Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-112
Case Report: Type IV In-Stent Restenosis in Unexpectedly Large Left Circumflex Artery
By Wee Pang Ng, Kwang How Ng, Jin Kiang Cheng, Wen Sheng Wong, Waye Young Lau, Ao Xiang Quek, Nur Hazurreen Harryzan, Jian Hao Sim, Gurudevan Mahadevan
Presenter
Wee Pang Ng
Authors
Wee Pang Ng1, Kwang How Ng1, Jin Kiang Cheng1, Wen Sheng Wong1, Waye Young Lau1, Ao Xiang Quek1, Nur Hazurreen Harryzan1, Jian Hao Sim1, Gurudevan Mahadevan1
Affiliation
Sultanah Aminah Hospital, Malaysia1,
View Study Report
TCTAP C-112
Coronary - Complex PCI - In-Stent Restenosis
Case Report: Type IV In-Stent Restenosis in Unexpectedly Large Left Circumflex Artery
Wee Pang Ng1, Kwang How Ng1, Jin Kiang Cheng1, Wen Sheng Wong1, Waye Young Lau1, Ao Xiang Quek1, Nur Hazurreen Harryzan1, Jian Hao Sim1, Gurudevan Mahadevan1
Sultanah Aminah Hospital, Malaysia1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
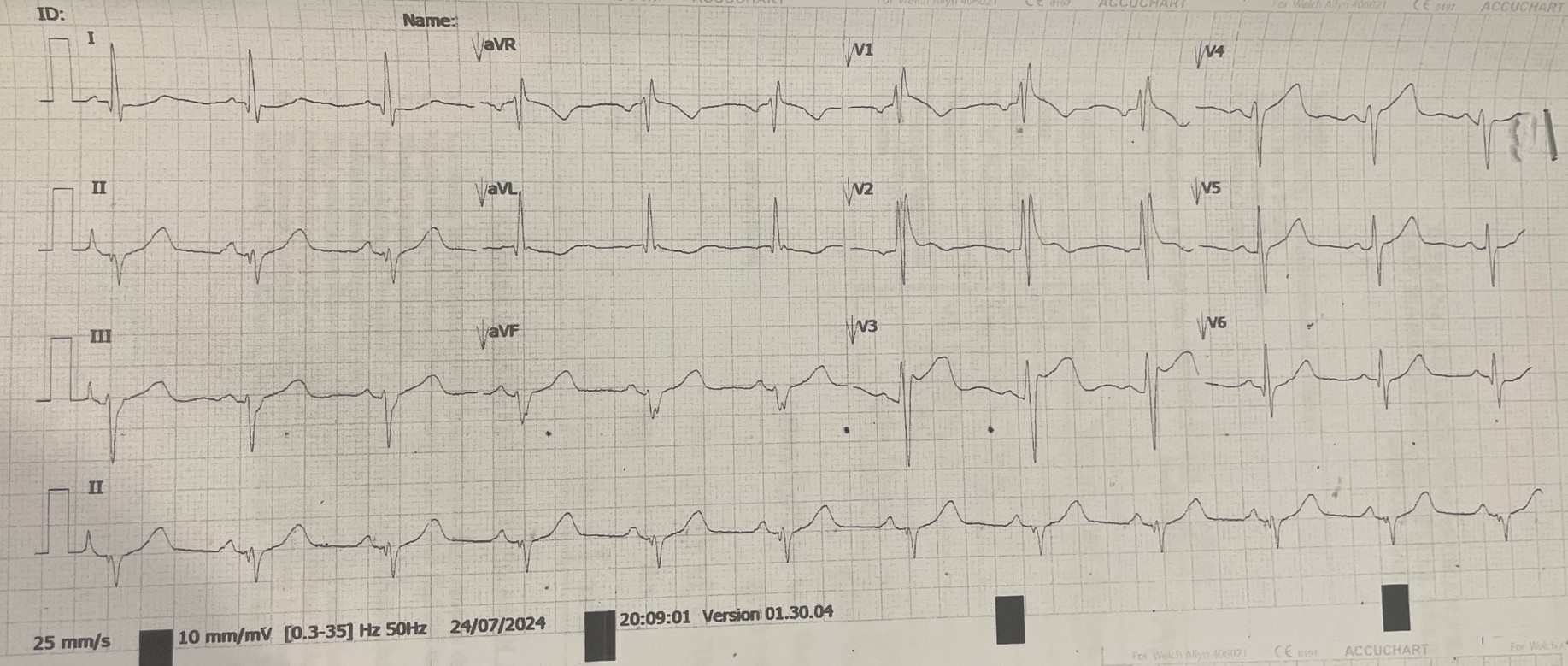
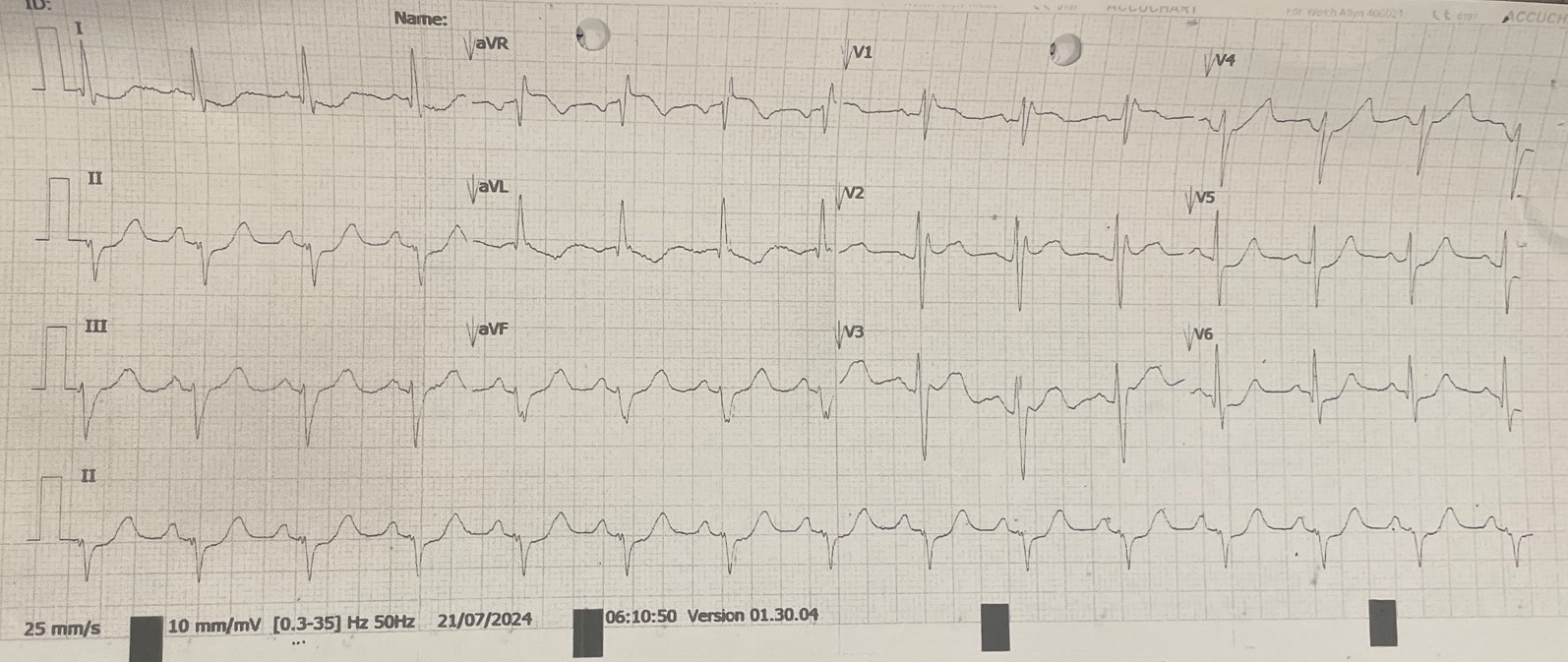
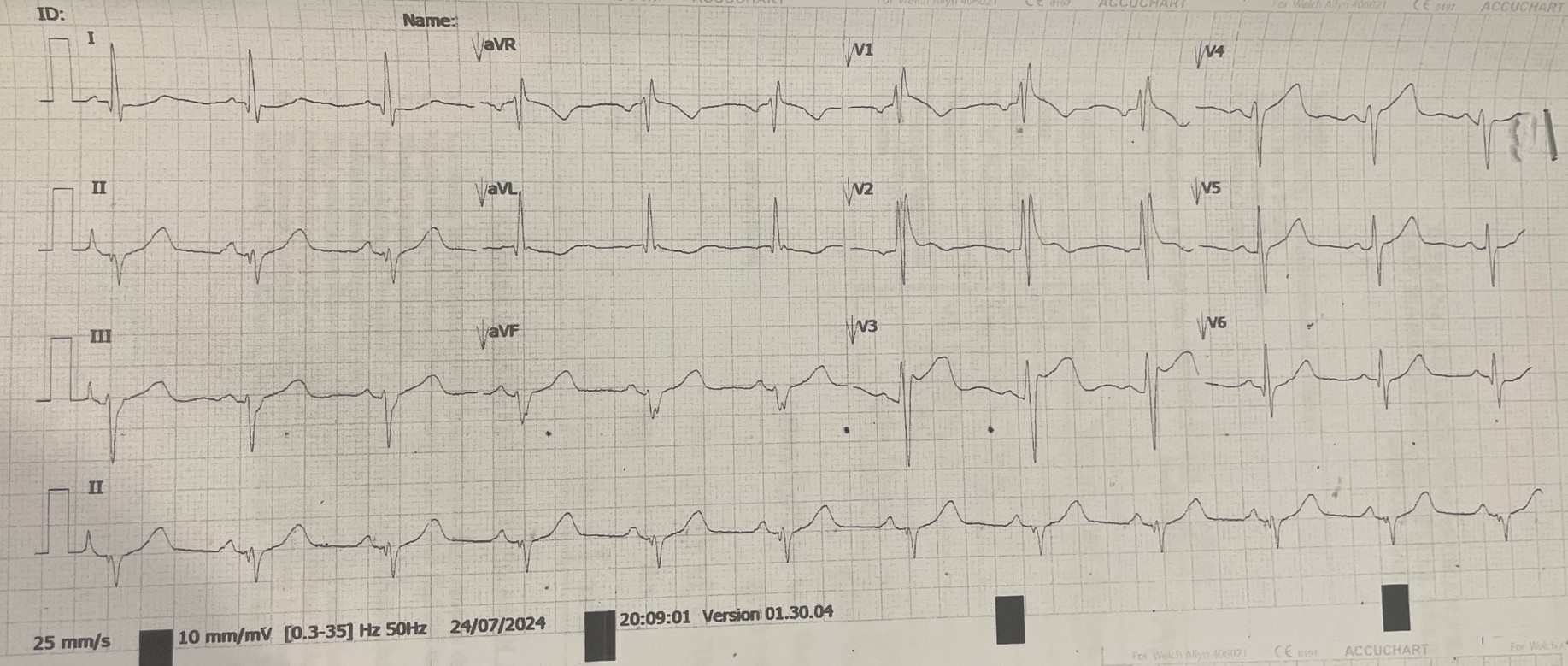
