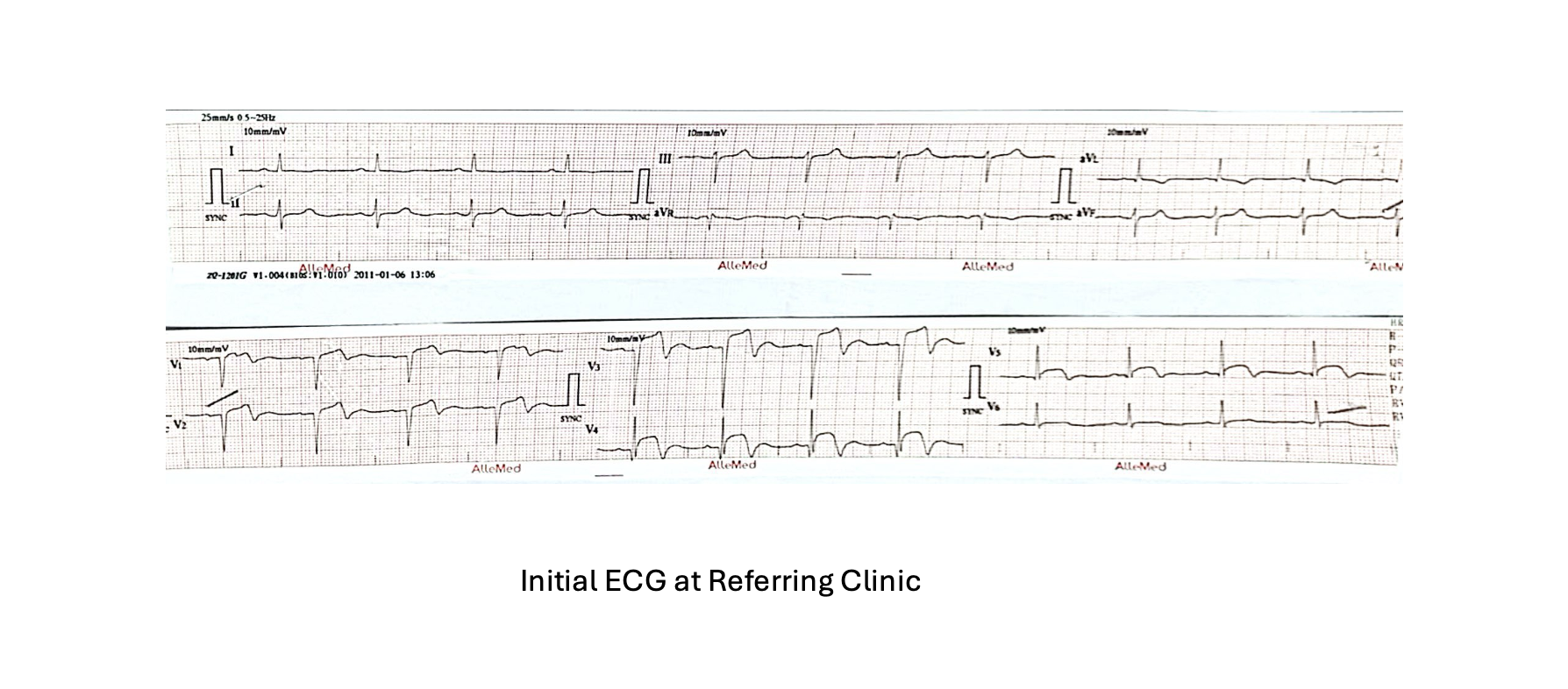
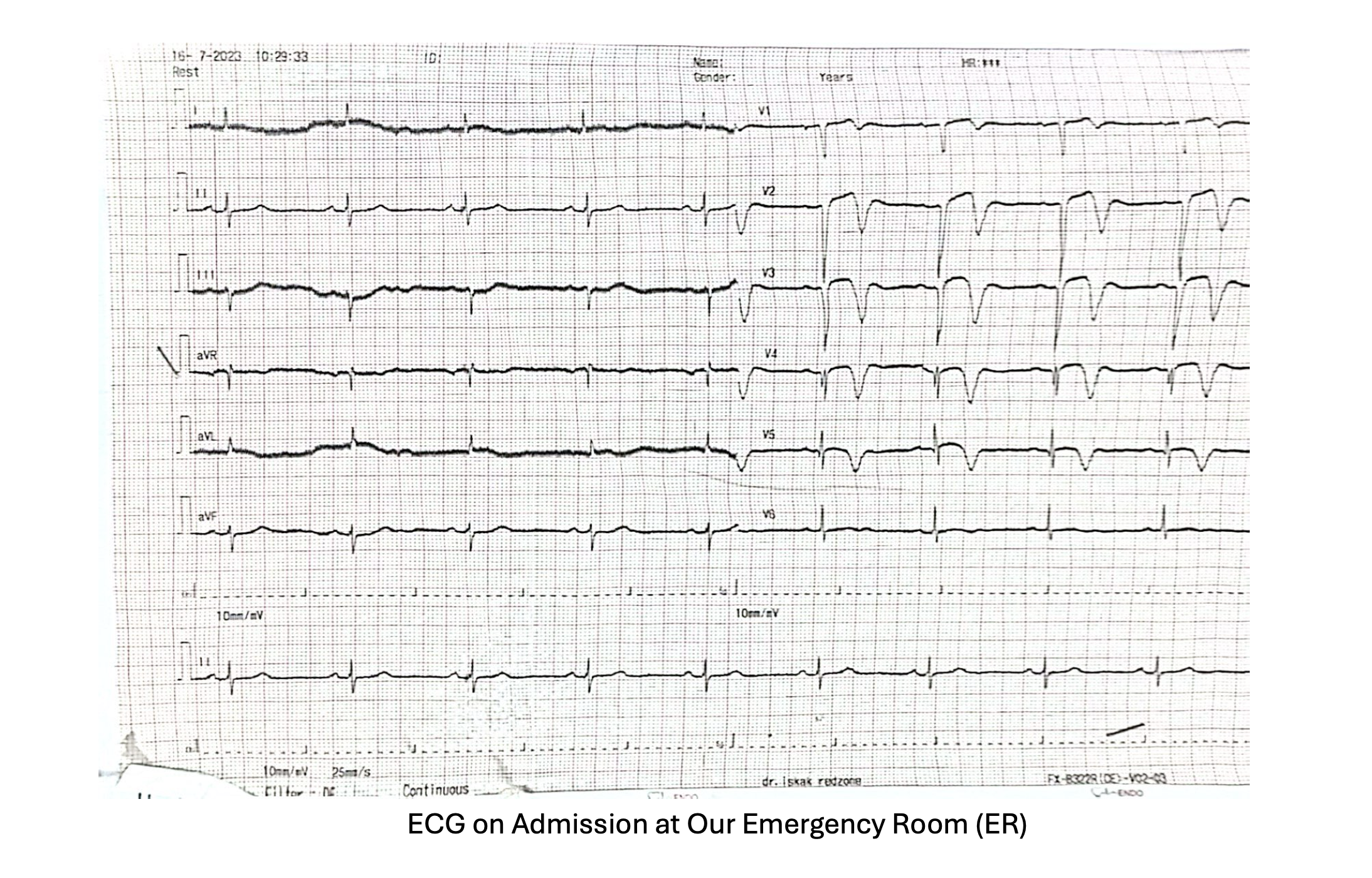
Physical examination and chest radiograph revealed signs of congestion. The initial ECG at the referring clinic showed anteroseptal ST elevation (V1-V4). Meanwhile, an