Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-110
Look Beyond What You See: Successful Oct Guided PCI of Lad Instent Restenosis
By Harish Oruganti
Presenter
Harish Oruganti
Authors
Harish Oruganti1
Affiliation
KIMS Hospital, India1,
View Study Report
TCTAP C-110
Coronary - Complex PCI - In-Stent Restenosis
Look Beyond What You See: Successful Oct Guided PCI of Lad Instent Restenosis
Harish Oruganti1
KIMS Hospital, India1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 52 year old male diabetic with presented to our hospital with typical chest pain since 2 weeks. Vitals: Heart rate was 90 per minute, BP 140/90 mmHg. He underwent PCI to LAD with 2.75 x 20 mm DES in 2018 at outside hospital, compliant on aspirin 75mg and rosuvastatin 20mg but continues to chew tobacco.
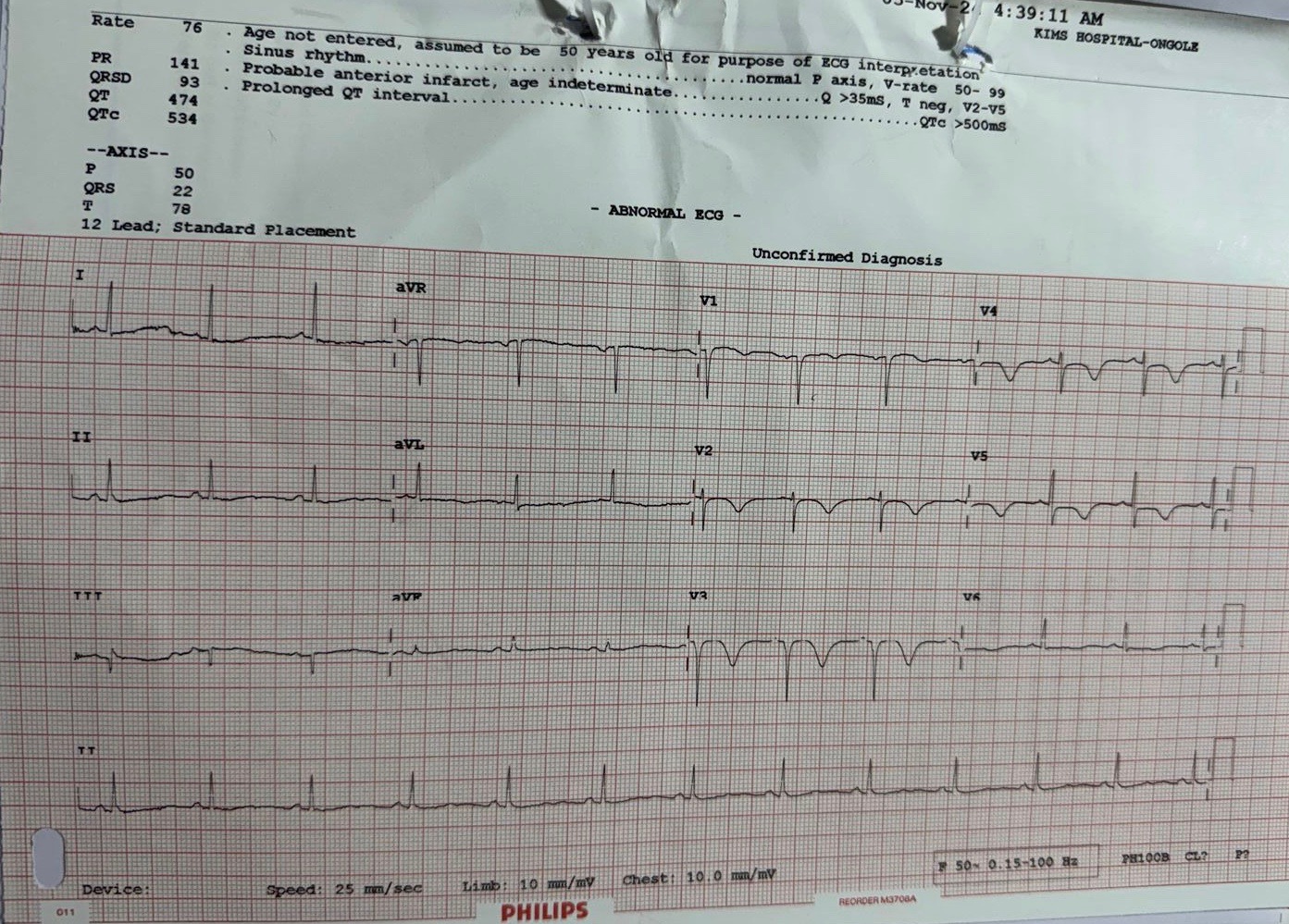
Relevant Test Results Prior to Catheterization
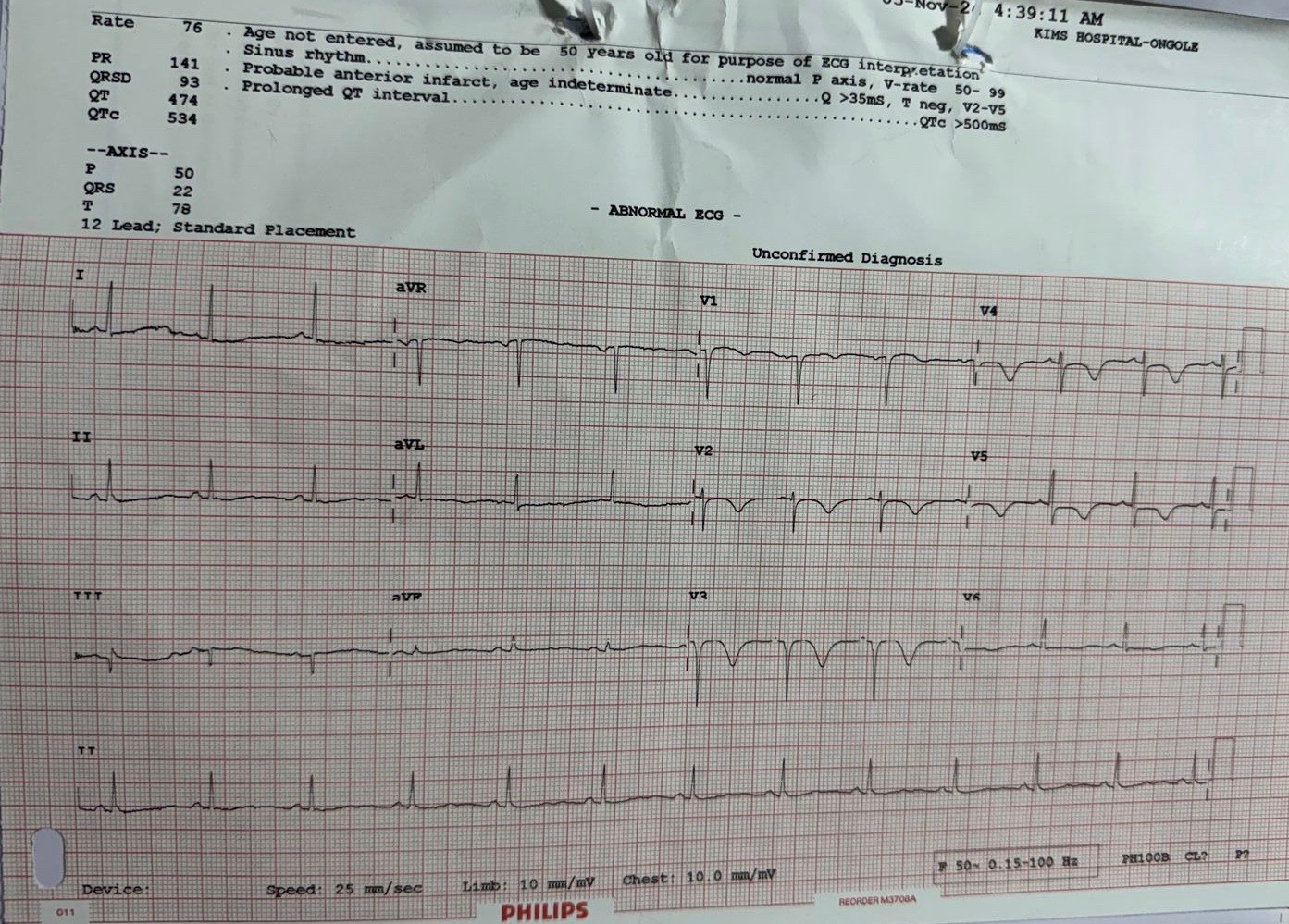
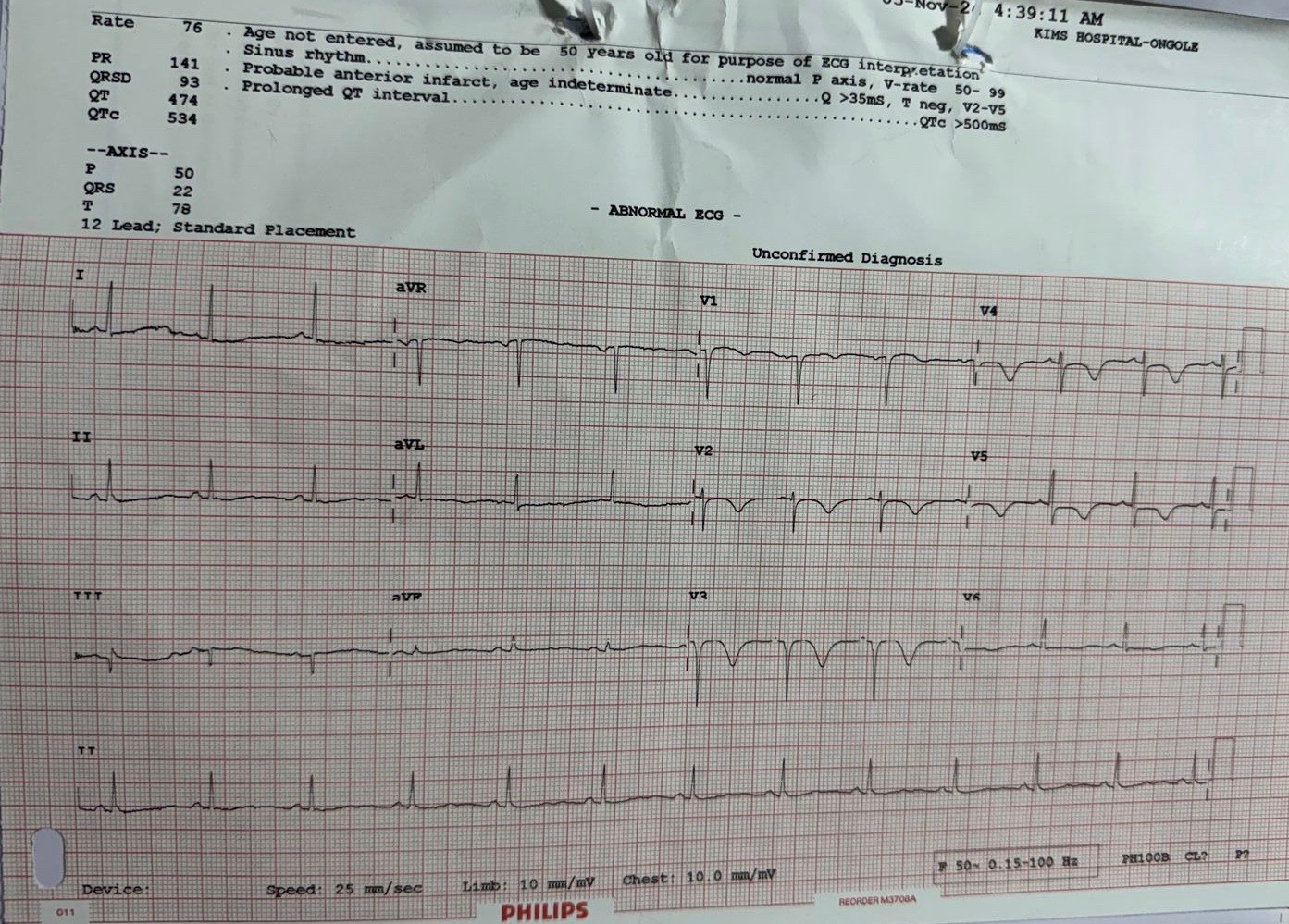
Troponin I was negative. ECG showed ST depressions in v1 to v4 leads with sinus rhythm. Echocardiography showed mild hypokinesia in anterior wall with mild LV dysfunction.