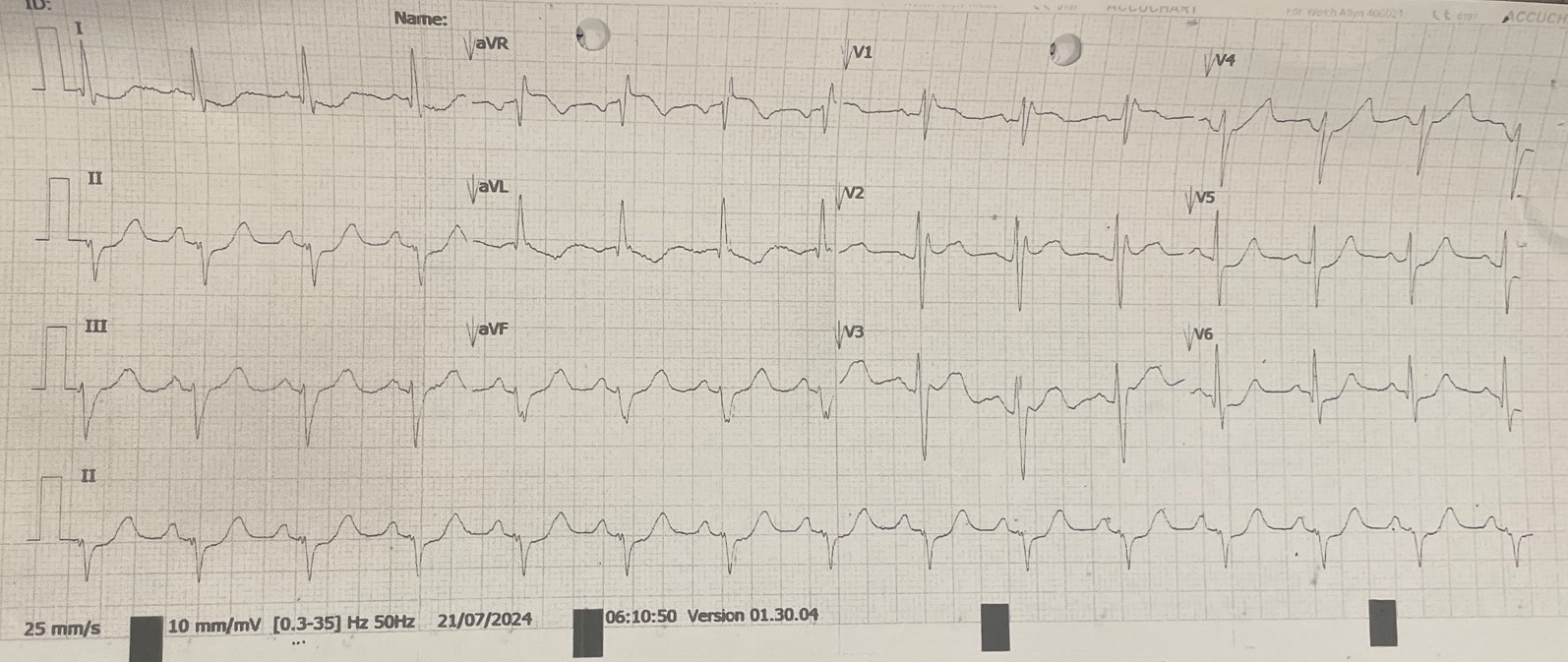
A case of a 44-year-old gentleman with epilepsy and coronary artery disease, who had angioplasty done to left circumflex artery with a DES in 2016. He complained of new onset of exertional angina for months and presented to hospital due to worsening symptoms. On presentation, he complained of ongoing chest pain, clinically not in failure with BP 100/62 mmHg, HR 74 bpm and SpO2 99% under room air. Lungs were clear, heart sound was normal with no murmur. ECG showed dynamic changes during chest pain.