ECG performed in our emergency room hours later revealed inverted T waves in V1-V5 leads, consistent with STEMI evolution. Both cardiac enzymes were elevated, Hs-Troponin I was 2987.2 ng/L and CKMB was 59 ng/mL. Other laboratory results were within normal limits.


Relevant Catheterization Findings
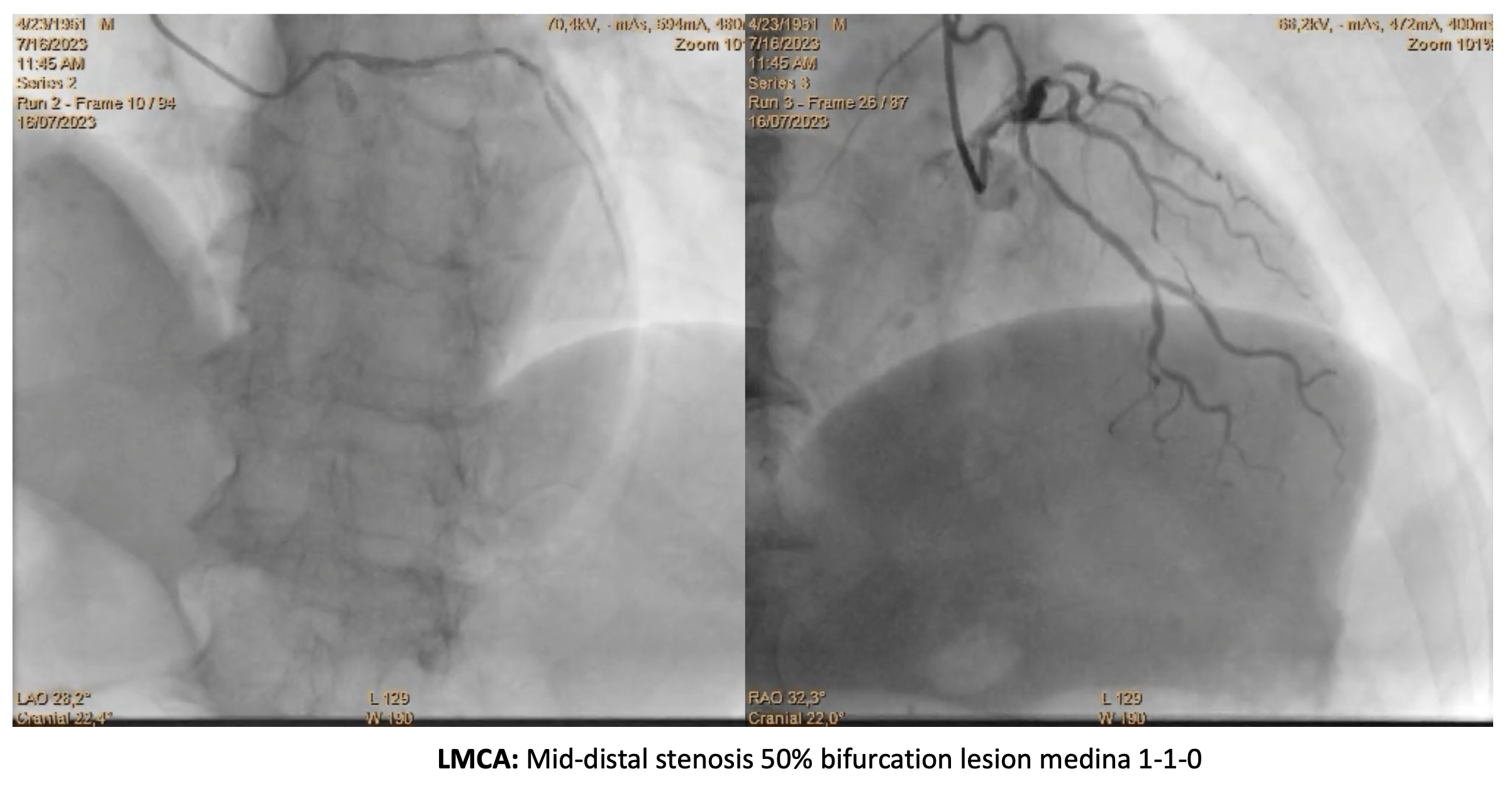
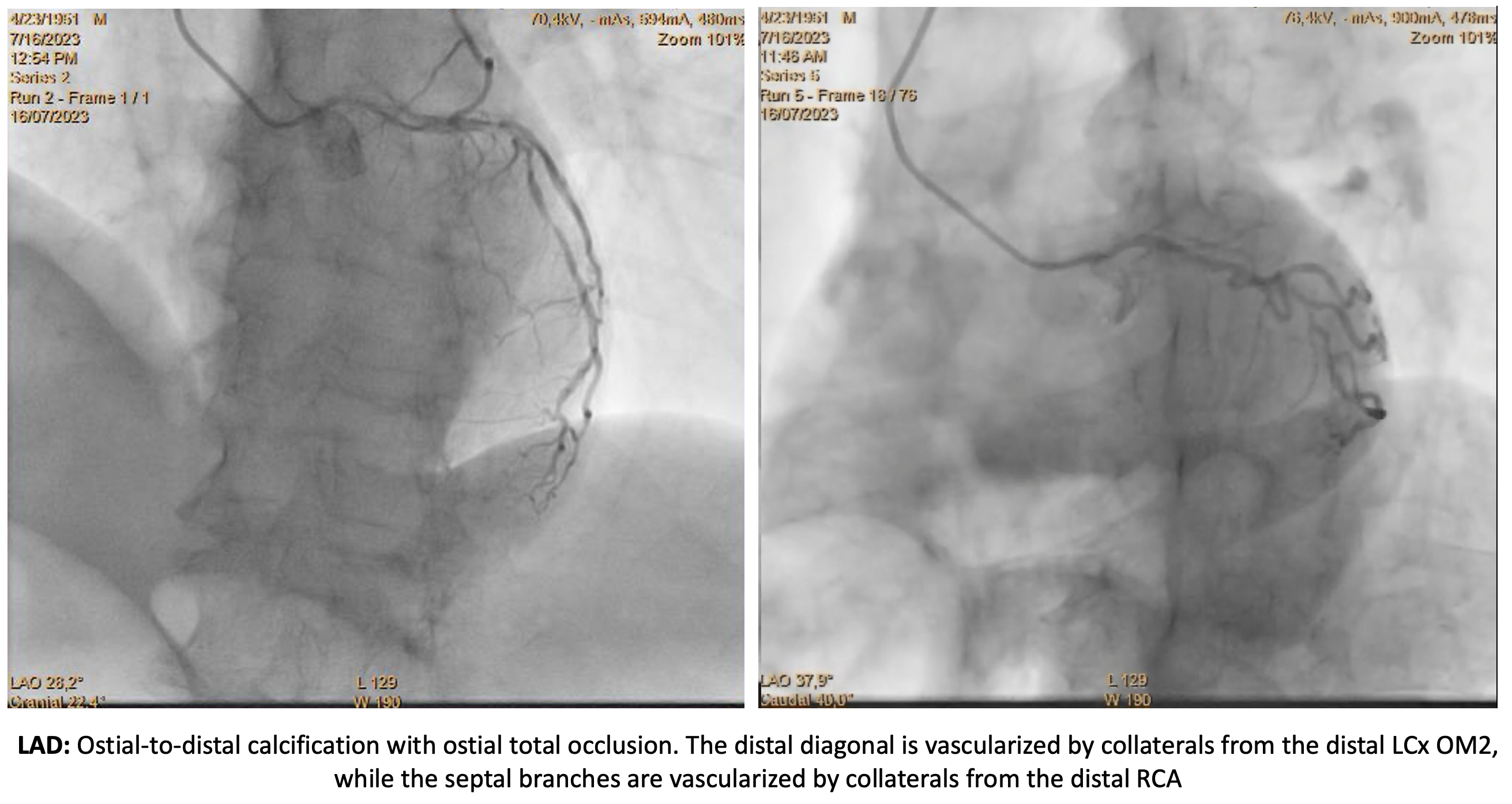
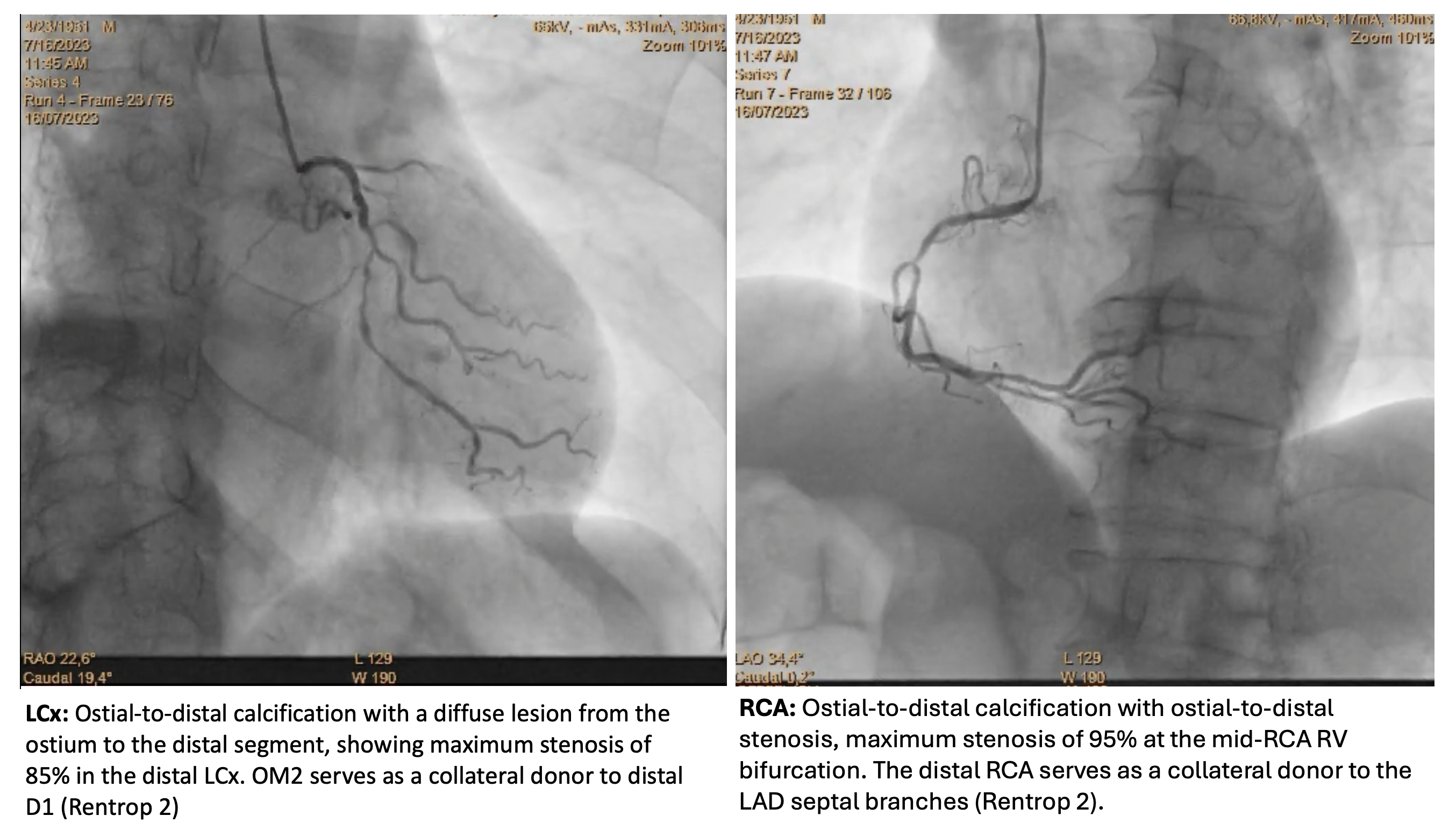
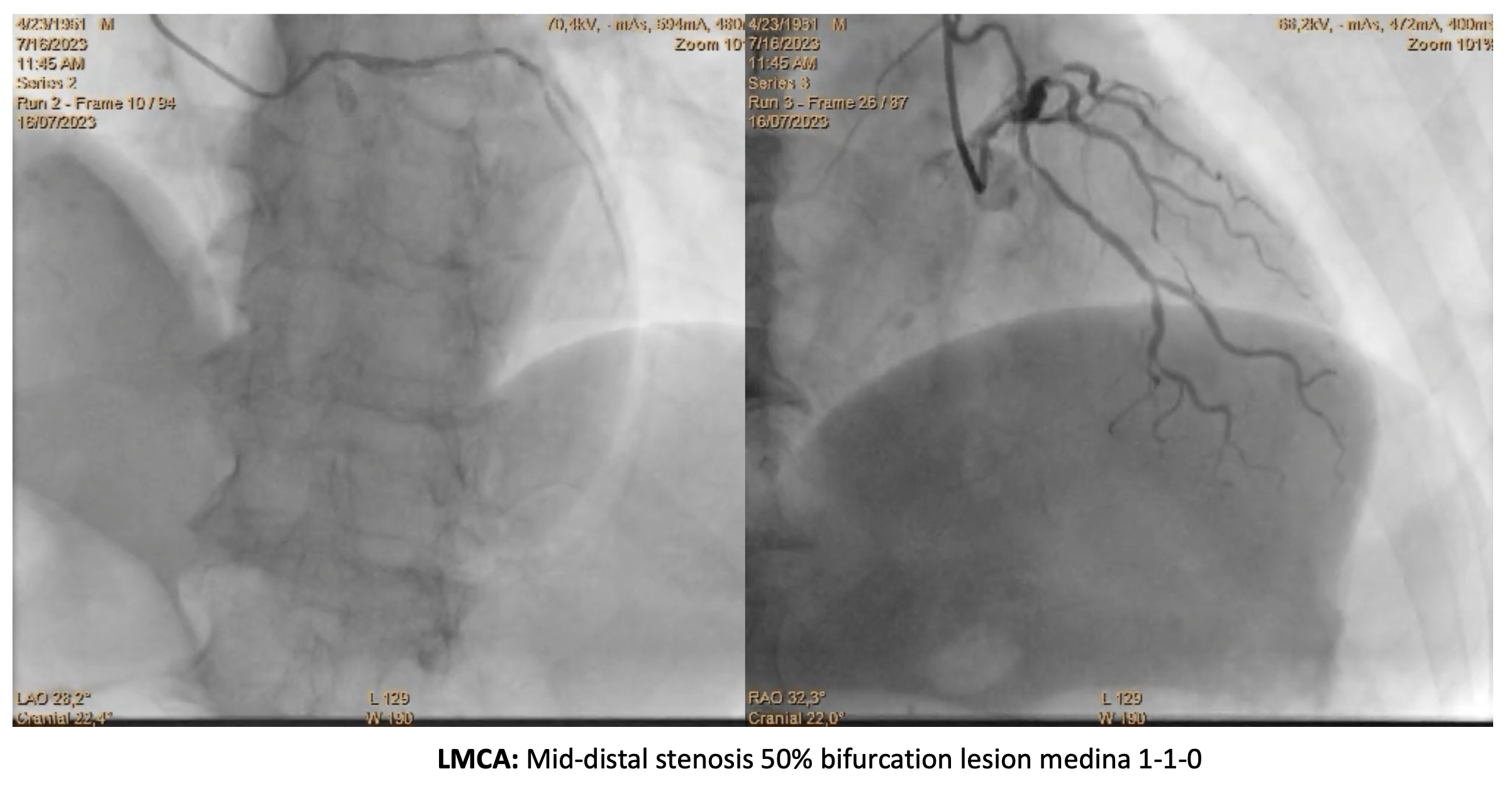
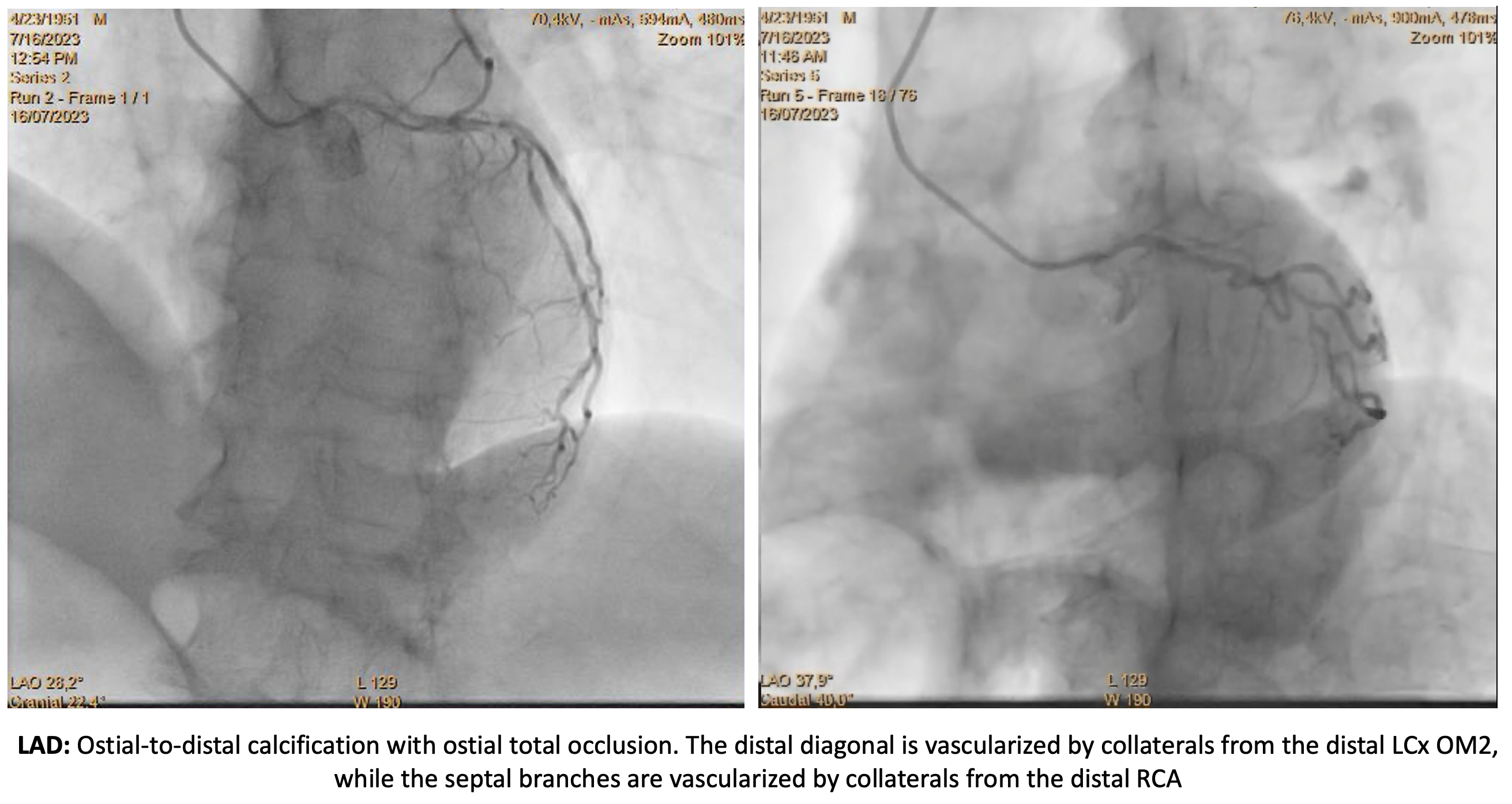
CAG revealed CAD3VD LM disease Medina 1:1:0, CTO ostial LAD and significant calcification in ostial-distal of all vessels. 95% critical stenosis was found in mid-RCA RV bifurcation, 85% maximum stenosis in distal LCx. Distal OM2 provided collateral flow to distal D1 (Rentrop 2) and distal RCA to LAD septals (Rentrop 2). EURO Score II was 1.16%, J-CTO 4, PROGRESS CTO 2, SYNTAX Score I 64. However, CABG was not performed due to patient refusal and our center's limited facilities for urgent CABG.
