Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-019
Shock, Stone, & Spin: A Primary PCI Against the Odds
By Widi Nugraha Hadian, Cheng Fong Cheah, Asri Said, Tiong Kiam Ong
Presenter
Widi Nugraha Hadian
Authors
Widi Nugraha Hadian1, Cheng Fong Cheah2, Asri Said2, Tiong Kiam Ong2
Affiliation
Al Islam Hospital Bandung, Indonesia1, Sarawak Heart Centre, Malaysia2,
View Study Report
TCTAP C-019
Coronary - ACS/AMI
Shock, Stone, & Spin: A Primary PCI Against the Odds
Widi Nugraha Hadian1, Cheng Fong Cheah2, Asri Said2, Tiong Kiam Ong2
Al Islam Hospital Bandung, Indonesia1, Sarawak Heart Centre, Malaysia2,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 52-year-old female with a history of diabetes and hypertension presented to our center from a district hospital with typical chest pain and shortness of breath. She was found to be in respiratory failure and cardiogenic shock, requiring intubation. Hemodynamic stability was achieved with intravenous inotropic and vasopressor support.
Relevant Test Results Prior to Catheterization
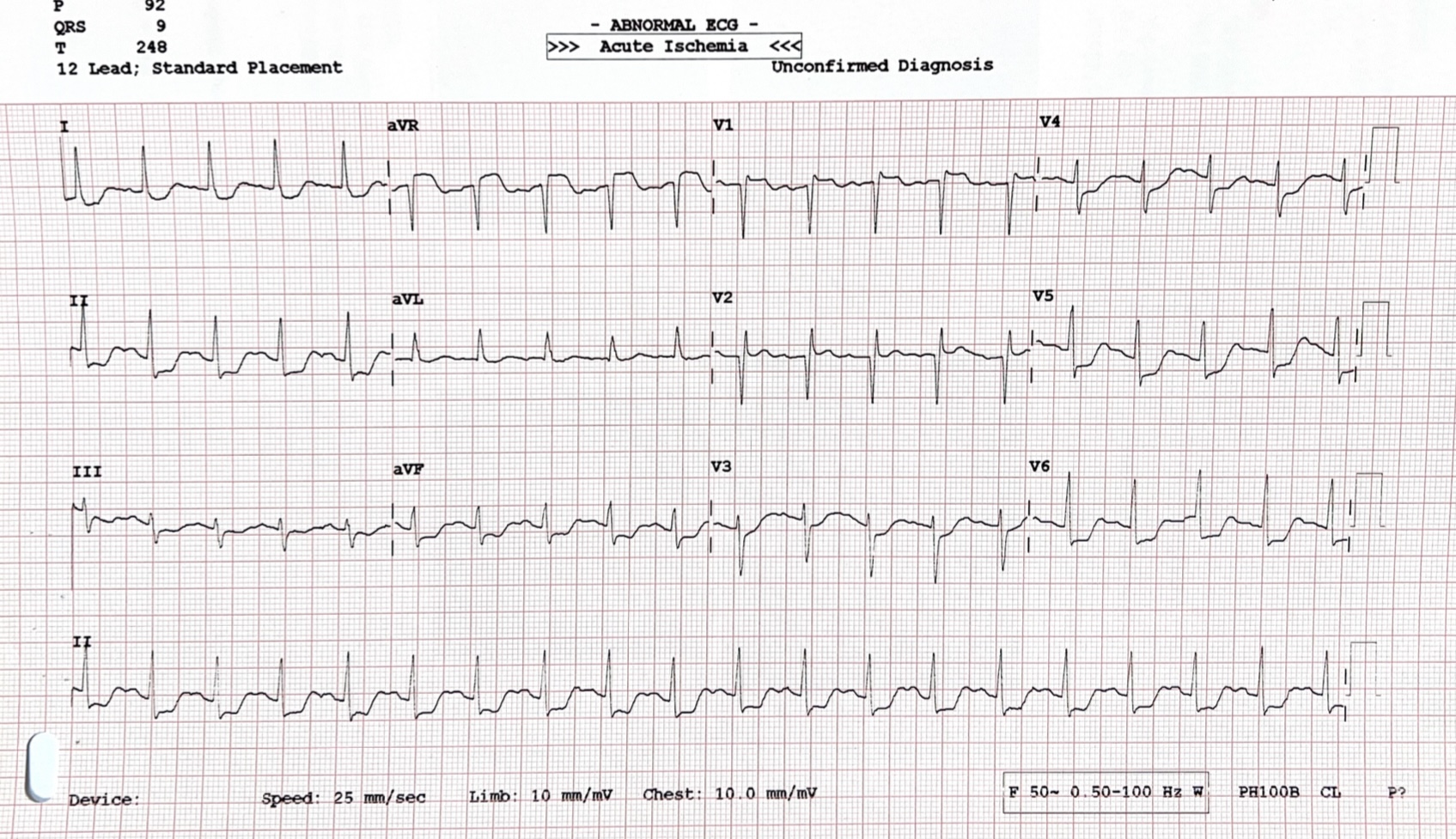
The ECG showed ST elevation in aVR with reciprocal ST depression in leads V4-V6, II, and aVF.