Relevant Test Results Prior to Catheterization
Baseline ECG showed sinus rhythm with right bundle branch block. There were ST depression over lead I, aVL, V5 and V6 during chest pain. Laboratory examination showed creatine kinase level of 161 U/L (<200 U/L). Echocardiogram showed good LV systolic function, LVEF 65-70% with no RWMA, normal chamber size. He was treated for unstable angina and underwent in-hospital coronary angiography (CAG) and percutaneous coronary intervention (PCI) in view of recurrent angina.
Relevant Catheterization Findings
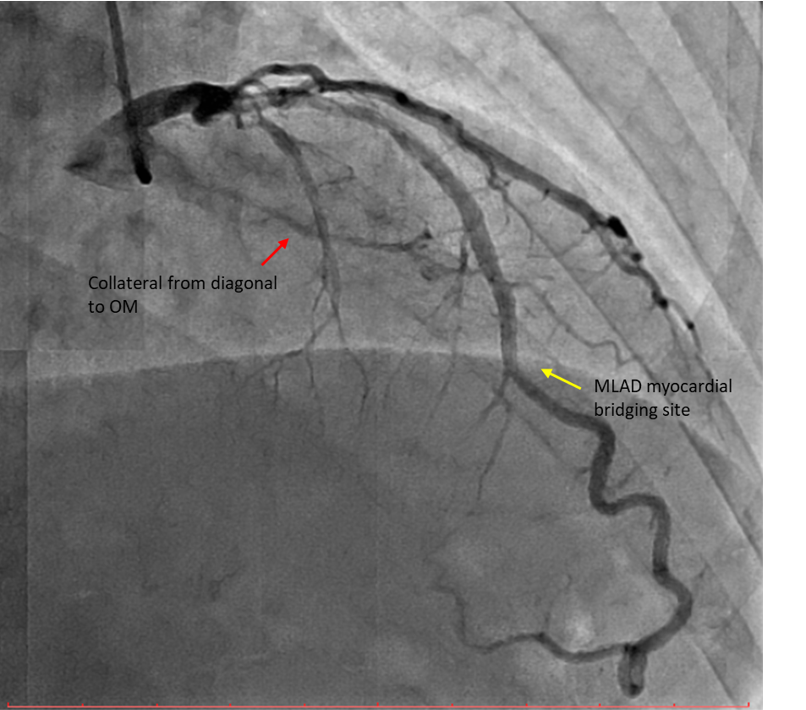
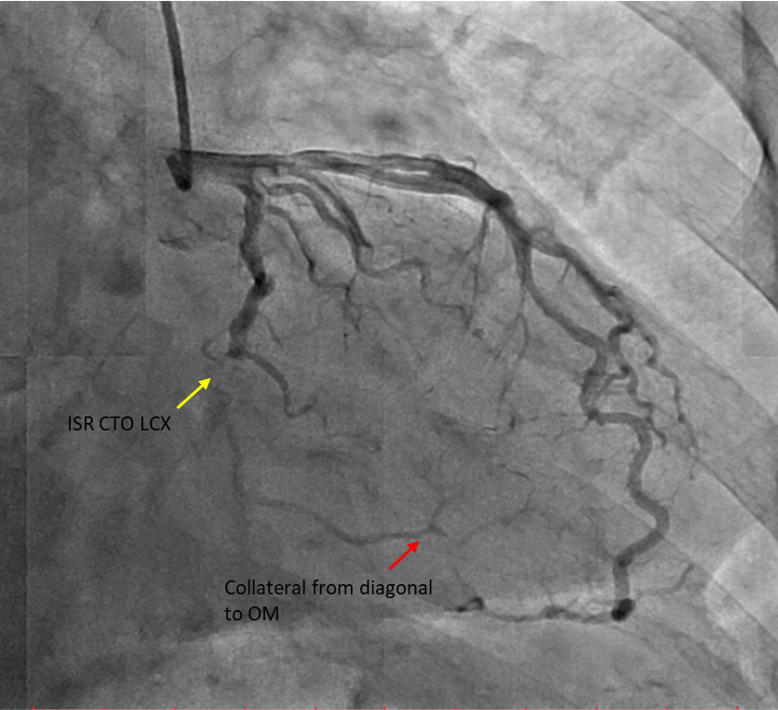