Interventional Management
Procedural Step
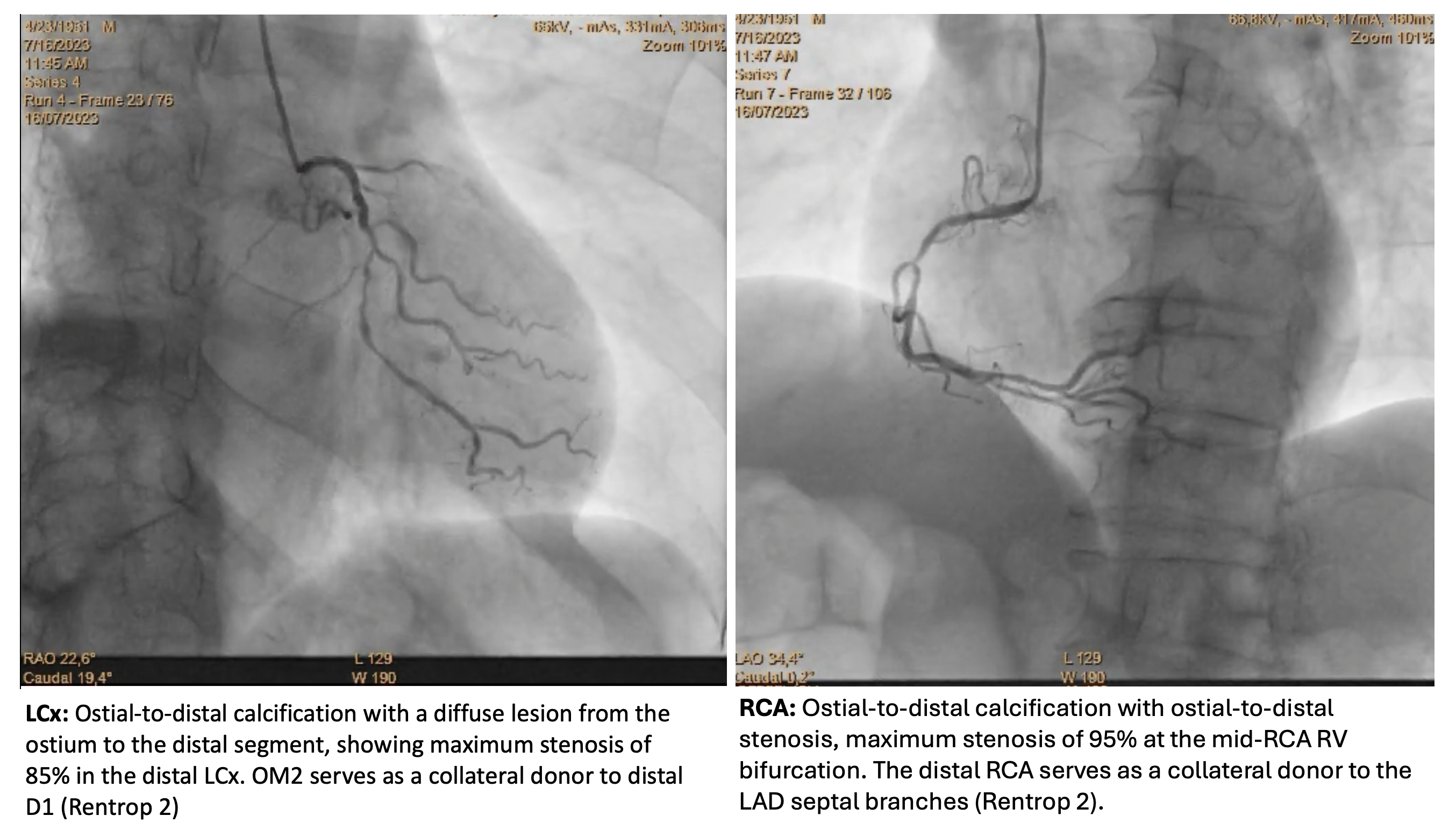
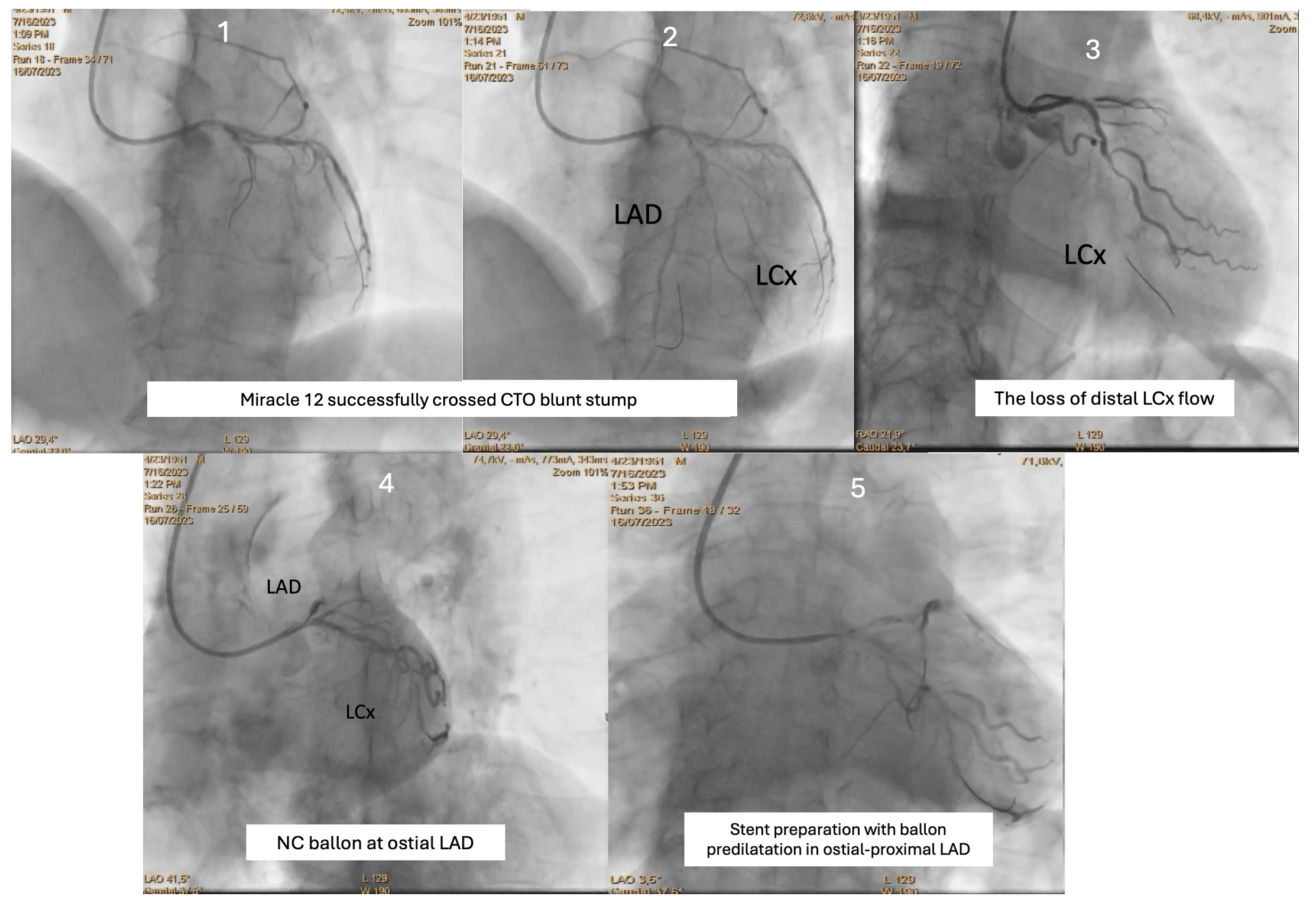
Based on an ambiguous proximal cap, >20 mm lesion length, calcified distal vessels and contralateral epicardial collaterals, we planned to first cross the ostial LAD CTO using an antegrade escalated wiring approach, followed by provisional MB stenting.Primary PCI was initiated by engaging GC EBU 3.5 6F in the ostial LM, with GW Runthrough Hypercoat advanced to protect LCx flow. After several attempts using Miracle 12 wire and Crusade, we successfully crossed the blunt stump of the CTO. Suddenly, CTO debris fell into distal LCx twice, leading to no flow and VF, but was successfully flushed into distal OM3, restoring TIMI flow 3. The initial strategy to cross the LAD CTO resulted in repeated LCx flow loss. To prevent further compromise, a DES 2.75×33mm was deployed in proximal-distal LCx after re-establishing LAD flow. Given the risk of disrupting collateral flow, LAD CTO revascularization was prioritized.Balloon predilatation in the mid-LM to proximal LAD was performed using a 2.75×15mm NC balloon. Provisional stenting with a DES 3.5×15 mm was then performed in the mid-LM to proximal LAD, followed by POT using an NC balloon. TIMI flow grade 3, 0% residual stenosis was achieved in both coronaries.3 days after PPCI, the patient experienced recurrent chest pain and elevated troponin level. DCA showed patent stents. Echocardiography evaluation 5 days later showed preserved LV systolic function and global normokinetic. The patient was discharged and scheduled for staged RCA PCI.