Relevant Catheterization Findings
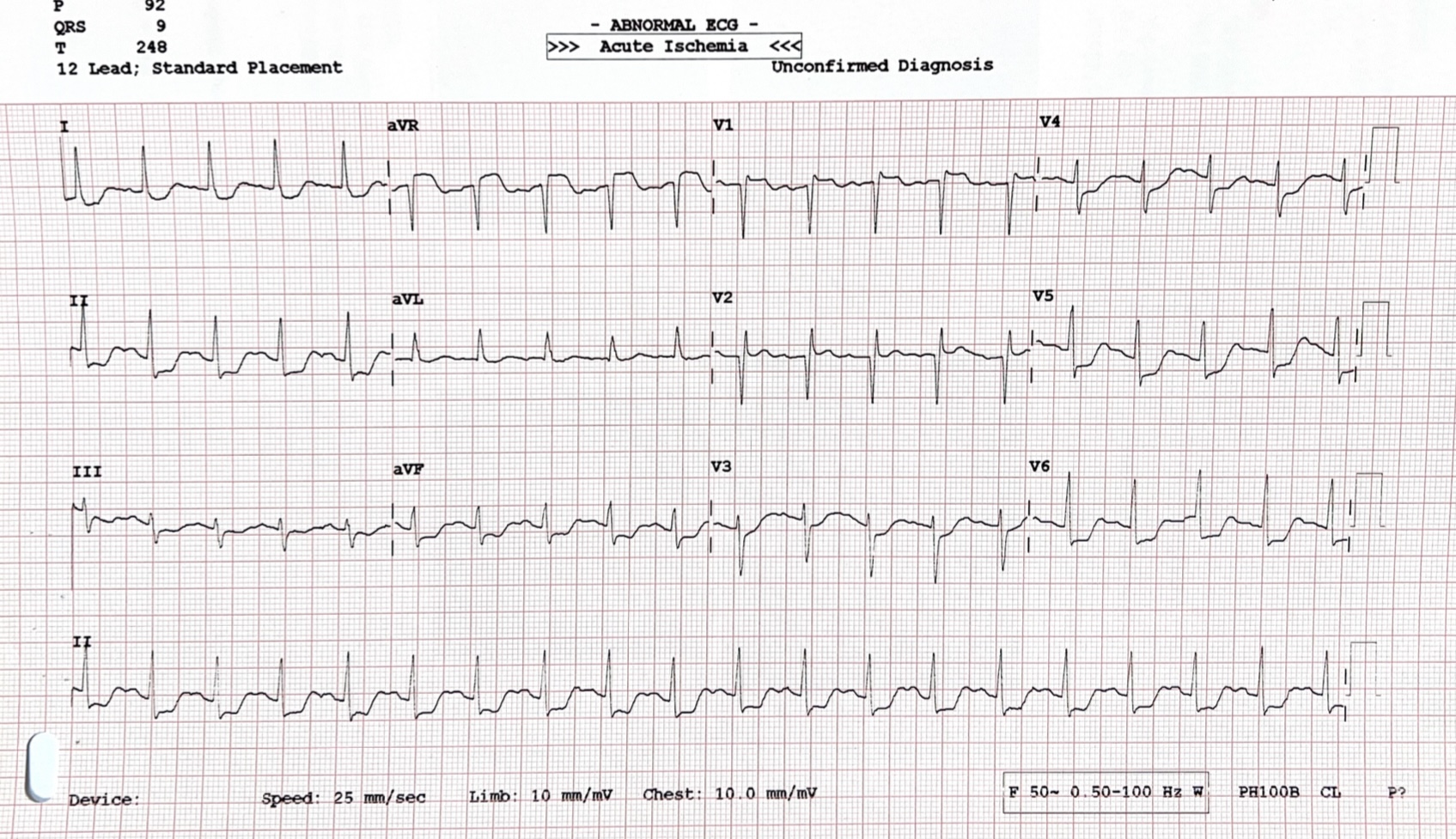
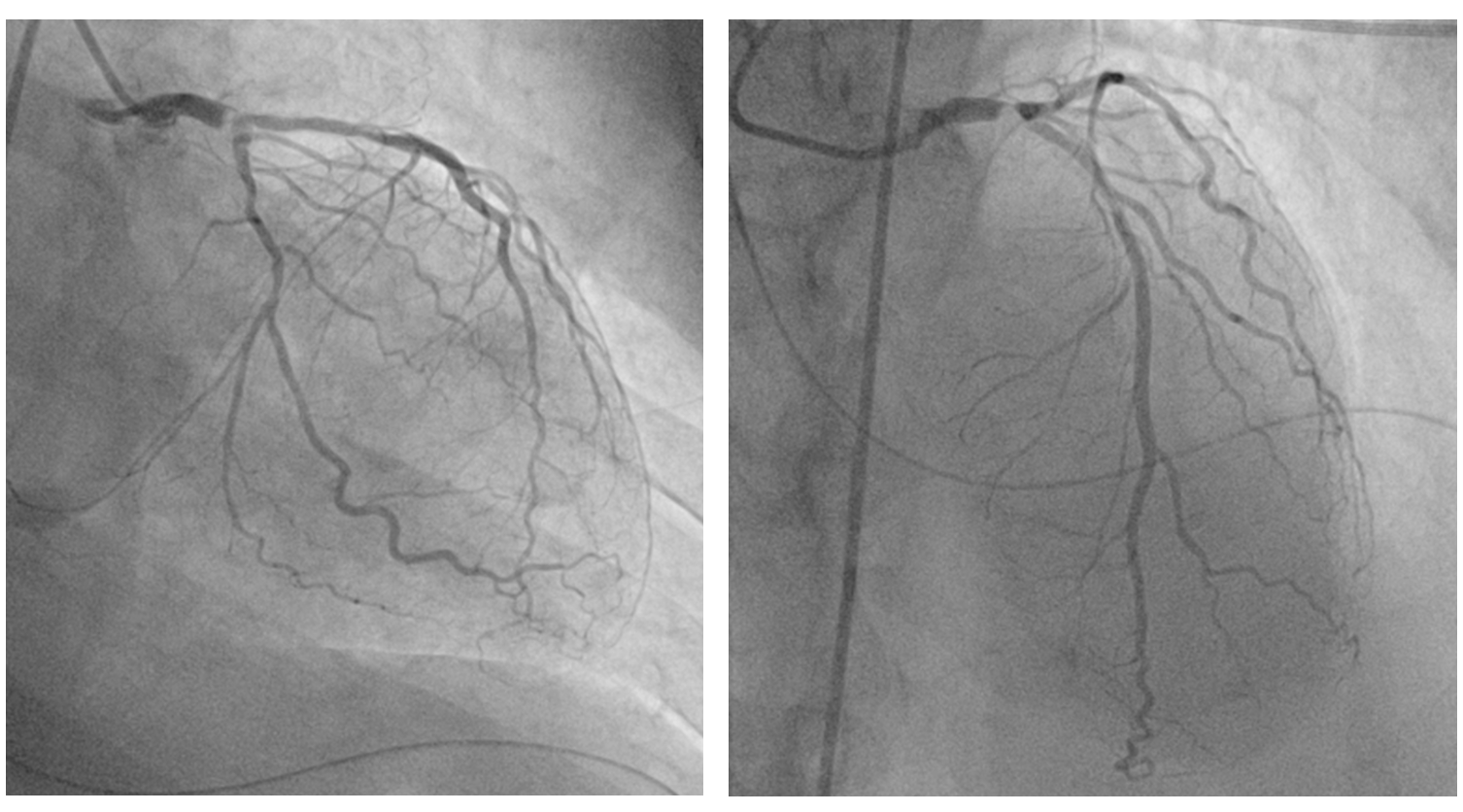
Due to a weak radial pulse, right femoral artery access was obtained for coronary angiography. A 6 French sheath was inserted. Angiography revealed : 95% stenosis with calcification of the distal left main coronary artery (LMCA), 70-80% stenosis