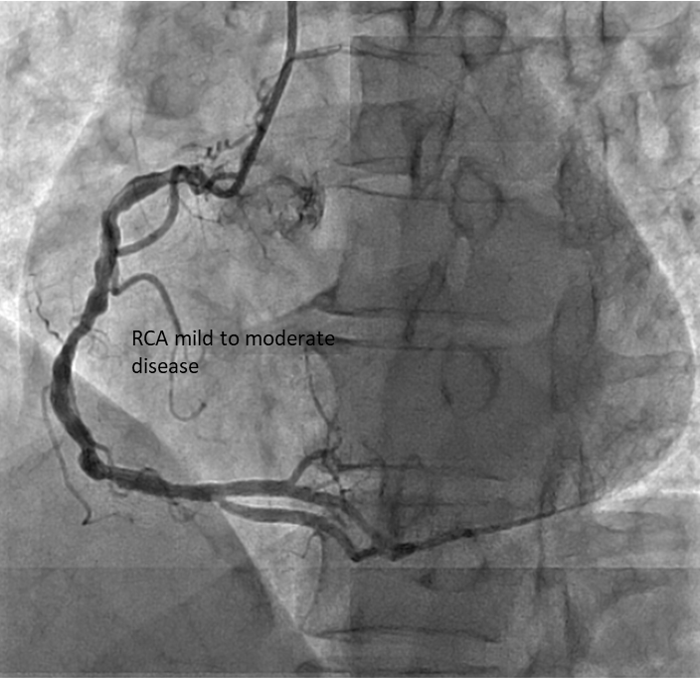
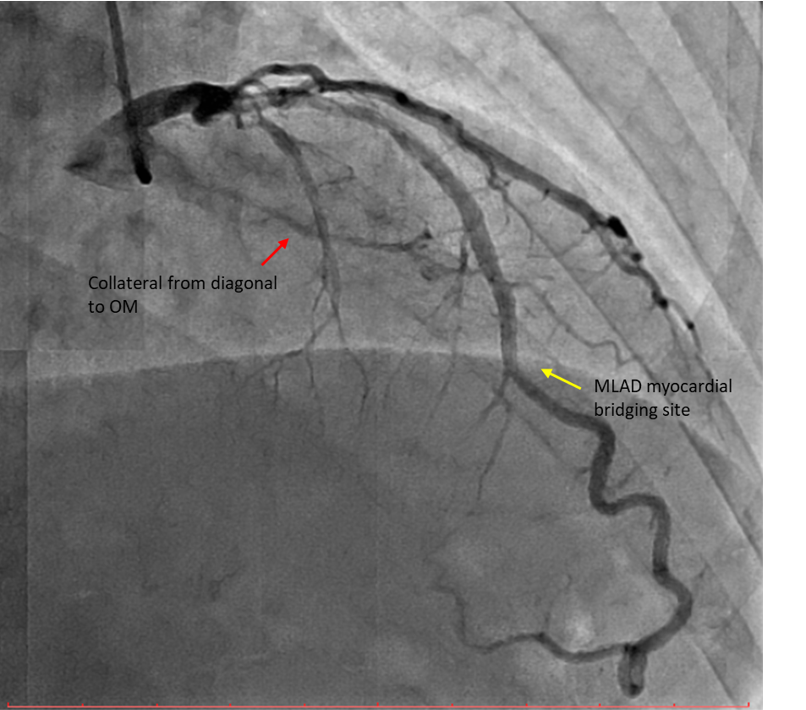
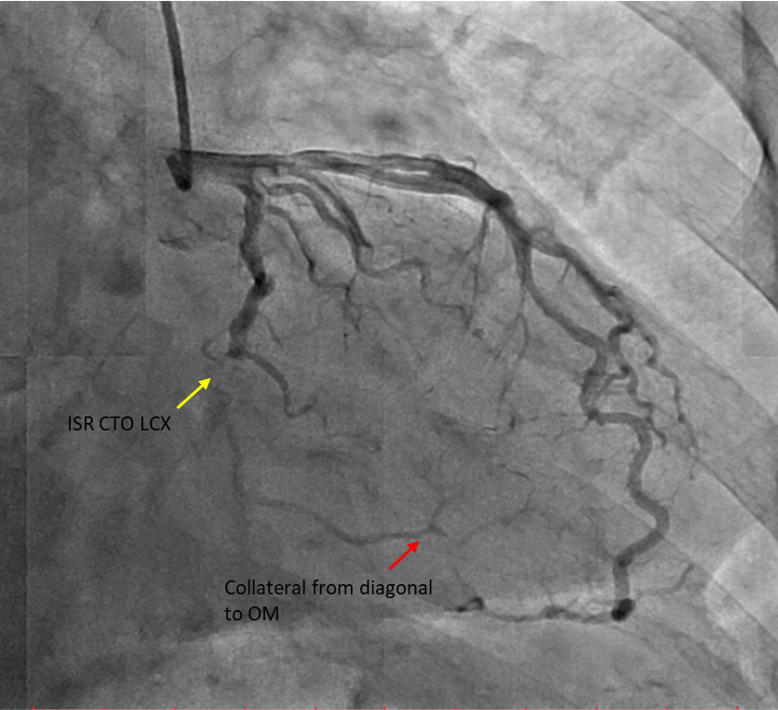
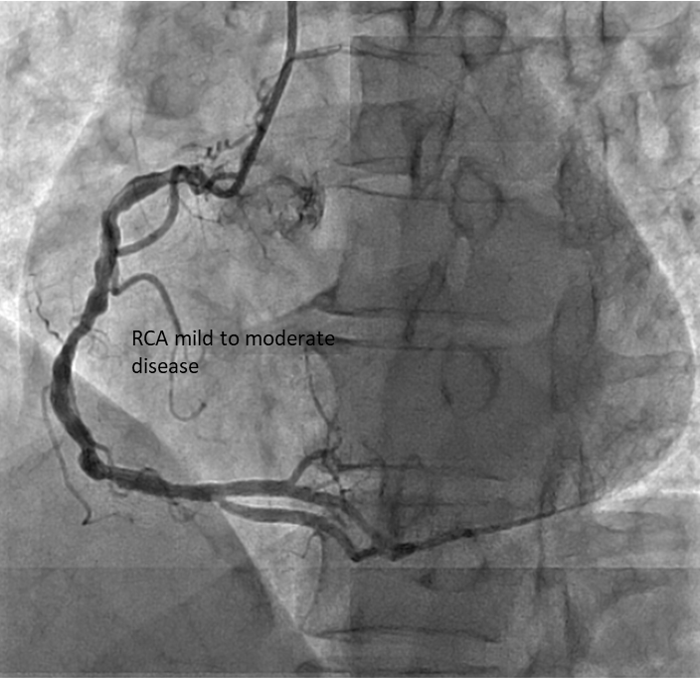
Diagnostic CAG:Left main stem: normalLeft anterior descending artery: proximal 30% stenosis, mid myocardial bridging, diagonal branch giving collateral to OM branchLeft circumflex artery: stent in distal LCX with ISR type IV 100% occlusionRight coronary artery: Dominant, mid 40-50% stenosis, PLV branch giving collateral to OM branch
Interventional Management
Procedural Step
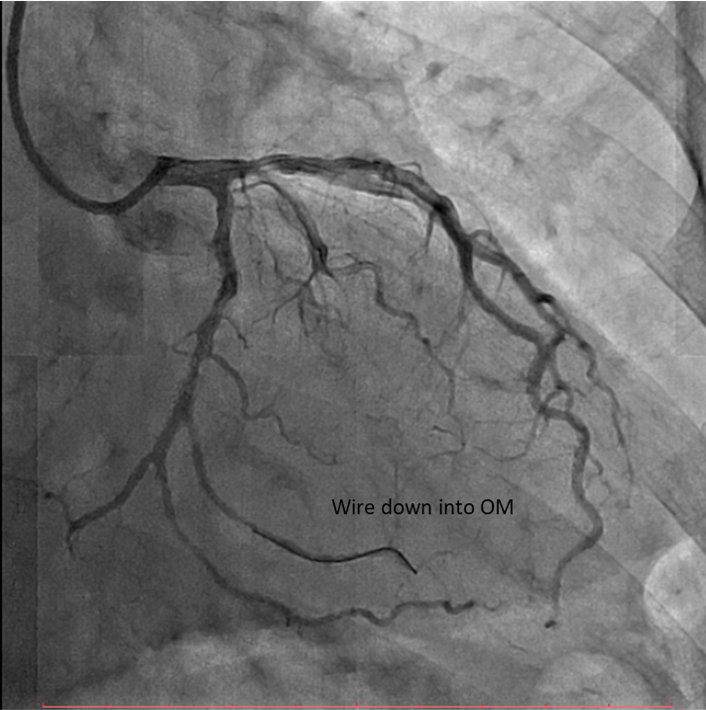
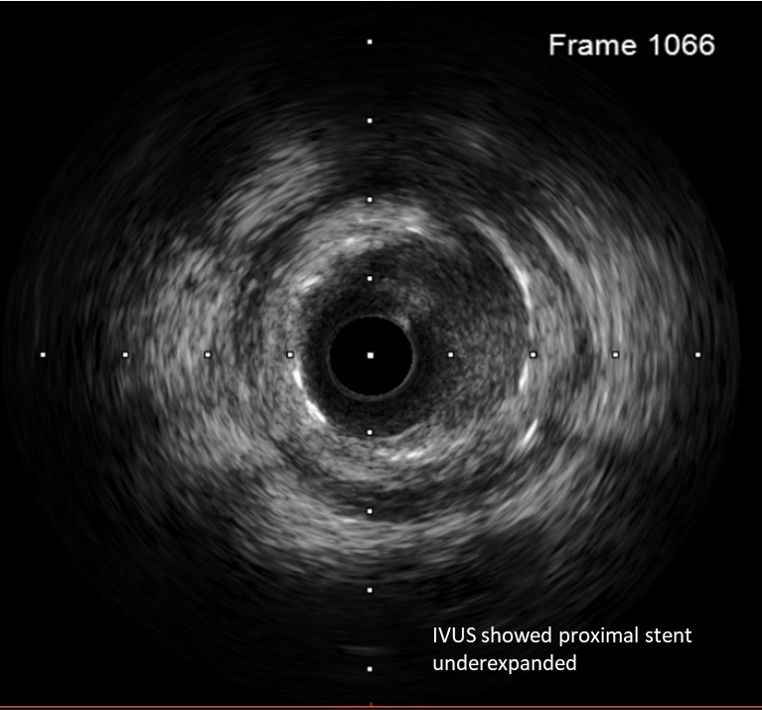
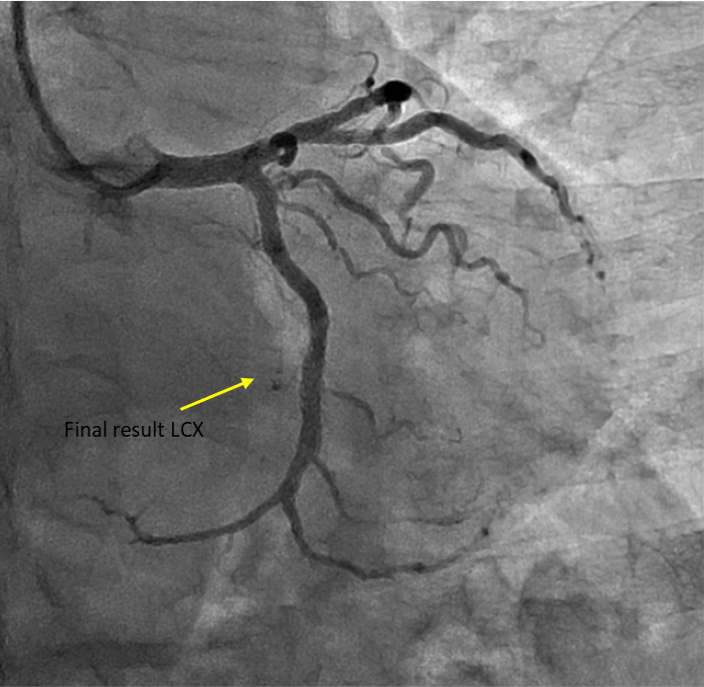
