Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-158
Distal Coronary Artery Perforation Management, Case Report
By Ahmad Bakhtiar Md Radzi, Ahmad Firdaus Zakaria, Muhammad Hanis Muhmad Hamidi, Huzairi Sani, Khairul Shafiq Ibrahim, Raja Ezman Faridz Raja Shariff, Sazzli Shahlan Kasim, Abdul Wahab Undok
Presenter
Ahmad Bakhtiar Md Radzi
Authors
Ahmad Bakhtiar Md Radzi1, Ahmad Firdaus Zakaria1, Muhammad Hanis Muhmad Hamidi1, Huzairi Sani1, Khairul Shafiq Ibrahim1, Raja Ezman Faridz Raja Shariff1, Sazzli Shahlan Kasim1, Abdul Wahab Undok2
Affiliation
Universiti Teknologi MARA, Malaysia1, KPJ Rawang Specialist Hospital, Malaysia2,
View Study Report
TCTAP C-158
Coronary - Complication Management
Distal Coronary Artery Perforation Management, Case Report
Ahmad Bakhtiar Md Radzi1, Ahmad Firdaus Zakaria1, Muhammad Hanis Muhmad Hamidi1, Huzairi Sani1, Khairul Shafiq Ibrahim1, Raja Ezman Faridz Raja Shariff1, Sazzli Shahlan Kasim1, Abdul Wahab Undok2
Universiti Teknologi MARA, Malaysia1, KPJ Rawang Specialist Hospital, Malaysia2,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 77-year-old female was electively admitted for multi-vessel complex coronary angioplasty. She presented with left sided chest pain for 2 weeks prior to this admission and was treated as non-ST elevation myocardial infarction. She had hypertension and dyslipidemia for 20 years. Physical examinations were unremarkable.




Relevant Test Results Prior to Catheterization
The patient declined for coronary artery bypass graft surgery for severe 3 vessel disease with a high syntax score of 57.
Relevant Catheterization Findings
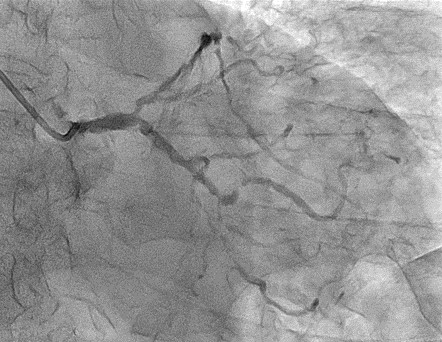
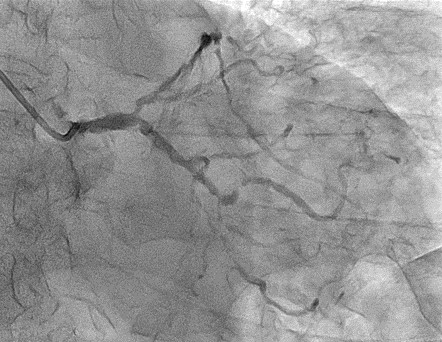
A repeat coronary angiogram of the right system revealed severe diffuse disease of the right coronary artery (RCA) from proximal until distal RCA.
Interventional Management
Procedural Step
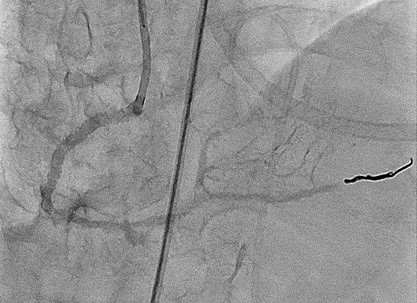
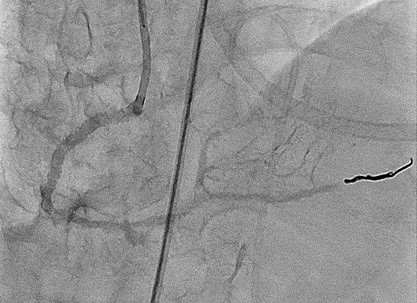
Coronary angioplasty was performed with Judkins Right catheter 3.5/6F via right radial artery. A Sion Blue 0.014 inch coronary wire was advanced until distal posterior descending artery (PDA). The distal RCA-PDA and mid RCA were inserted with a drug coating balloon Magic Touch 2.5/40mm and 2.75/40mm respectively after lesion preparations. Proximal RCA was implanted with a drug eluting stent Synergy 2.75/28mm. Subsequent angiogram images revealed a contrast extravasation into the pericardial sac with type III perforation at distal PDA likely due to the injury caused by the coronary wire. The leak was confirmed with echocardiography. Subsequently, the patient developed cardiac tamponade causing cardiogenic shock requiring inotropic support and emergency pericardiocentesis was performed. Guiding catheter was changed to AL 0.75 6F via right femoral artery for better support. Prolonged coronary balloon inflation proximal to the perforation site was unsuccessful to seal it. Penumbra Ruby coil 2mm x 4cm was deployed at the perforation area via Terumo Progreat microcatheter system which managed to seal the distal perforation. A total of 1.5L of hemorrhagic pericardial fluid drained and the patient was transfused with 3 unit pack cell. The patient was transferred to intensive cardiac care unit and subsequently managed to be discharged after 5 days. Staged percutaneous coronary intervention to the left coronary system was planned later.


Case Summary
The risk factors of coronary artery perforation have been well-established, but it can be seen even though there are minimal or no risk factors. Precautions should be taken to minimize the risk of perforation while using stiff/hydrophilic wires. Early detection, immediate prolonged coronary balloon inflation, and other treatment modalities such as covered stent, autologous fat/ blood clot/ thrombin injection or coil embolization in our case are the cornerstones of the management of coronary artery perforation.