of the proximal - mid left anterior descending artery (LAD), 50%-60% stenosis of the proximal left circumflex artery (LCx) and normal right coronary artery (RCA).
Interventional Management
Procedural Step
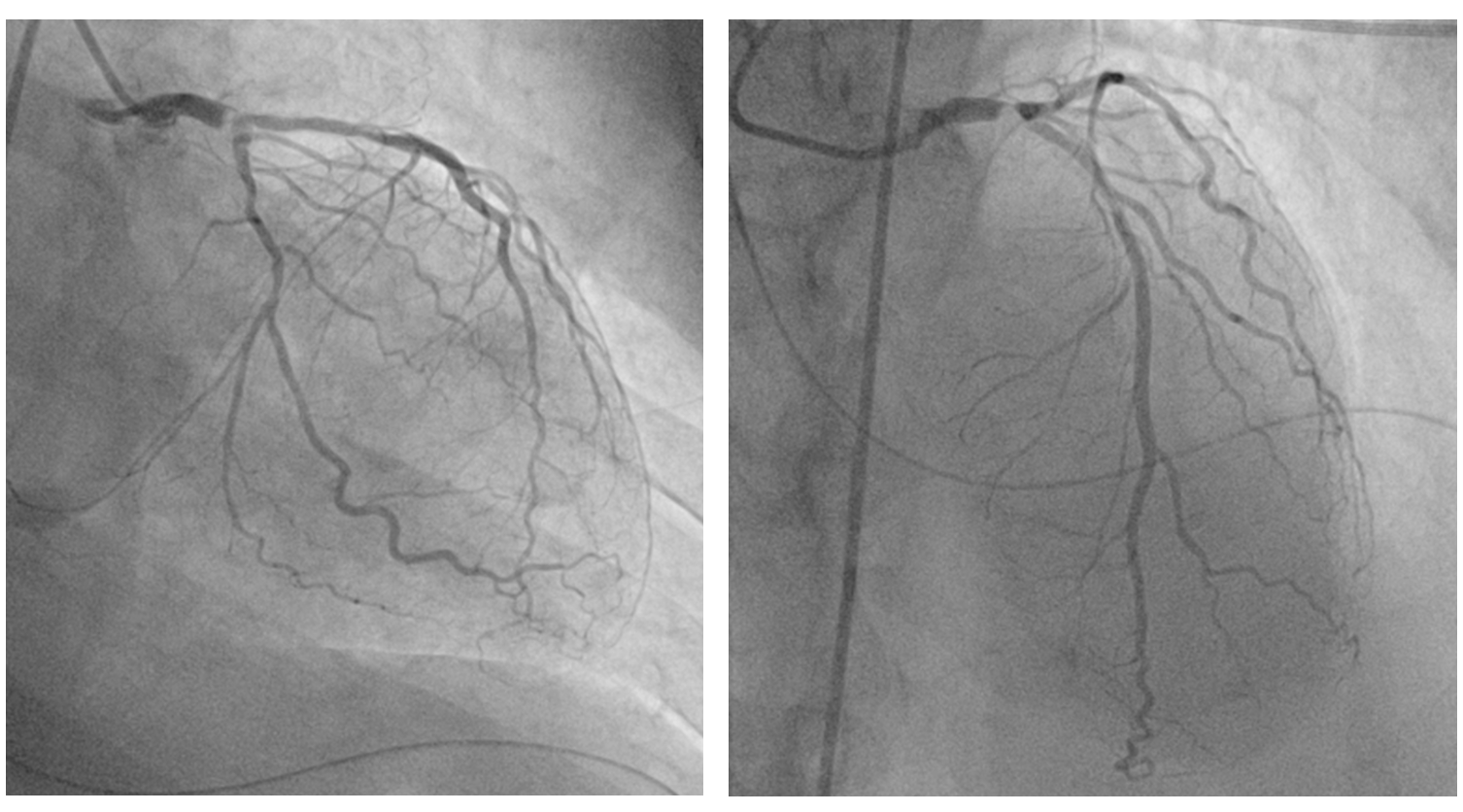
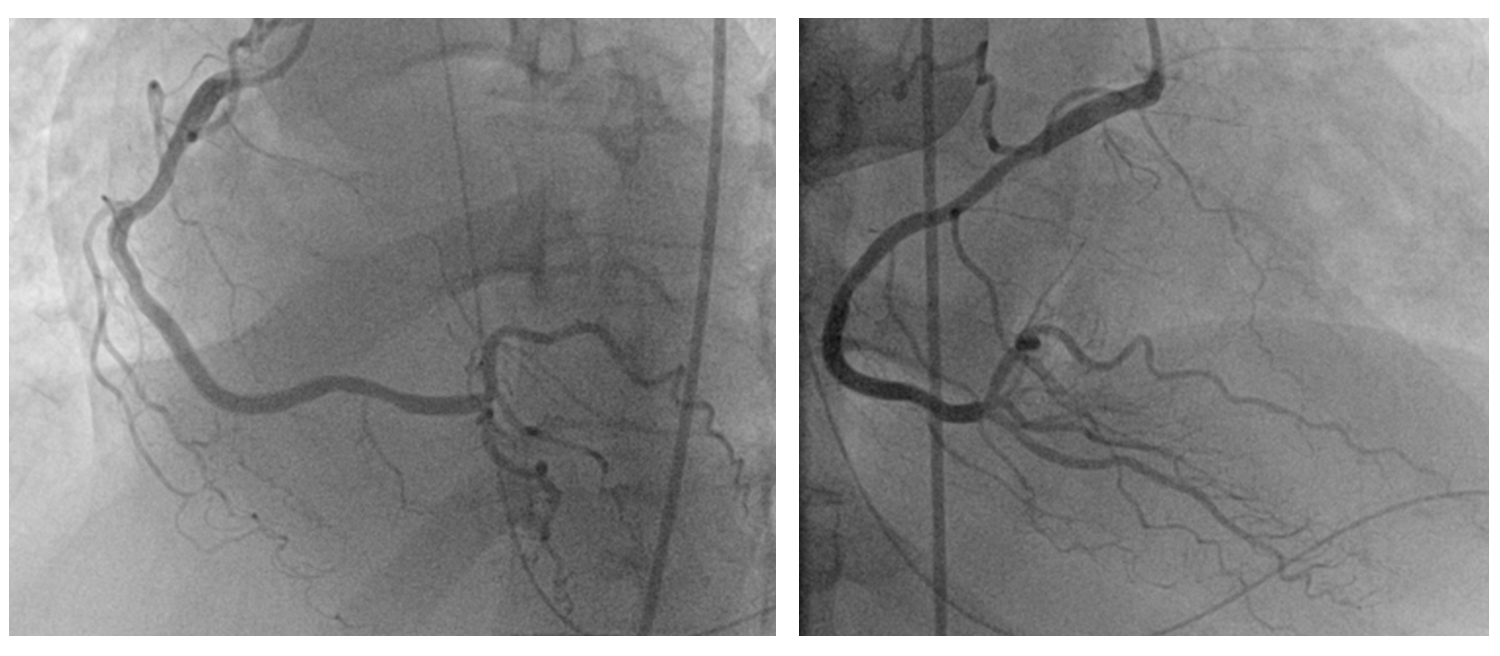
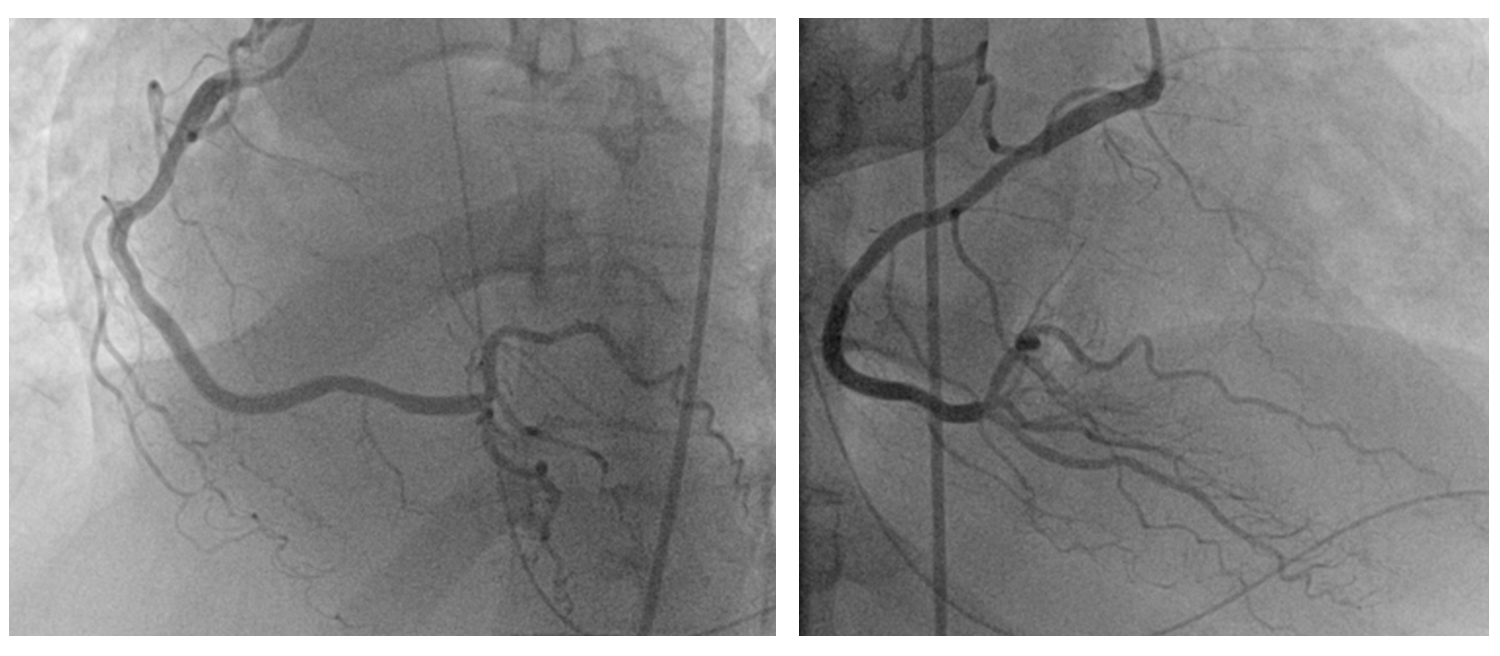
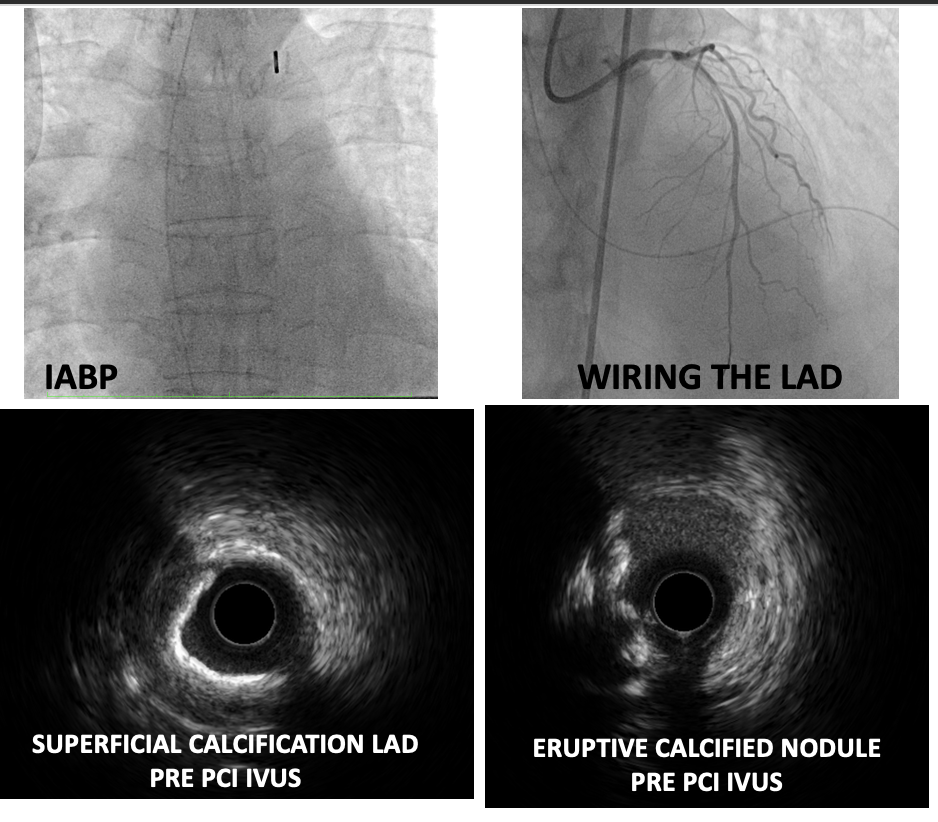