Relevant Catheterization Findings
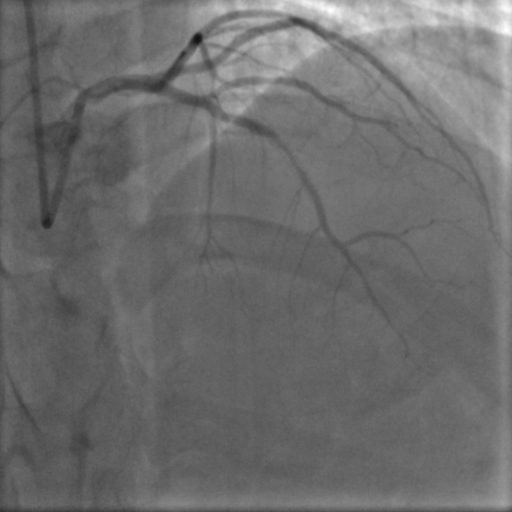
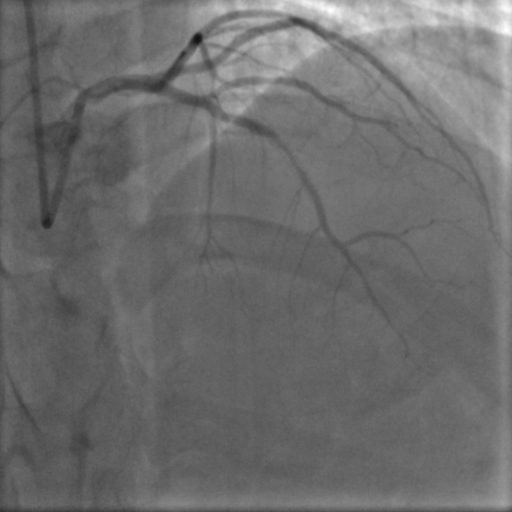
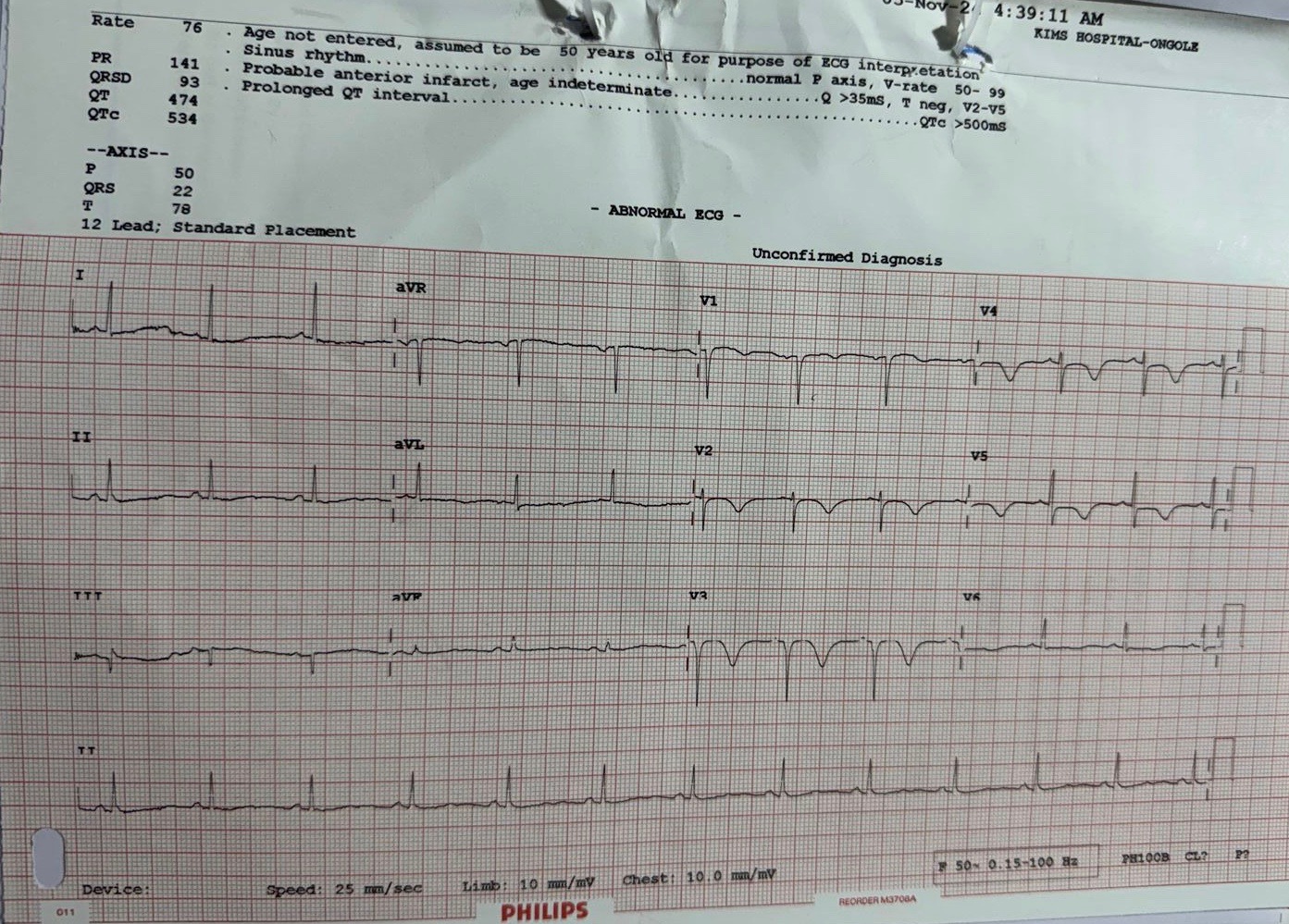
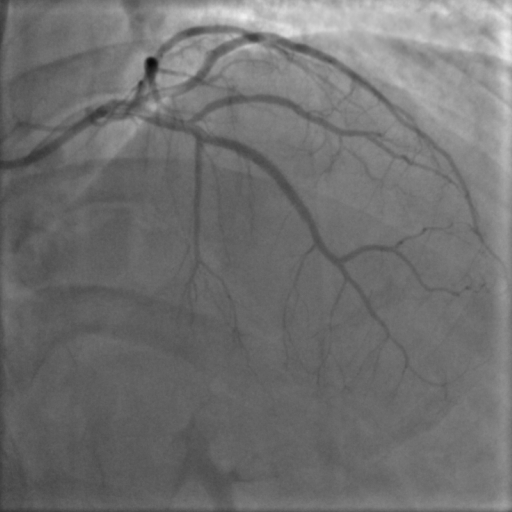
Coronary angiography was done through right radial access which demonstrated severe Instent restenosis (ISR) in the mid portion of LAD stent. LCX and RCA were normal.
Interventional Management
Procedural Step
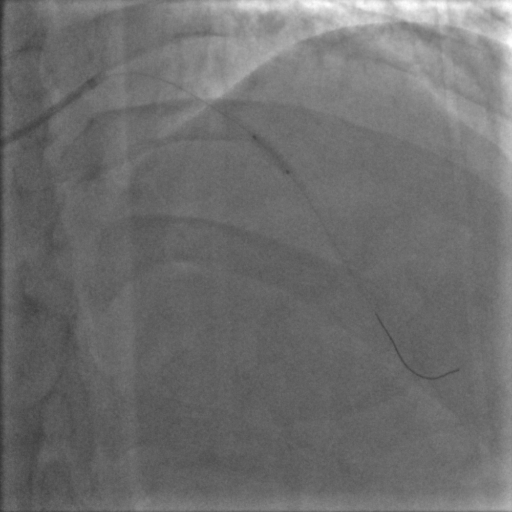
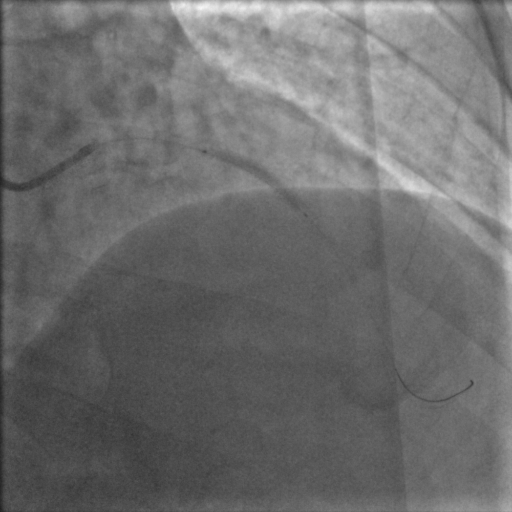
