Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-210
Complex Management of Severe Aortic Stenosis and Multivessel Coronary Artery Disease in a Frail, Small-Stature Patient: Transition From Cardiogenic Shock to Transcarotid TAVR
By Wittawin Wangpermpoon, Thinnakrit Sasiprapha, Tawai Ngernsritrakul, Mann Chandavimol
Presenter
Wittawin Wangpermpoon
Authors
Wittawin Wangpermpoon1, Thinnakrit Sasiprapha1, Tawai Ngernsritrakul1, Mann Chandavimol1
Affiliation
Ramathibodi Hospital, Thailand1,
View Study Report
TCTAP C-210
Structural - Aortic Valve Intervention - Non-femoral TAVR
Complex Management of Severe Aortic Stenosis and Multivessel Coronary Artery Disease in a Frail, Small-Stature Patient: Transition From Cardiogenic Shock to Transcarotid TAVR
Wittawin Wangpermpoon1, Thinnakrit Sasiprapha1, Tawai Ngernsritrakul1, Mann Chandavimol1
Ramathibodi Hospital, Thailand1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
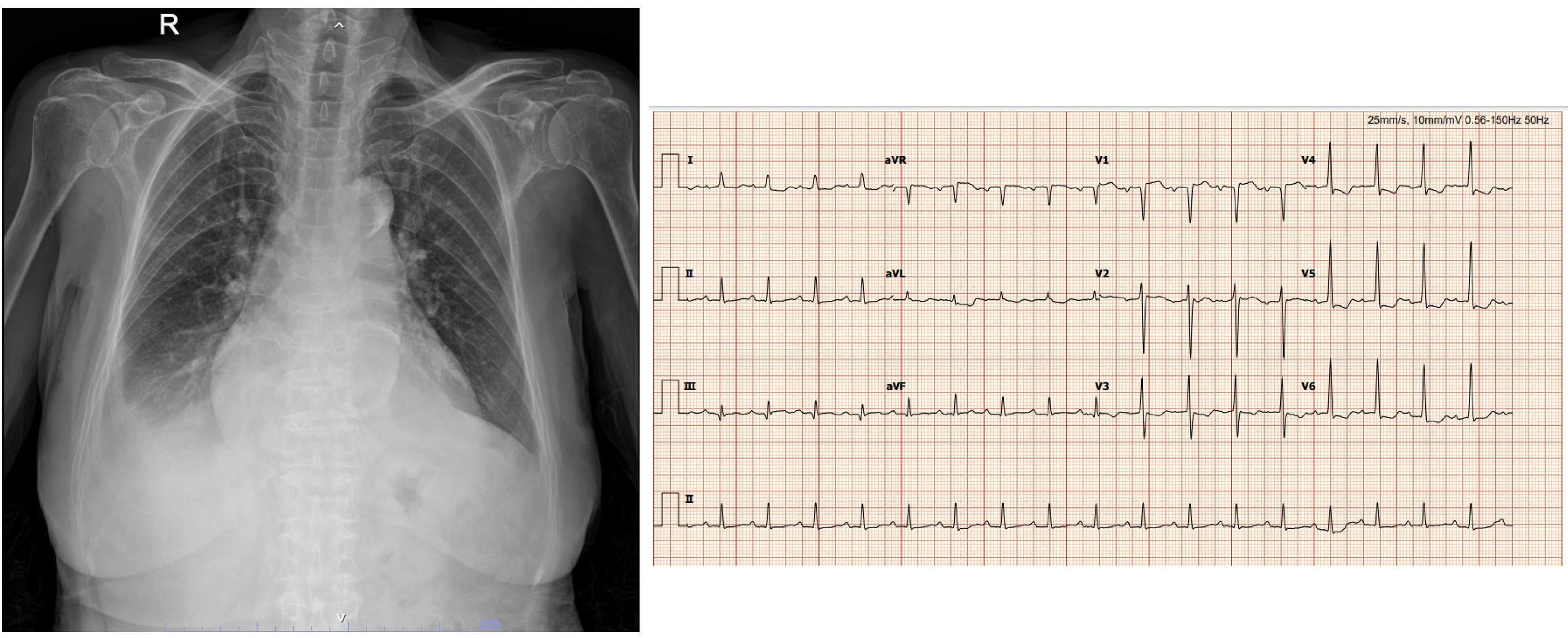
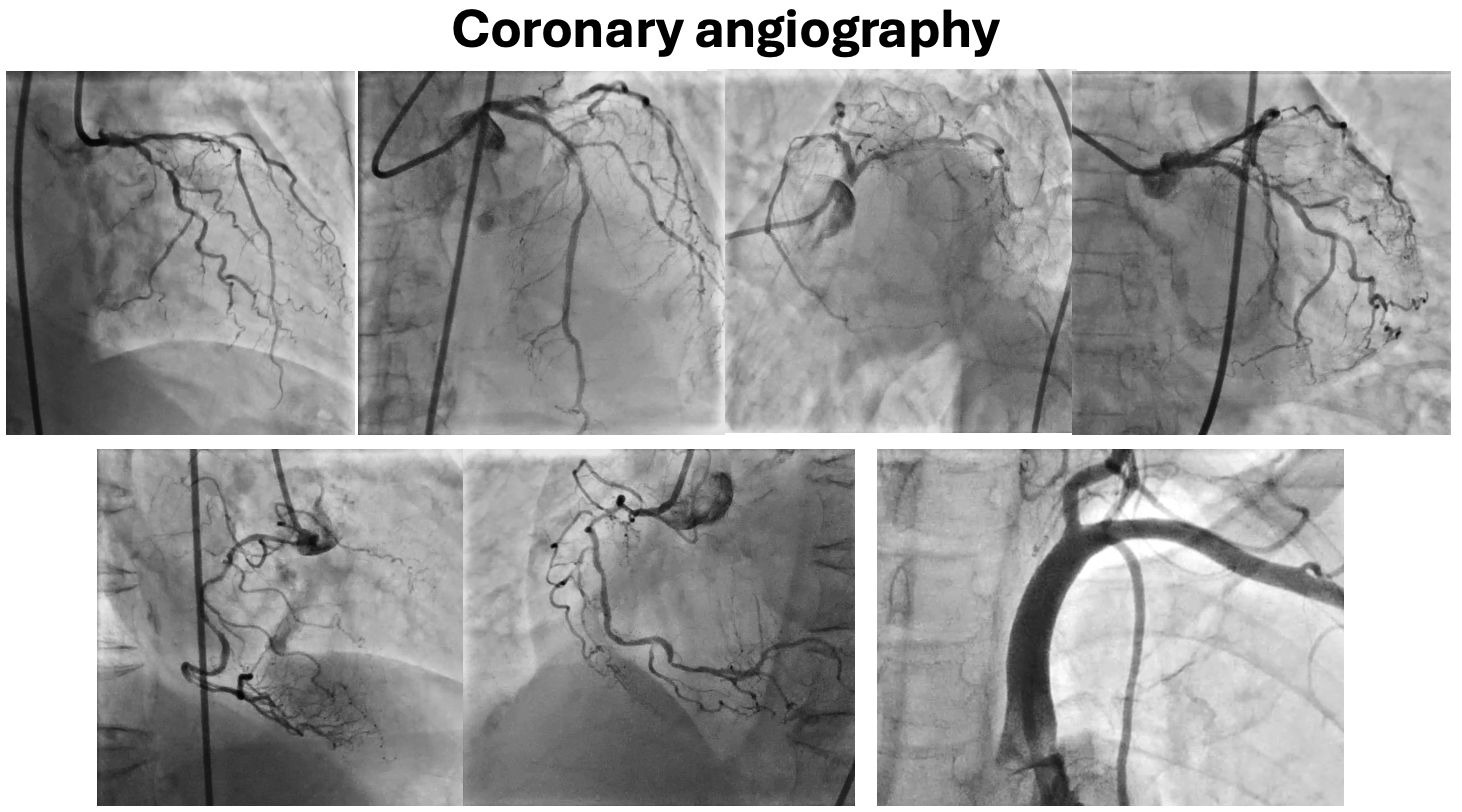
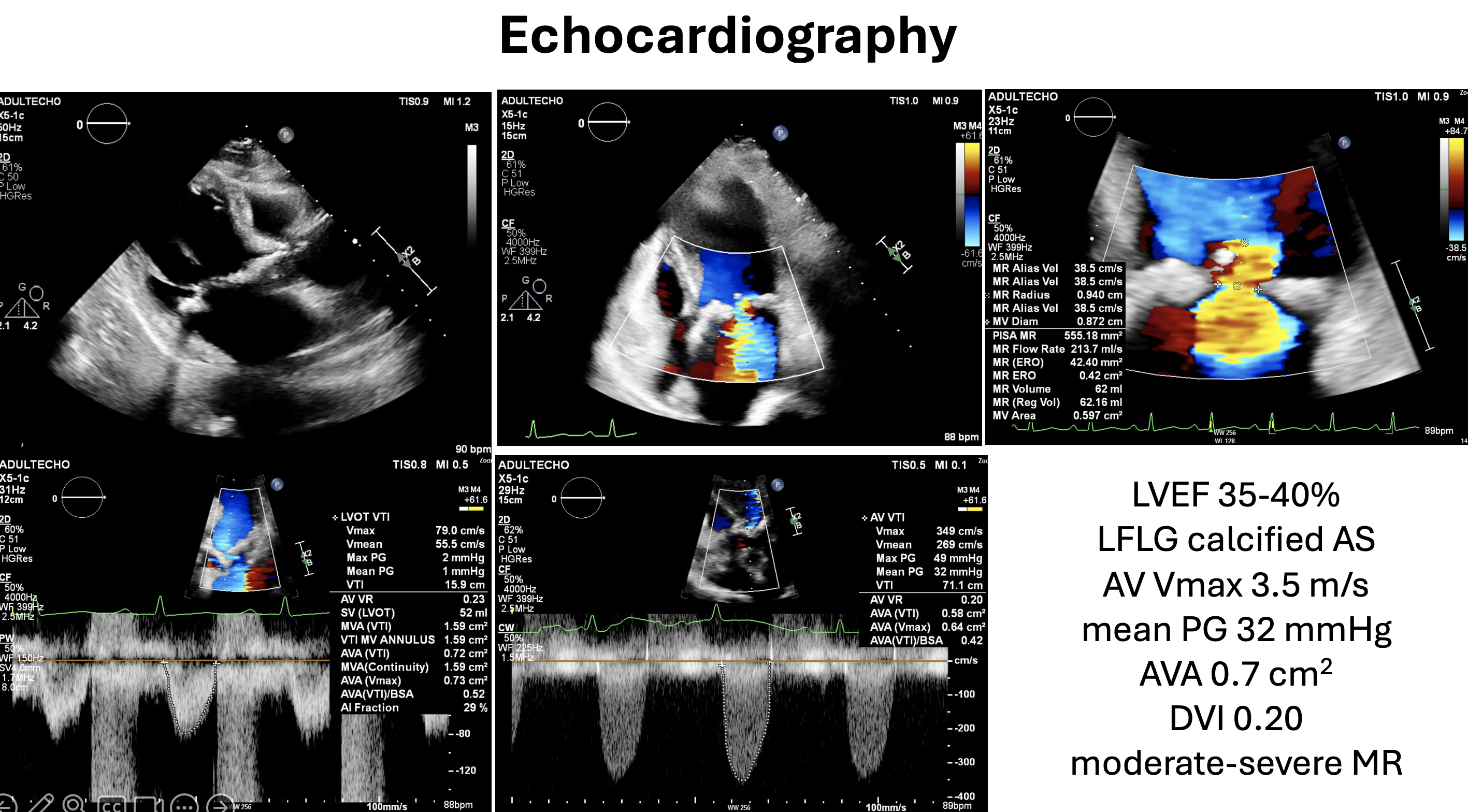
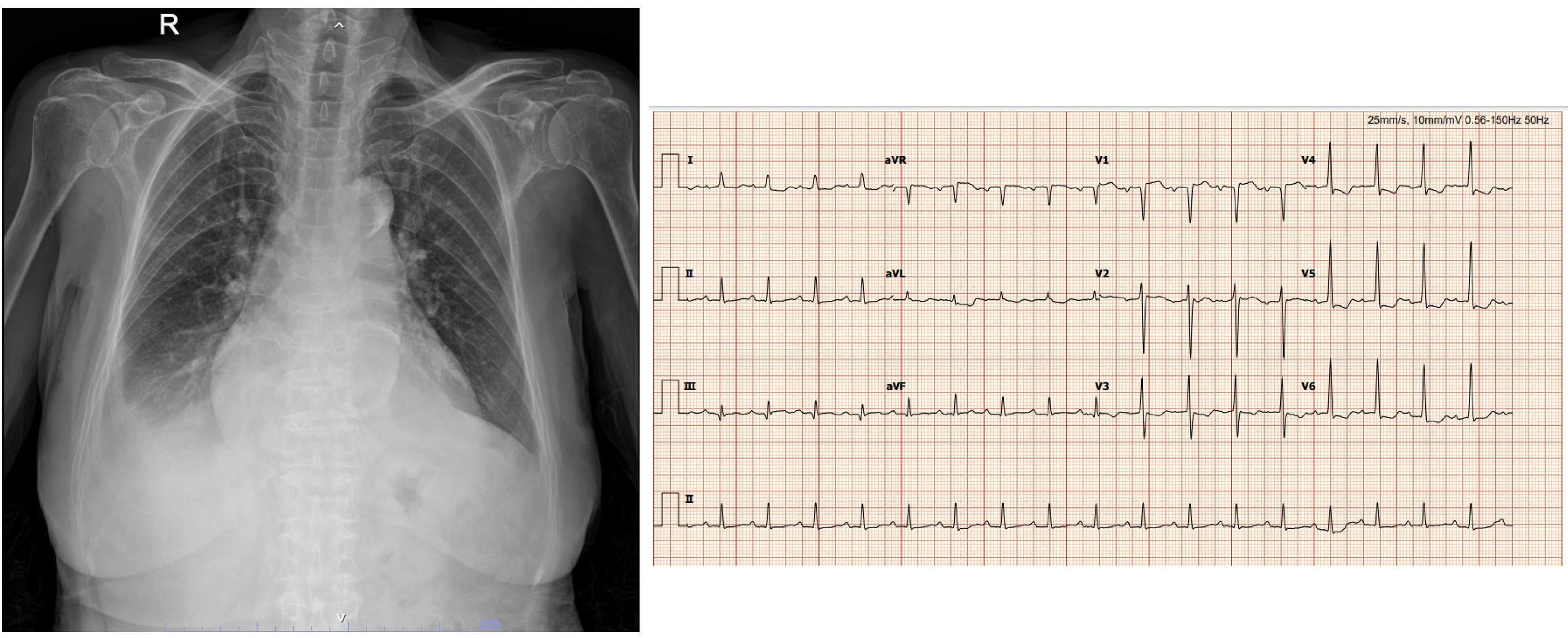
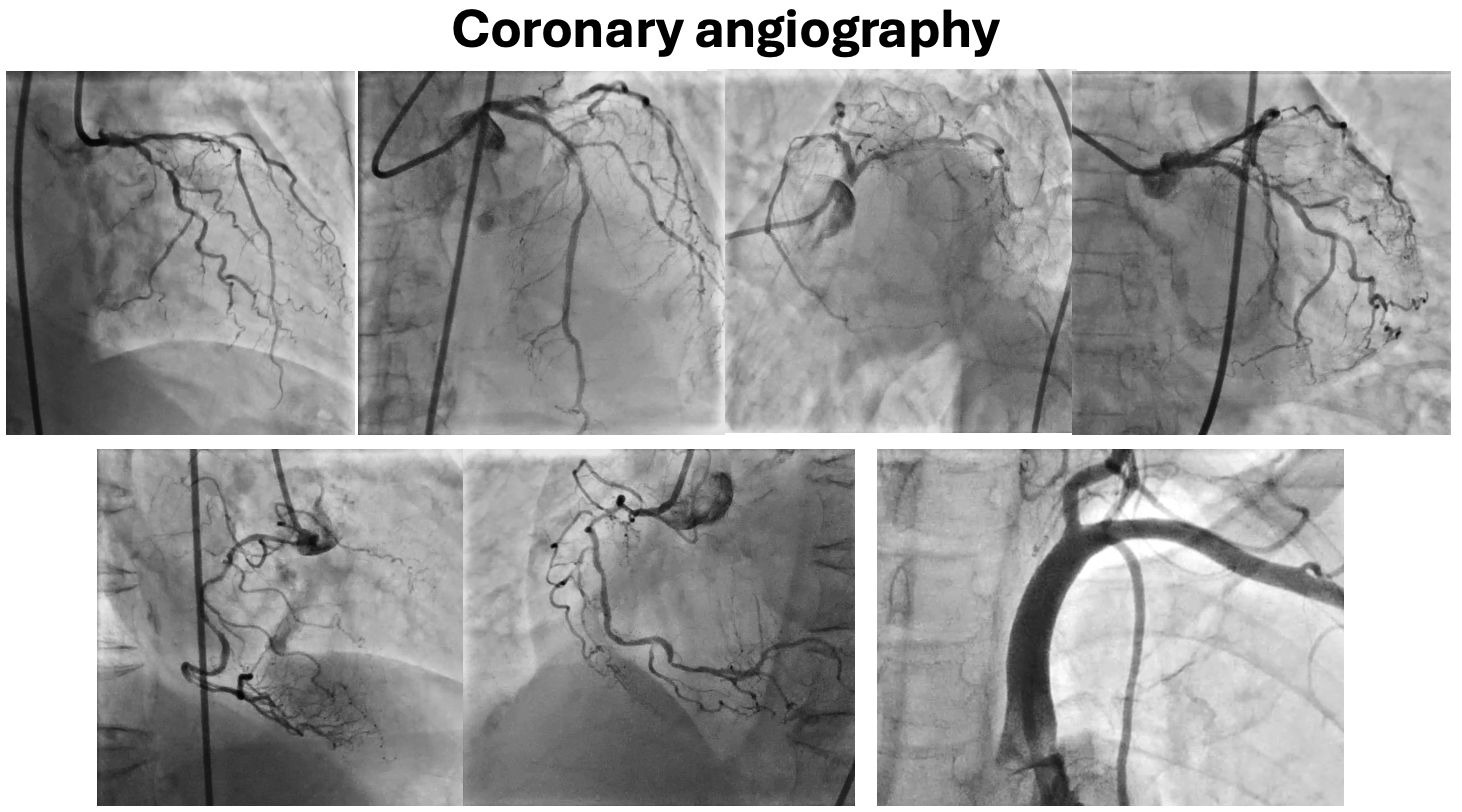