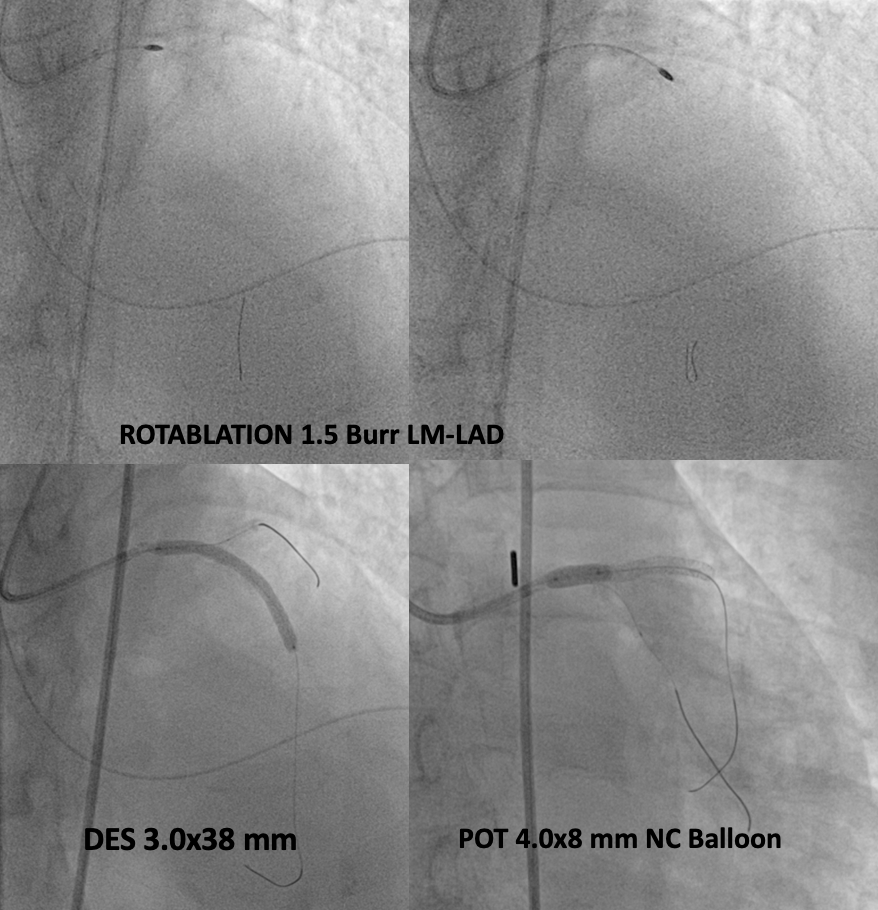
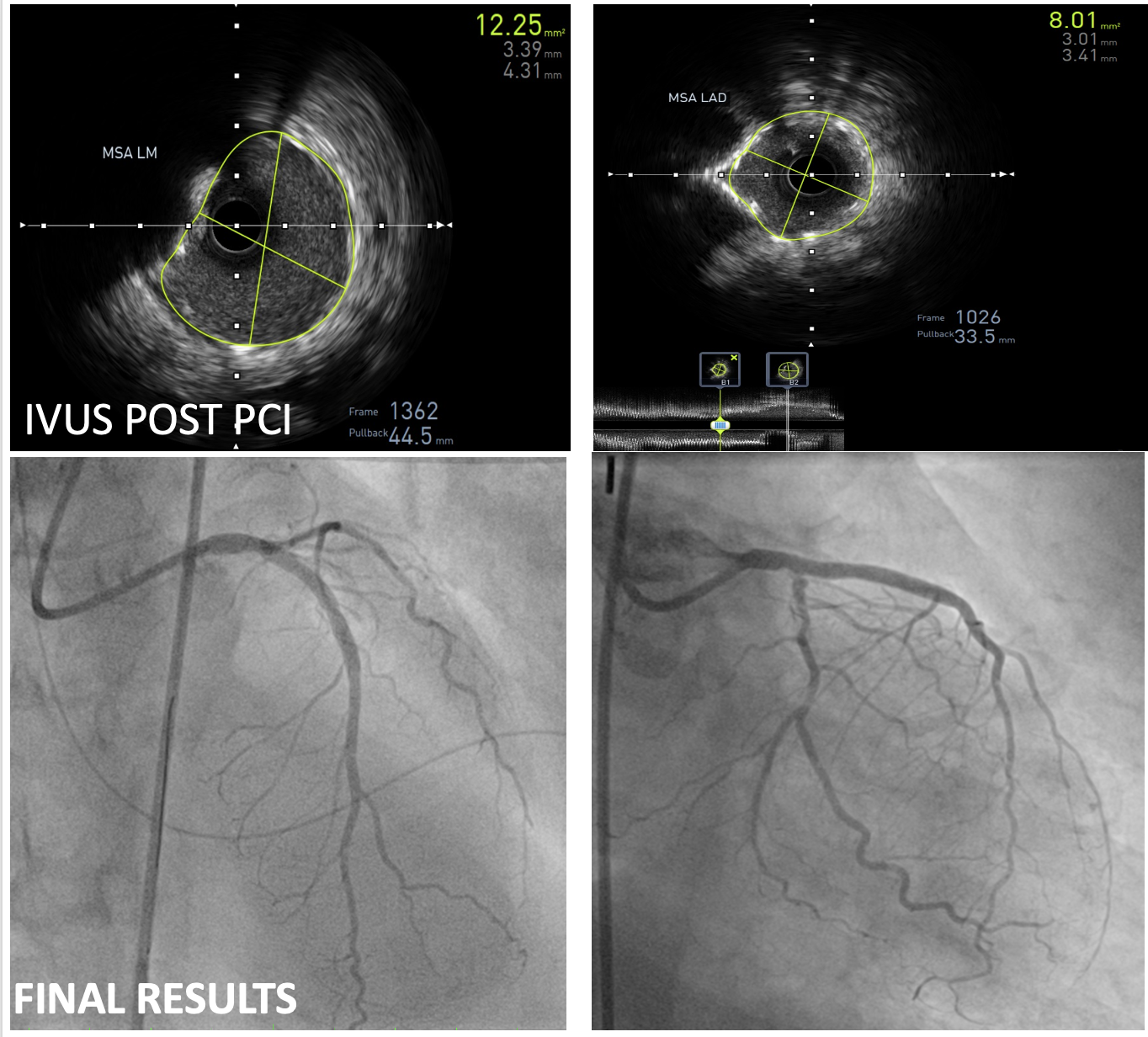
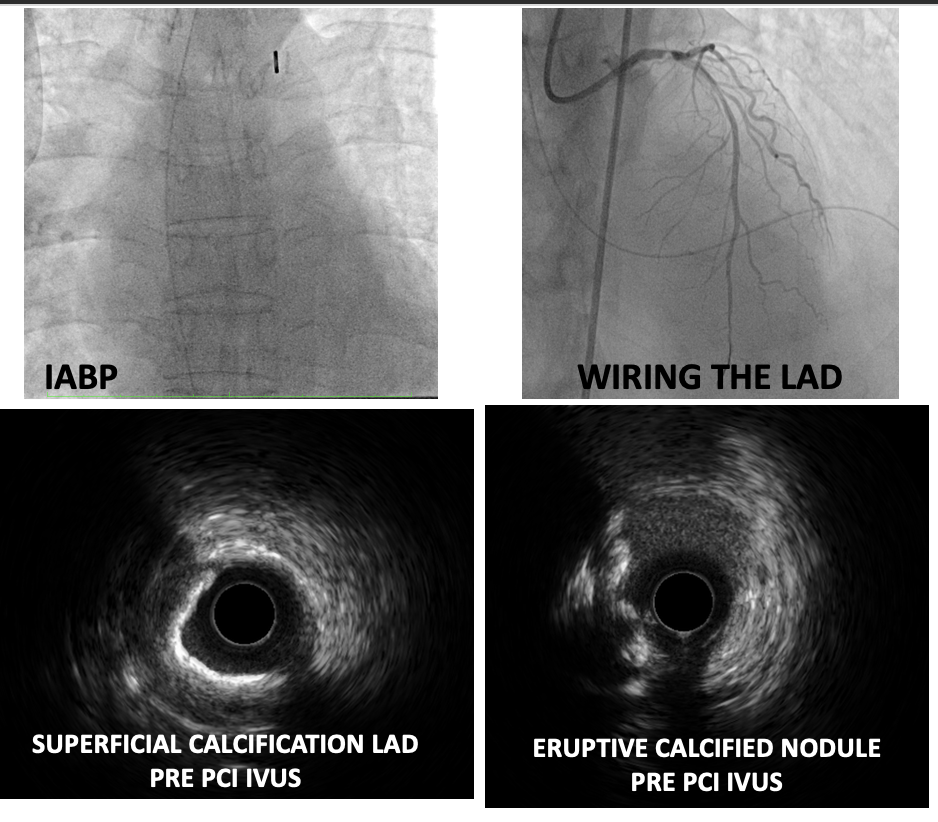
Percutaneous coronary intervention (PCI) of the LMCA-LAD lesion was performed with intra-aortic balloon pump (IABP) support. A 6 French EBU 3.5 guiding catheter was used to engage the left coronary artery. After wiring the lesion with a moderate support wire, intravascular ultrasound (IVUS) revealed an eruptive calcified nodule in the distal LMCA and heavy calcification (270-360 degrees) in the LAD. Rotablation was performed with a 1.5 mm burr for 3 runs. Following rotablation, the LAD wire was lost but successfully rewired. The LMCA-LAD lesion was predilated with a 3.0 x 15 mm non-compliant (NC) balloon. Provisional crossover stenting of the LMCA-LAD was performed with a 3.0 x 38 mm drug-eluting stent (DES). Proximal optimization was achieved with a 4.0 x 8 mm NC balloon inflated to 16 atmospheres (ATM) in the LMCA. The proximal-mid LAD was post-dilated with a 3.0 x 15 mm NC balloon inflated to 12 ATM. Repeat IVUS demonstrated good stent apposition and landing zones with no edge dissection, but the minimal stent area (MSA) in the proximal LAD required further optimization. Final post-dilation in proximal LAD with a 3.5 x 12 mm non-compliant (NC) balloon inflated to 16 ATM resulted in a good final angiographic result and IVUS-confirmed MSA of 8.01 mm2 in the LAD and 12.24 mm2 in the LMCA.