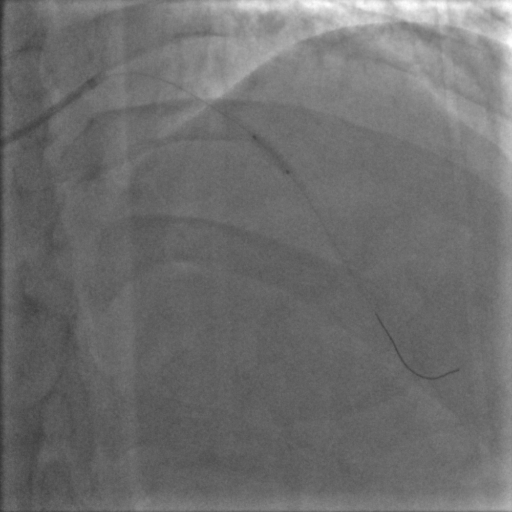
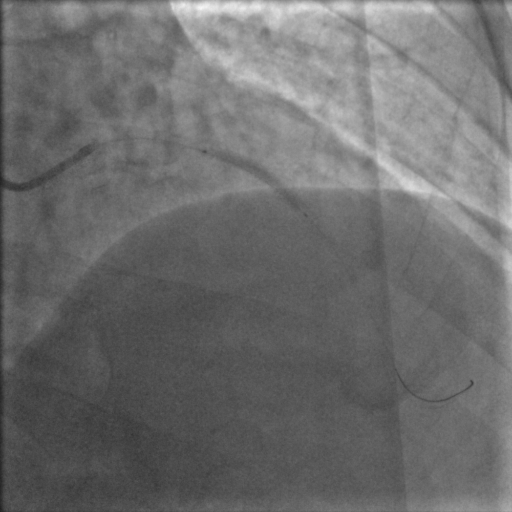
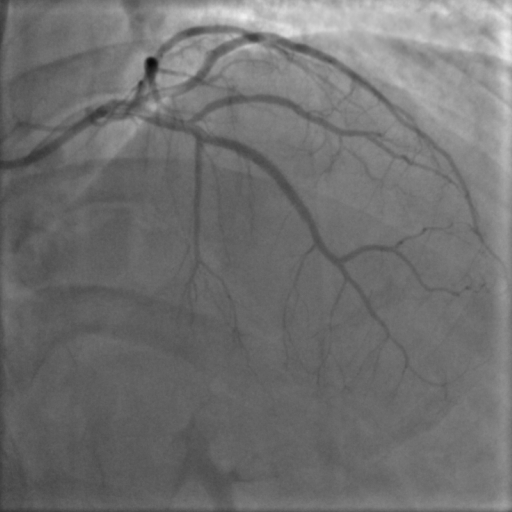
PCI was planned to LAD ISR lesion through right radial approach with 6 French sheath. Optical Coherence Tomography (OCT) was chosen for intracoronary imaging modality as it gives high resolution images to know the plaque morphology, exact mechanism of ISR which help in planning device selection and also to assess the adequacy of lesion preparation. 