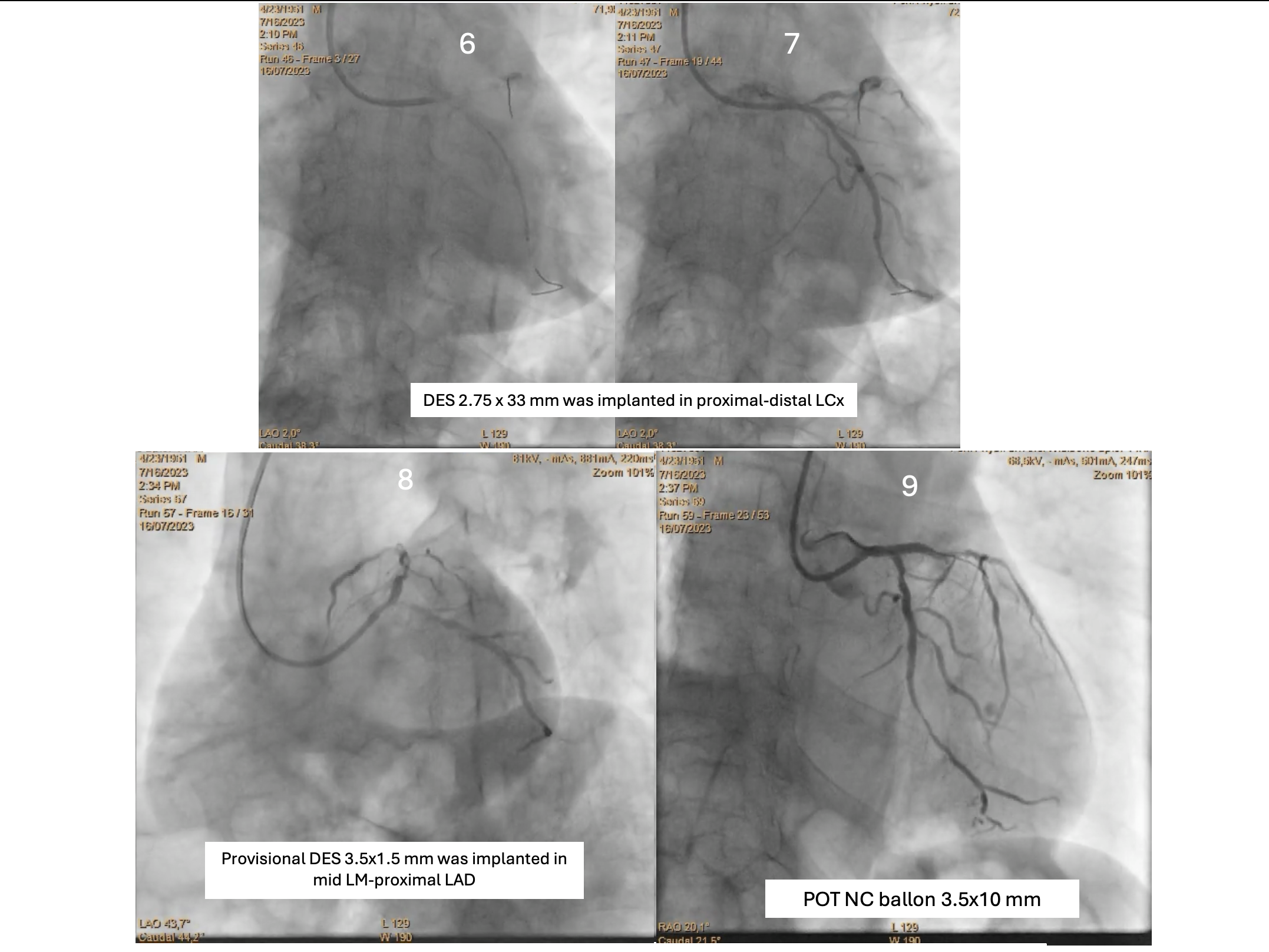
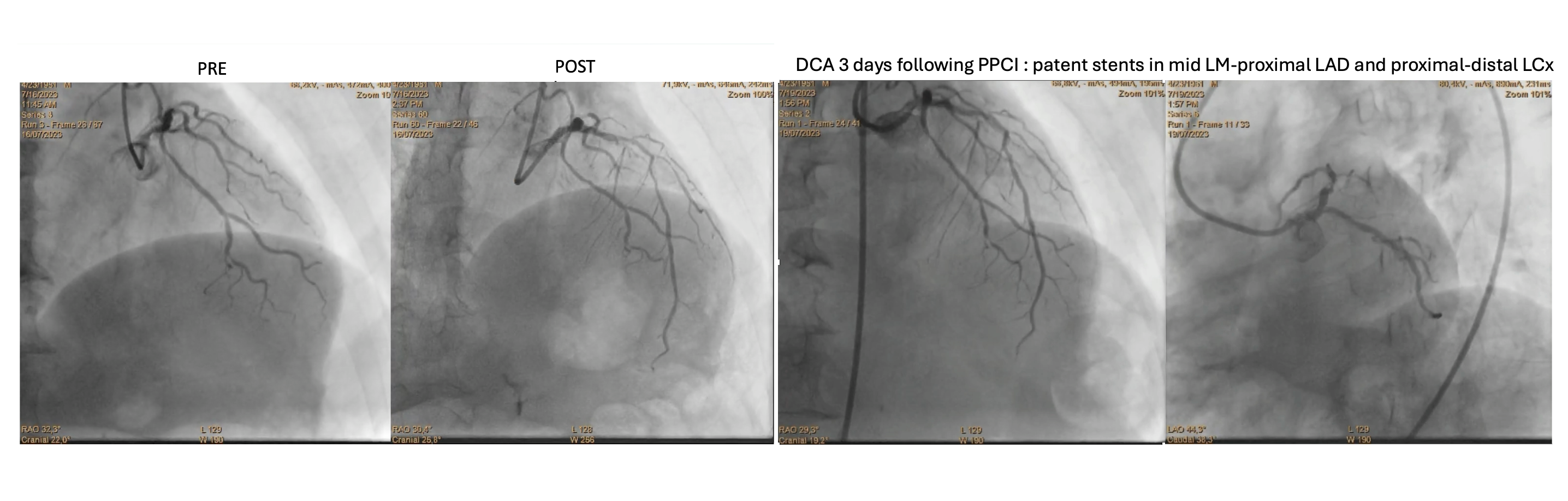
Case Summary
STEMI in the elderly is inherently complex. The angiography findings of CAD3VD LM disease and CTO LAD further compounded the challenges. Managing this case using a flip-flop technique, a dynamic switching intervention, between LAD as the culprit lesion and LCx as the collateral donor, can aid in assessing difficult segments while preserving collateral circulation. This dynamic strategy proved crucial in achieving adequate revascularization while minimizing MACE in acute settings, emphasizing the pitfalls of solely focusing on LCx stenting could compromise collateral flow to the LAD.


