Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-237
Coarctation Stenting With PDA Device Closure in Patient With Severe Pulmonary Hypertension: Lesson Learnt From a Challenging Case
By Quy Le Nguyen Phu
Presenter
Quy Le Nguyen Phu
Authors
Quy Le Nguyen Phu1
Affiliation
University of Medicine and Pharmacy at Ho Chi Minh City, Vietnam1,
View Study Report
TCTAP C-237
Endovascular - Thoracic & Abdominal Aortic Interventions
Coarctation Stenting With PDA Device Closure in Patient With Severe Pulmonary Hypertension: Lesson Learnt From a Challenging Case
Quy Le Nguyen Phu1
University of Medicine and Pharmacy at Ho Chi Minh City, Vietnam1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 11-year-old girl presented with exertional dyspnea. She has a history of ventricular septal defect and patent ductus arteriosus, along with severe coarctation of the aorta, but the coarctation was not repaired, and she was lost to follow-up. One year ago, she received a coarctation stent and was prescribed diuretics, bosentan, and sildenafil. However, her most recent follow-up revealed an abnormal increase in blood pressure in her upper limbs
Relevant Test Results Prior to Catheterization
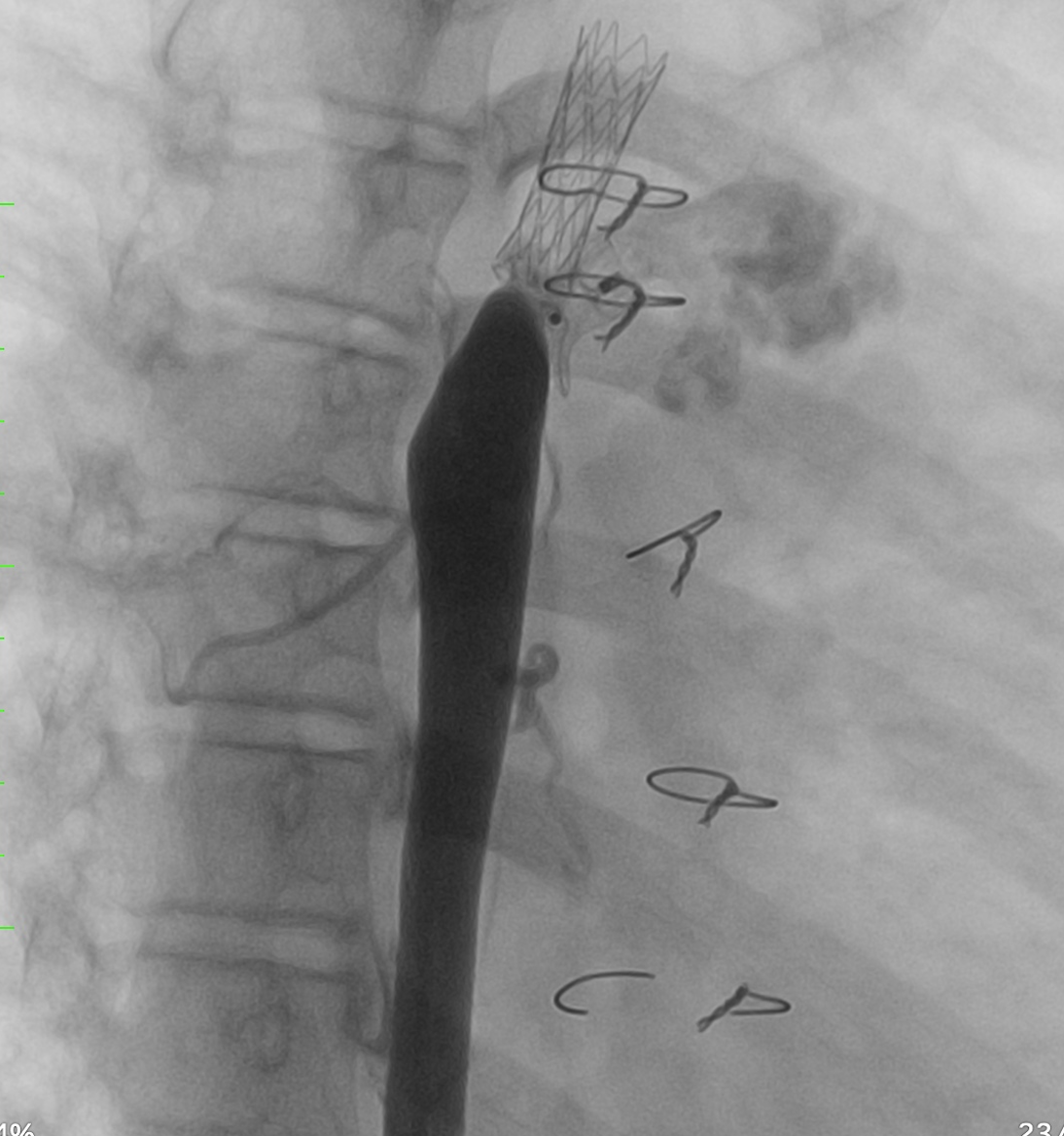
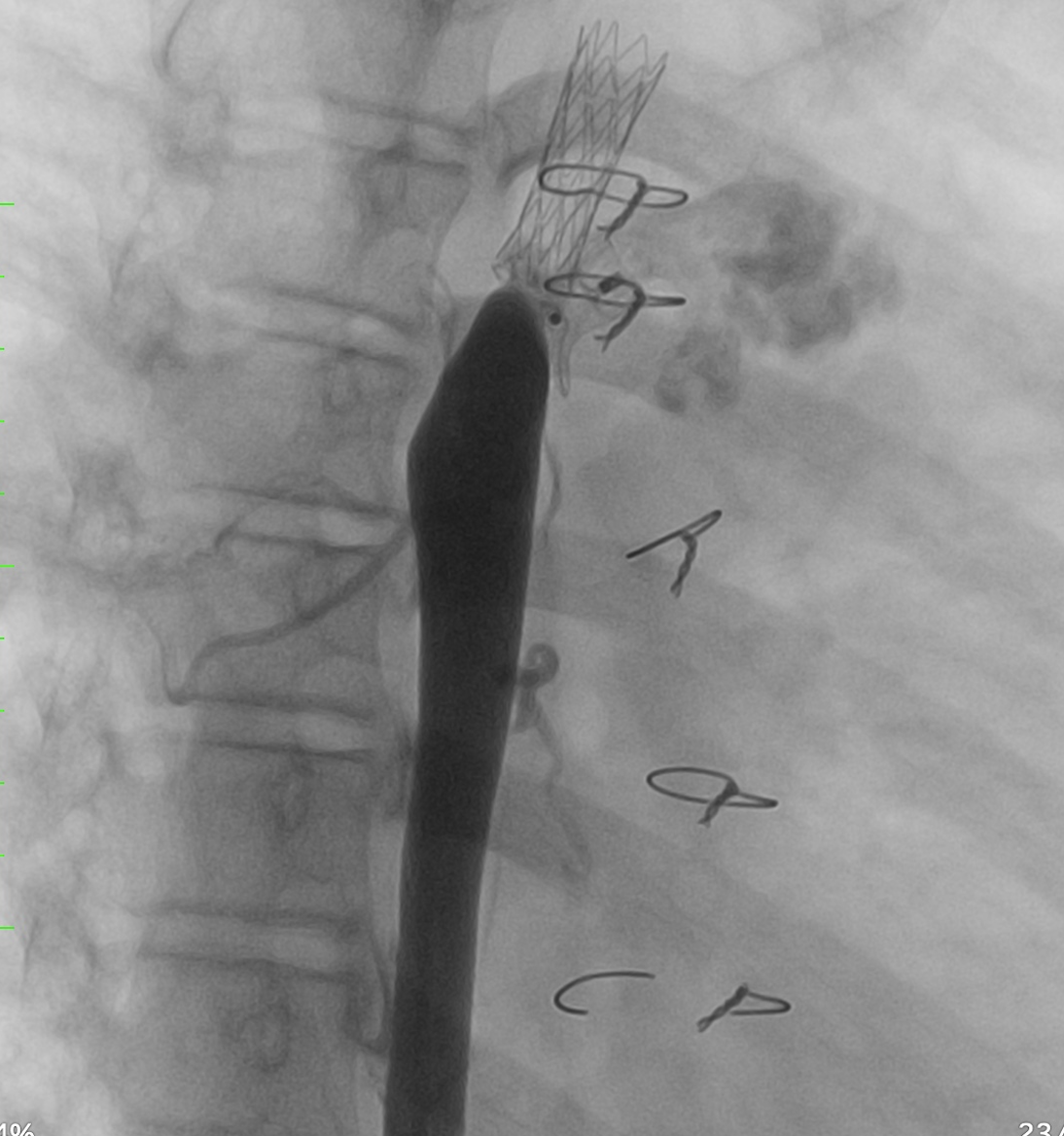
Echocardiography and CTA revealed severe stenosis in the distal part of the coarctation stent, caused by displacement of the PDA device. There was a residual shunt through the PDA measuring 3.5mm, with a slight left-to-right shunt. The narrowest diameter of the stent was 4mm. Additionally, a bidirectional shunt muscular outlet VSD with a diameter of 6mm was noted. The function of the left ventricle was preserved
Relevant Catheterization Findings
The aortography revealed severe stenosis in the distal part of the coarctation stent, caused by displacement of the PDA device, which had shifted toward the descending aorta. There was a residual shunt through the PDA with a slight left-to-right shunt. The diameters of the ascending aorta, aortic arch, and descending aorta were 22mm, 9mm, and 13mm, respectively. The narrowest diameter of the stent was 4mm.