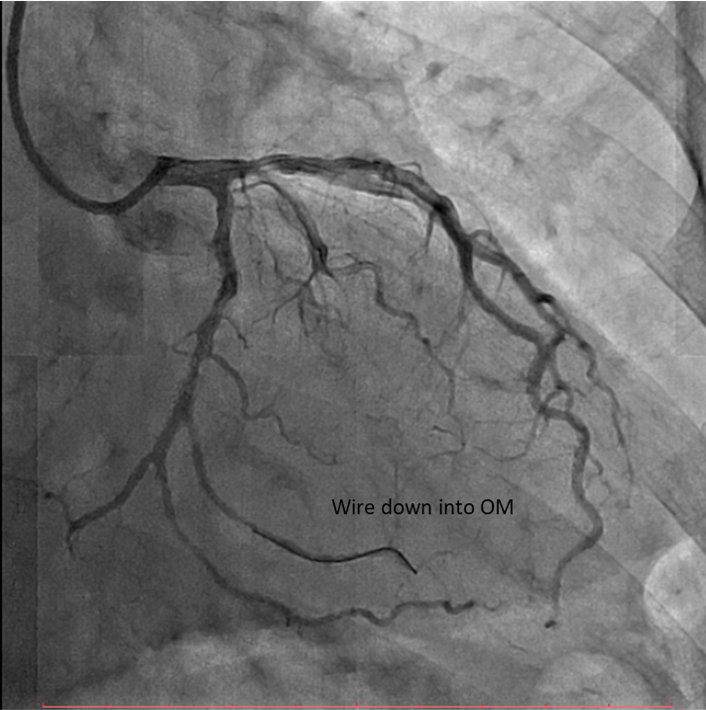
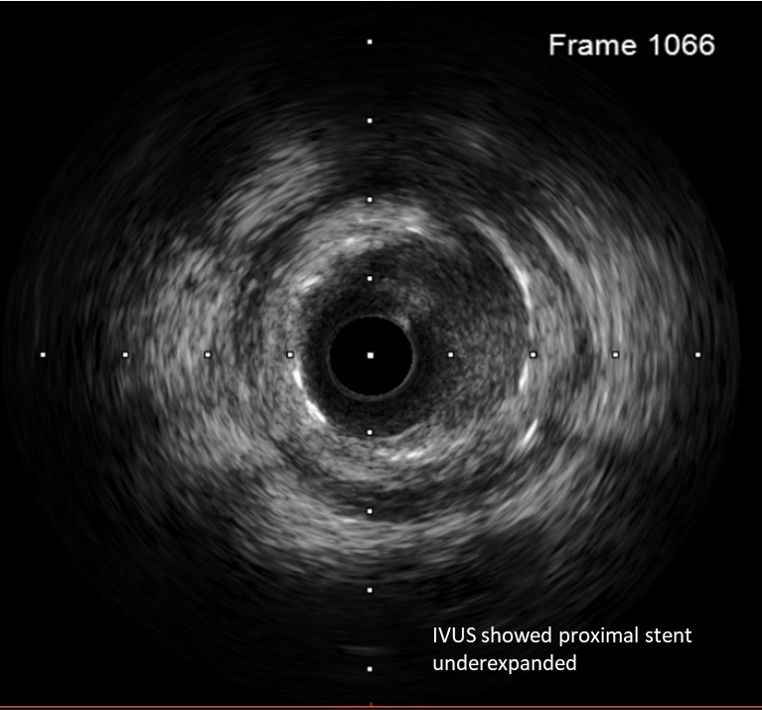
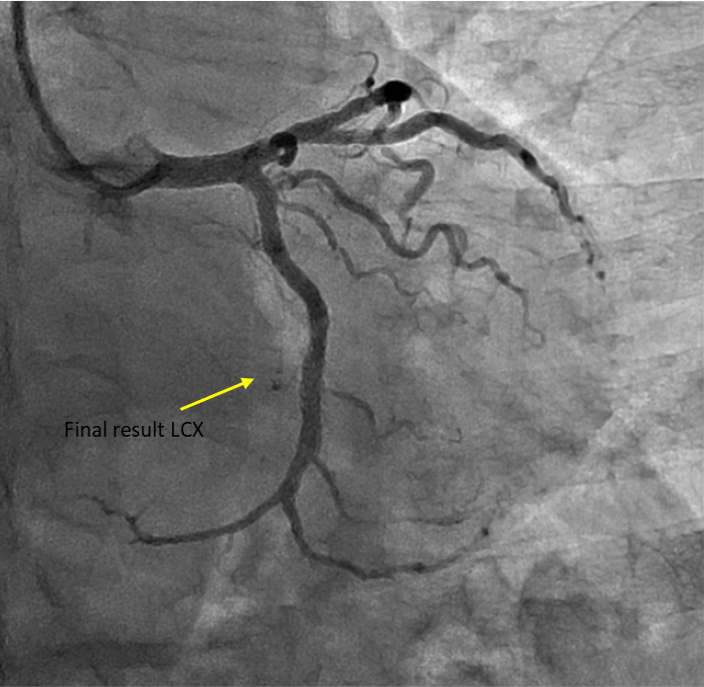
Percutaneous coronary intervention (PCI) was performed via transradial approach with 6 Fr radial sheath. Left coronary system was engaged using EBU 3.0 6 Fr guiding catheter. We decided for antegrade approach. Initial attempt with Fielder XT-A wire with a microcatheter support failed to cross the in-stent restenosis (ISR) lesion. We escalated to Asahi Gaia Second wire and successfully crossed the lesion to OM branch. Subsequently, wire was exchanged to a workhorse wire Runthrough Floppy via microcatheter. Lesion site was first predilated with a semi-compliant balloon Pantera Pro 2.0x 15 mm. Then, IVUS was passed down which showed previous stent site undersized, vessel size distal LCX of 4.0 mm. We further predilated lesion site with scoring balloon Scoreflex Trio 3.5x15 mm, up to 22 atm. Lesion site was acceptably prepared, then Paclitaxel drug-coated balloon Prevail 4.0x25 mm was deployed at nominal 6 atm for 60 seconds. Repeated IVUS run showed good stent apposition with MSA of 9.5mm2 proximally and 6.6mm2 distally. Final fluoroscopic shot showed good result with TIMI 3 flow, no stent edge dissection. Patient was symptom-free after procedure and discharged the following day.
Case Summary
In-stent restenosis (ISR) remains the most common cause of stent failure after percutaneous coronary intervention (PCI). Factors affecting risk of ISR include stent factor and also intra- and extra-stent factors. Undersizing of stent is one of the factor contributing to ISR. This case demonstrates a late onset Type IV ISR in an unexpectedly large left circumflex artery which was not accurately sized by previous angiography estimation. The use of intracoronary imaging proves crucial in determining the etiology of ISR and aids in better management of in-stent restenosis.