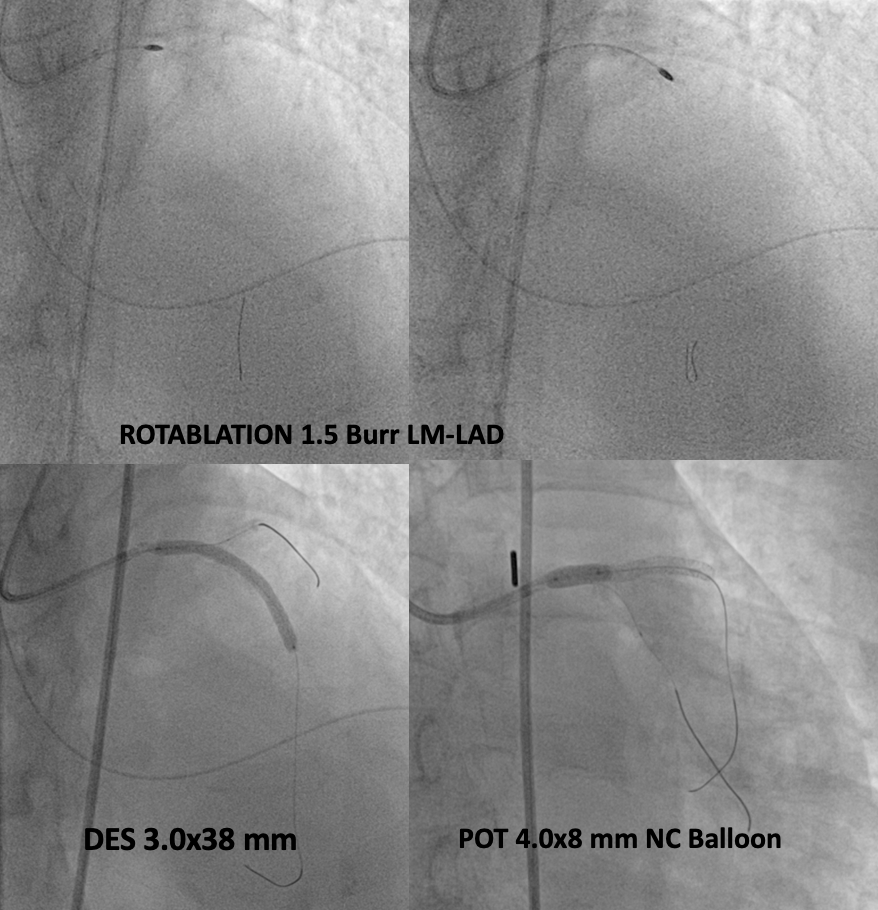
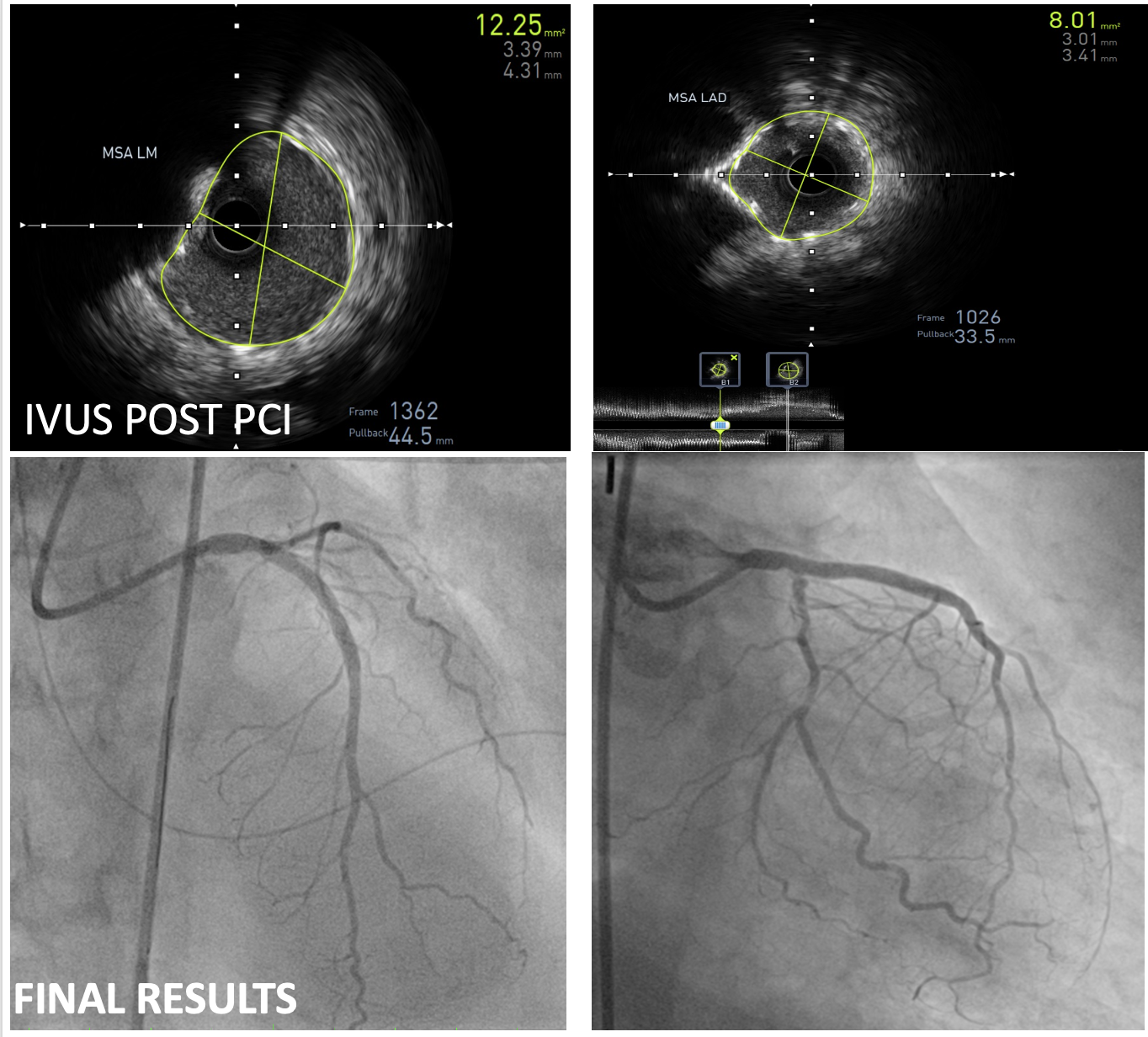
Case Summary
This case highlights successful IVUS-guided PCI with rotablation in a critically ill patient with late-onset STEMI and aVR ST-elevation. The culprit lesion was a complex, eruptive calcified nodule in the distal LMCA, for which now no established treatment strategy exists. Despite the challenges, optimal angiographic and IVUS results were achieved. This case demonstrates the feasibility and potential benefit of this approach in this complex high-risk subset of ACS patients.