Interventional Management
Procedural Step
Firstly, an angiography was performed to confirm the positions of the CoA stent and PDA device. A 0.014” microwire (Transcend, Boston Scientific) was used to cross through the PDA device to reach the upper part of the aorta. A 5F guiding catheter was advanced toward the proximal stent but was unsuccessful. To assist with advancing the 5F guiding catheter, we used a 3.0 mm and 5.0mm balloon to dilate the opening beside the PDA device. An angiography was then conducted to assess the relative positions of the CoA stent and PDA device. We decided to deploy an additional stent to cover the distal part of the previous stent to direct the PDA device towards the pulmonary artery. A 7F delivery system was advanced to the optimal position, and a 21L AndraStent was successfully deployed. A 8.0mm high-pressure balloon (VACS III) was then used to further dilate the stent. The pressures in the ascending and descending aorta (below the stent) were recorded as 115mmHg and 90mmHg, respectively. Finally, an angiography confirmed the correct positioning of both the stent and the PDA device without complications.

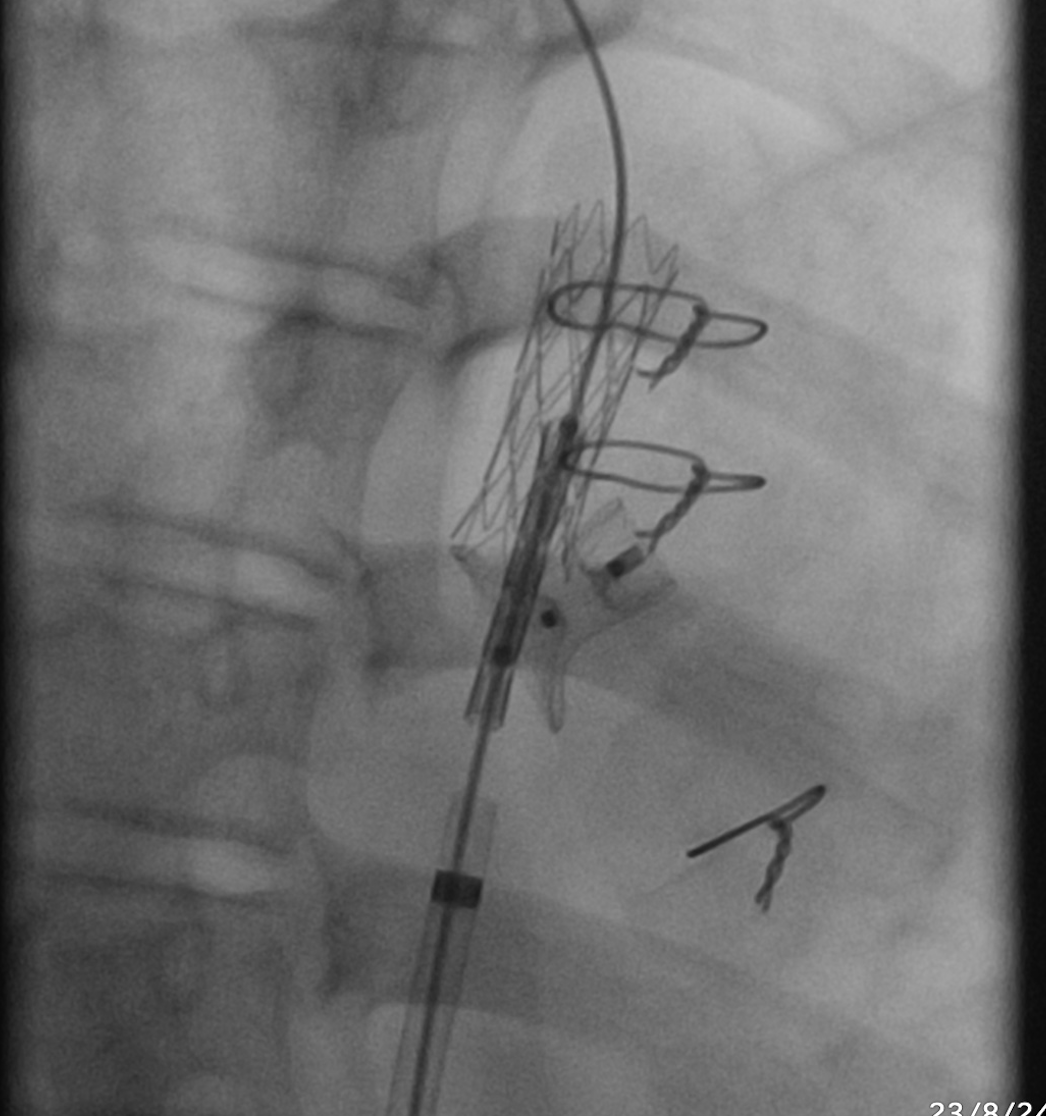


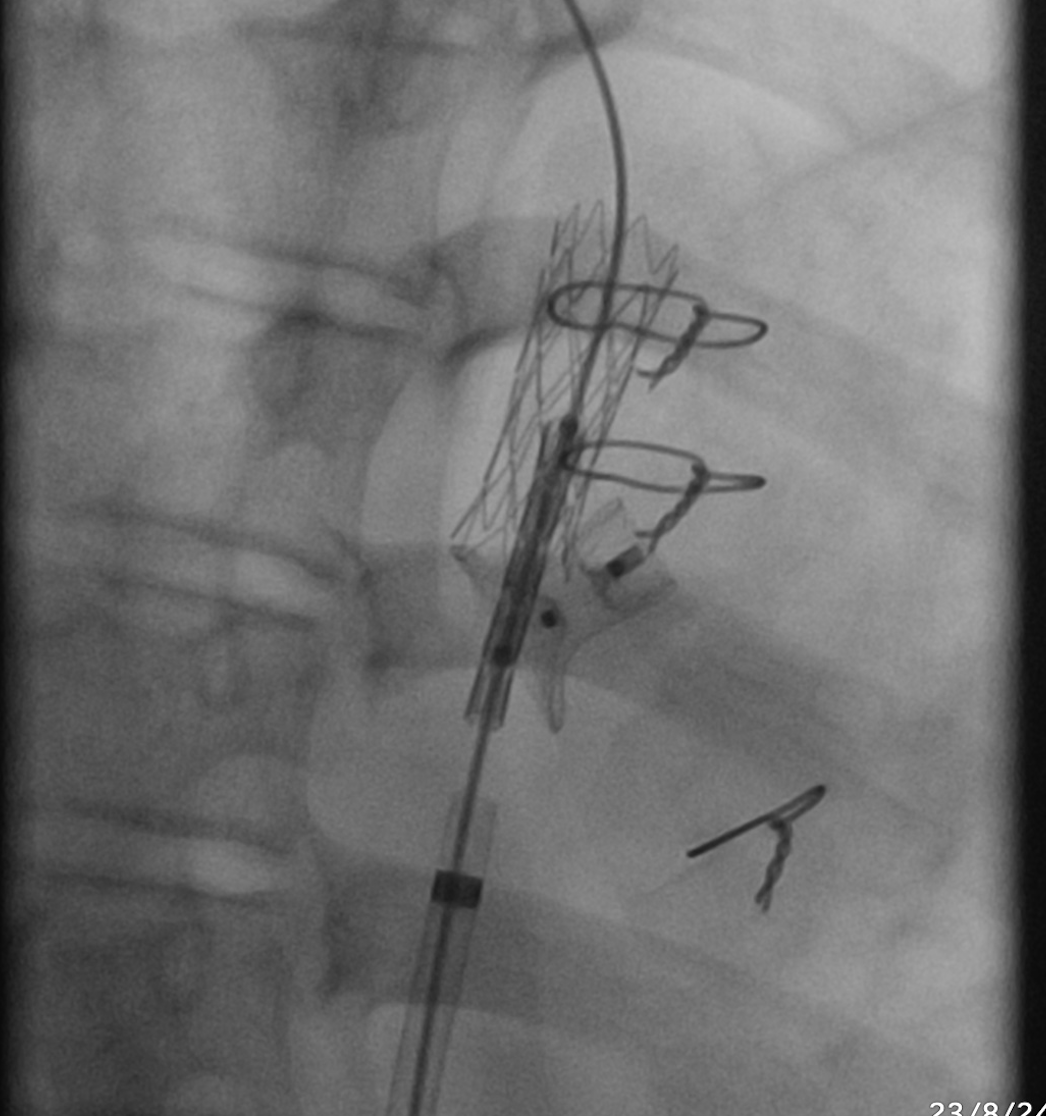

Case Summary
Coarctation stenting with PDA device closure in patients with severe pulmonary hypertension can be challenging due to potential complications during or after the procedure. The stent should be long enough to adequately cover the aorta below the PDA ampulla. Additionally, use of a high-pressure balloon may be necessary to achieve sufficient stent expansion and fixation, which can help compress the PDA device towards the pulmonary artery.