3.5 EBU 6 French Guiding catheter was taken with Runthrough (Terumo ,Japan) guidewire. Initial OCT ( Dragonfly OpStar catheter, Abbott,USA) run was done. Thick neointimal hyperplasia was seen with neoatheroma in mid portion of ISR lesion. mm as mean diameter in the distal reference segment was 2.9 mm (EEL to EEL) and the measured stent diameter was 2.6 mm. The MLA at the tightest point was 1.15 mm2 . Lesion length was 28 mm. We planned to do plaque modification with cutting balloon and correction of stent under expansion with non compliant balloon followed by drug coated balloon application.Initial plaque modification was done with wolverine (Boston Scientific,USA) 2.5 X 10 mm cutting balloon up to 12 atm from distal to proximal followed by 3.0 x12 mm NC Quantum Apex (Boston Scientific,USA) balloon inflation from 16 to 20 atm. Final OCT run was done which showed intimal micro tears with good lumen gain. 3x 30 mm Agent (Boston Scientific,USA) Drug-Coated Balloon was inflated within the lesion area at 6 atm nominal pressure for 90 seconds. TIMI 3 flow was seen with good vessel expansion on angiography.
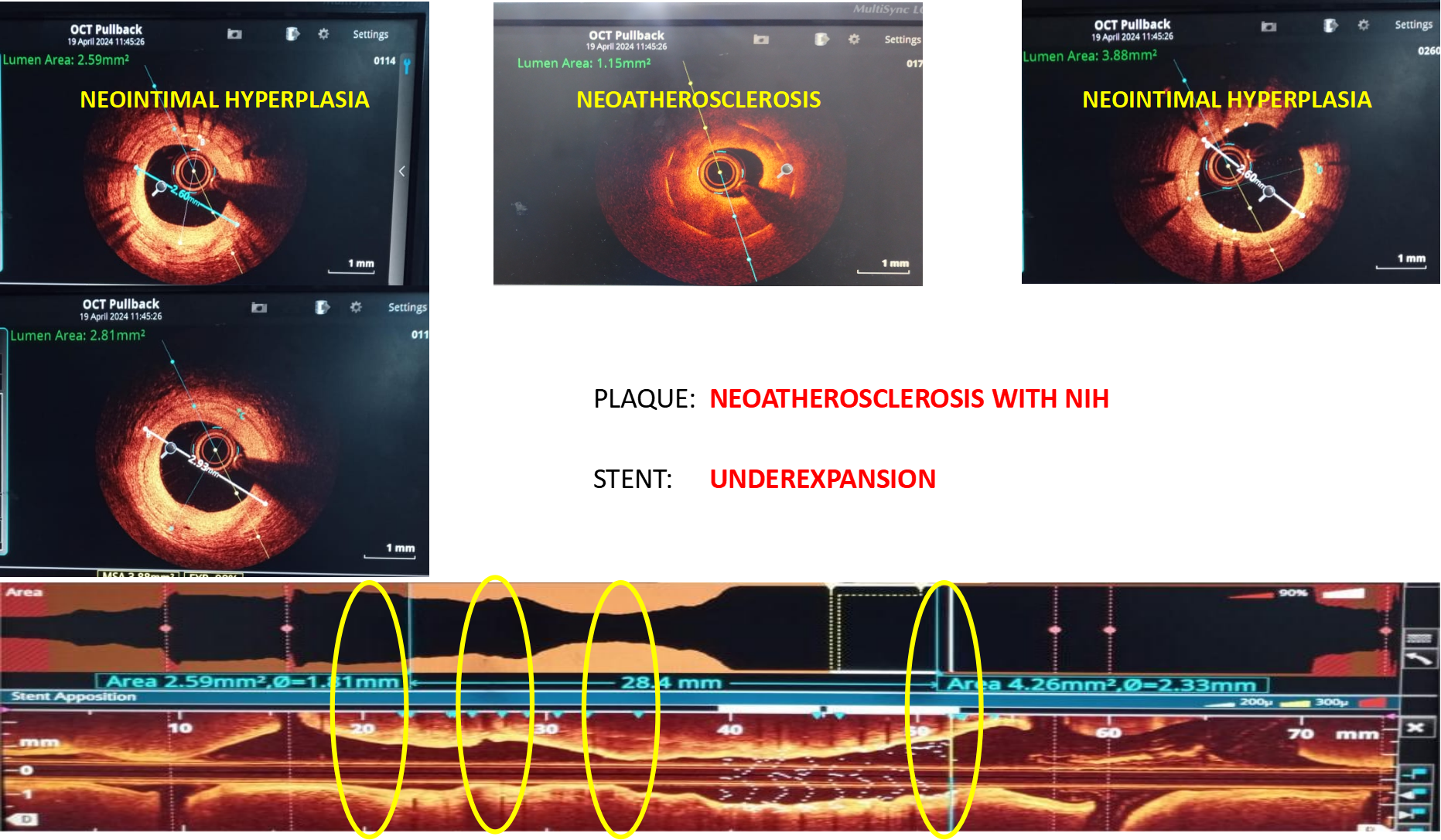
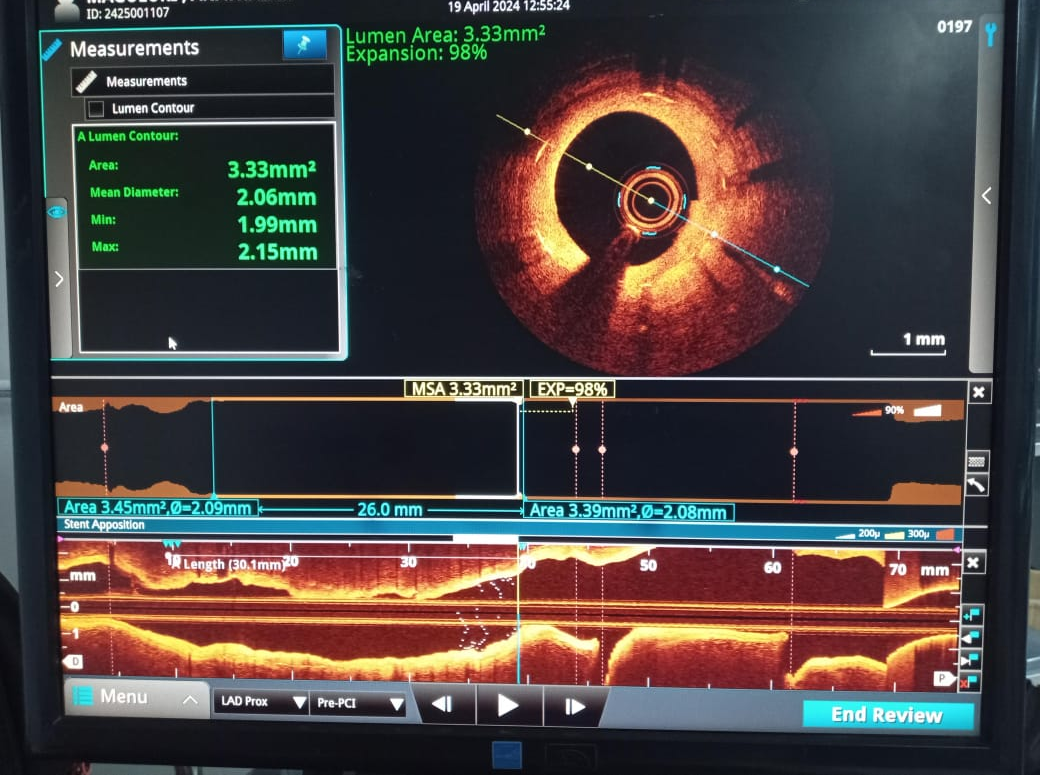
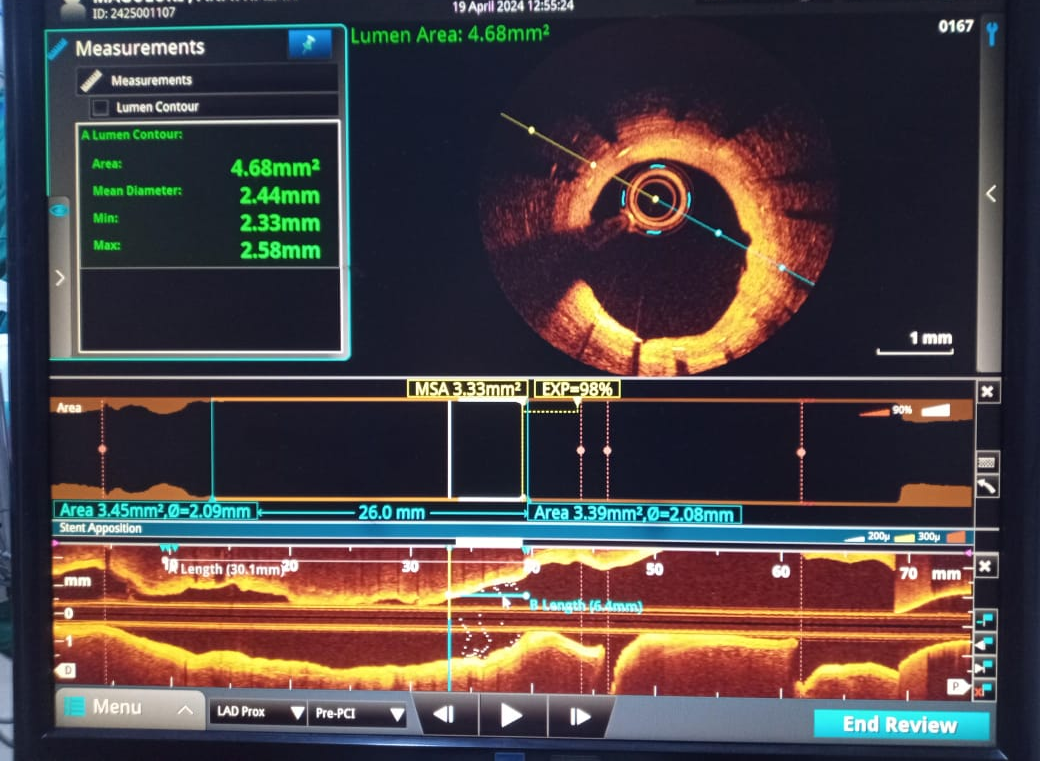
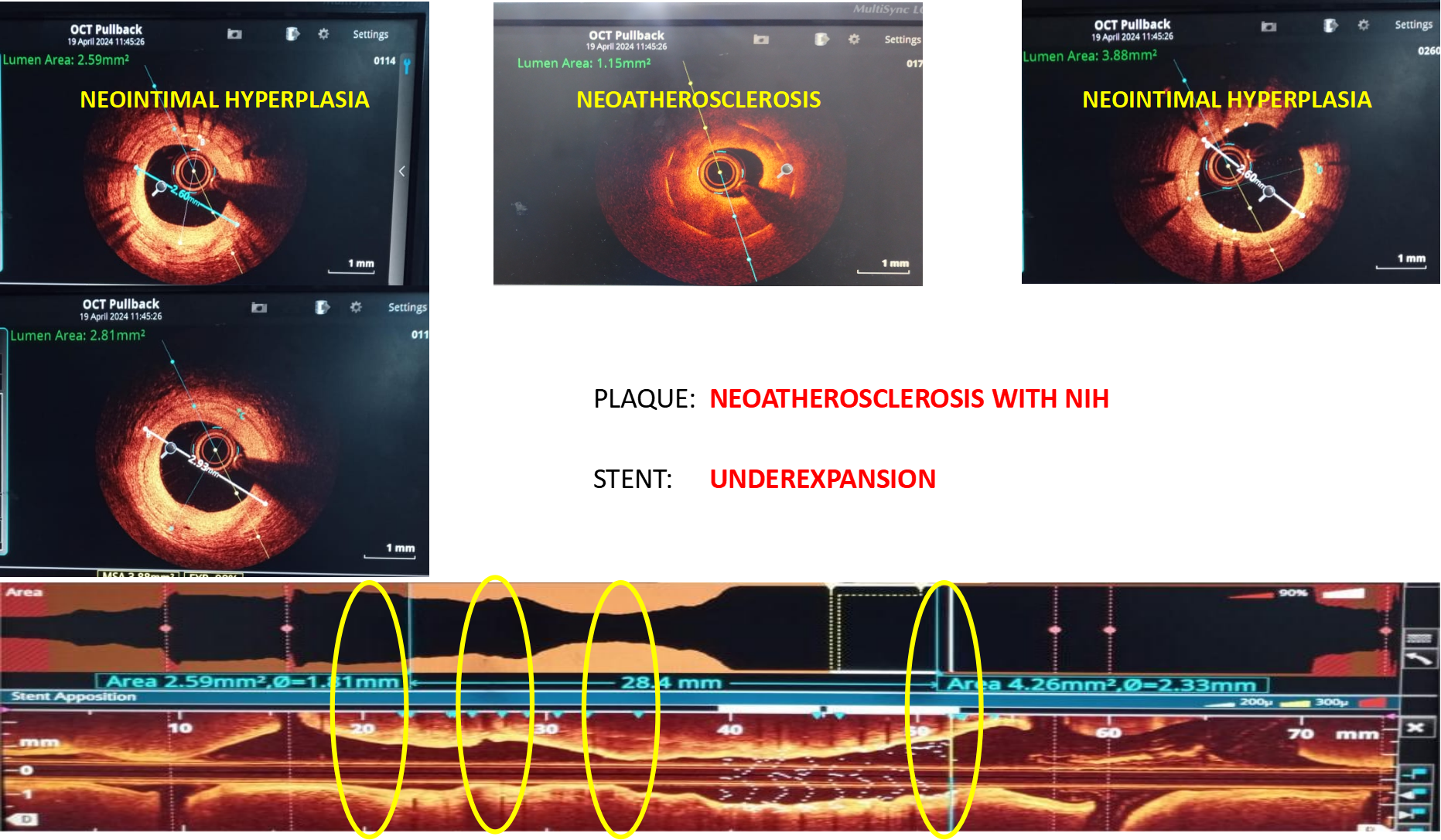
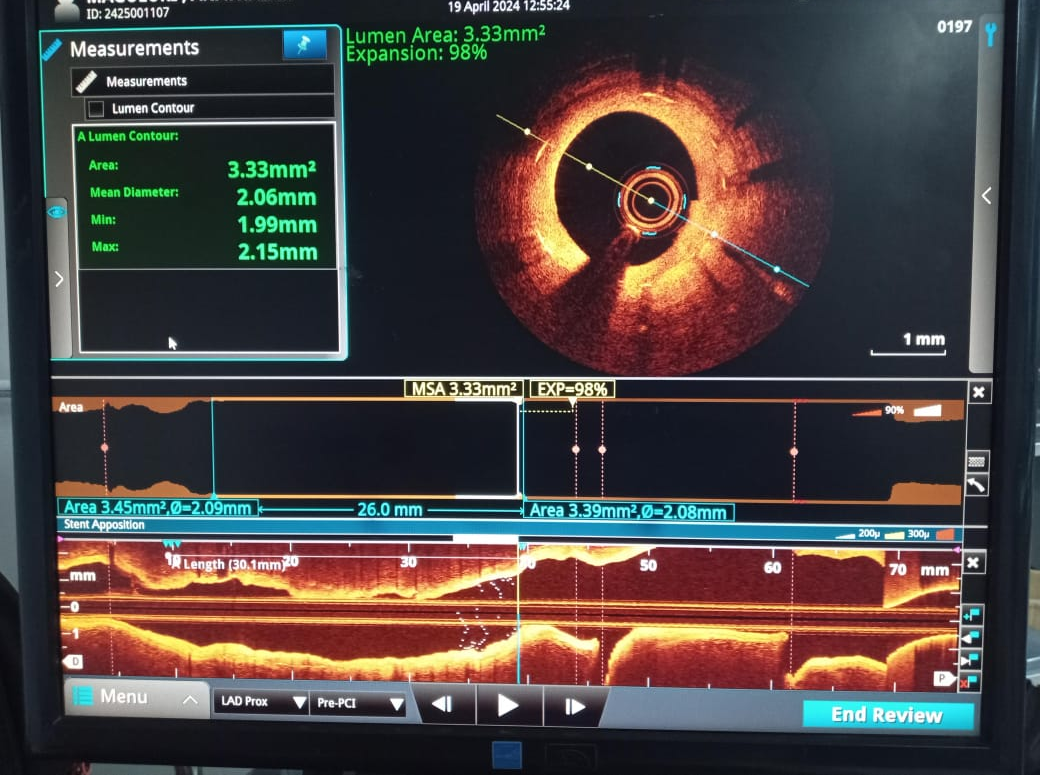
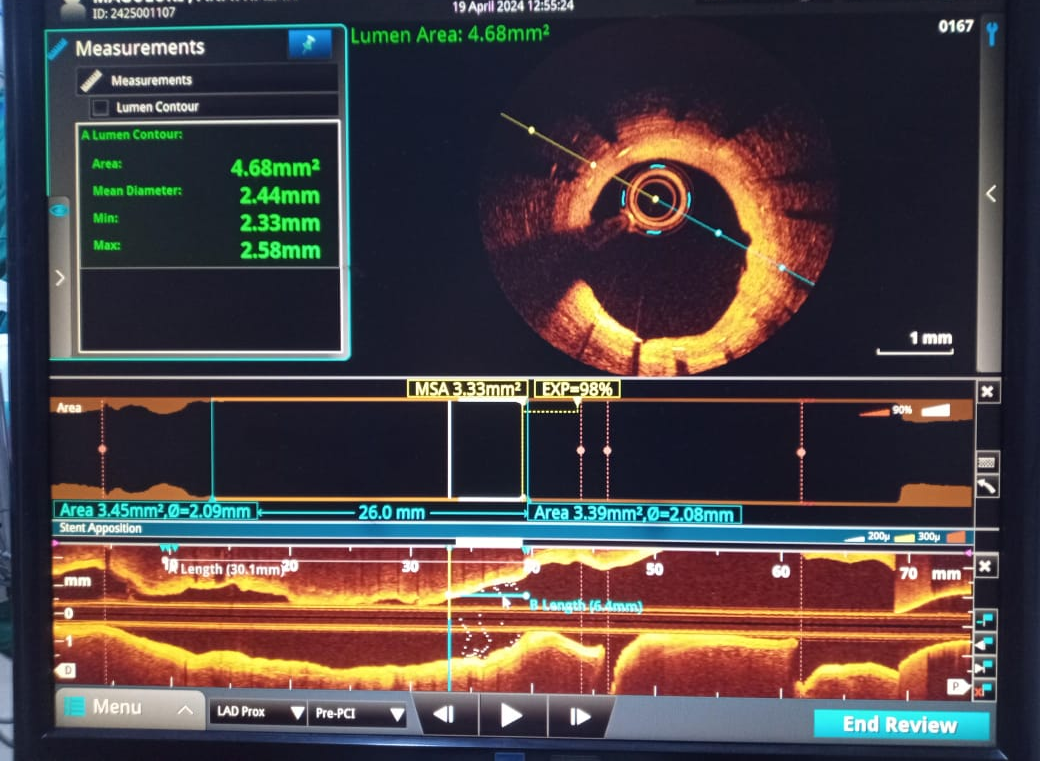
Case Summary
Management of Instent restenosis requires deep insights into the mechanism to treat it. OCT with its high resolution images helps in knowing the plaque morphology , vessel diameter and assessment of plaque modification. In this case we observed only micro tears in the intima inspite of high pressure 1: 1 NC and cutting balloon inflations .This could have been due to the predominance of thick fibrous and elastic tissue within the Neointimal hyperplasia. Significant improvement in stent diameter and MLA showed correction of stent underexpansion. Further studies are needed to assess the relation between post dilation fissures and composition of the lesions in NIH.