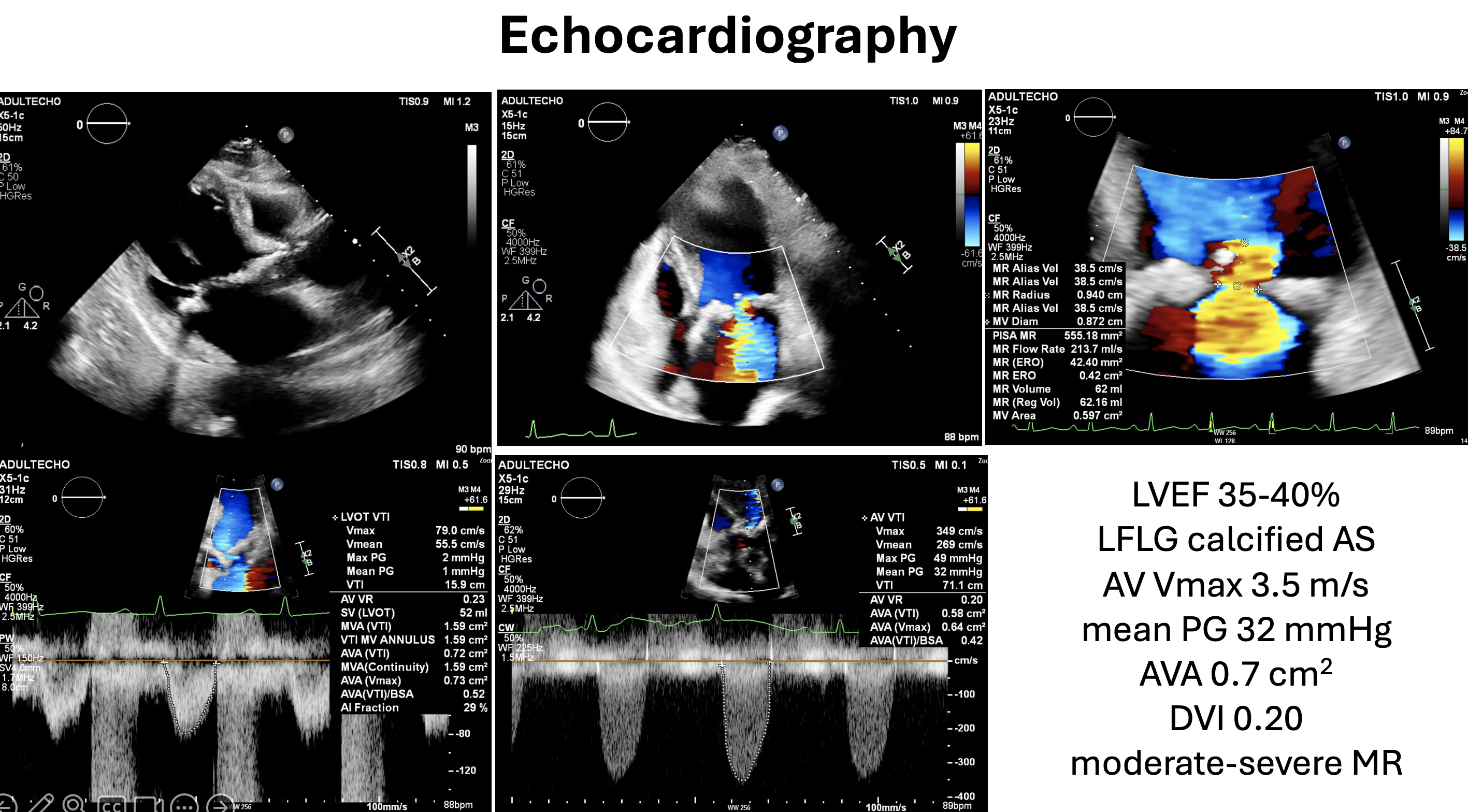
70 YOF with DM, DLP, and HT presented with worsening dyspnea over two weeks and a two-year decline in functional status. She appeared hyposthenic (BW 35 kg, BSA 1.23 m) V/S: BP 94/54 mmHg, RR 28 bpm, PR 102 bpm. Physical exam revealed JVP elevation, S3 gallop, murmurs, and lung crepitations. ECG showed sinus tachycardia, AVR STE, and ST depression. Echo revealed LVEF 40%, moderate to severe MR, and low-gradient AS. CAG showed TVD with LM disease. CABG with DVR was advised from conference
Relevant Test Results Prior to Catheterization
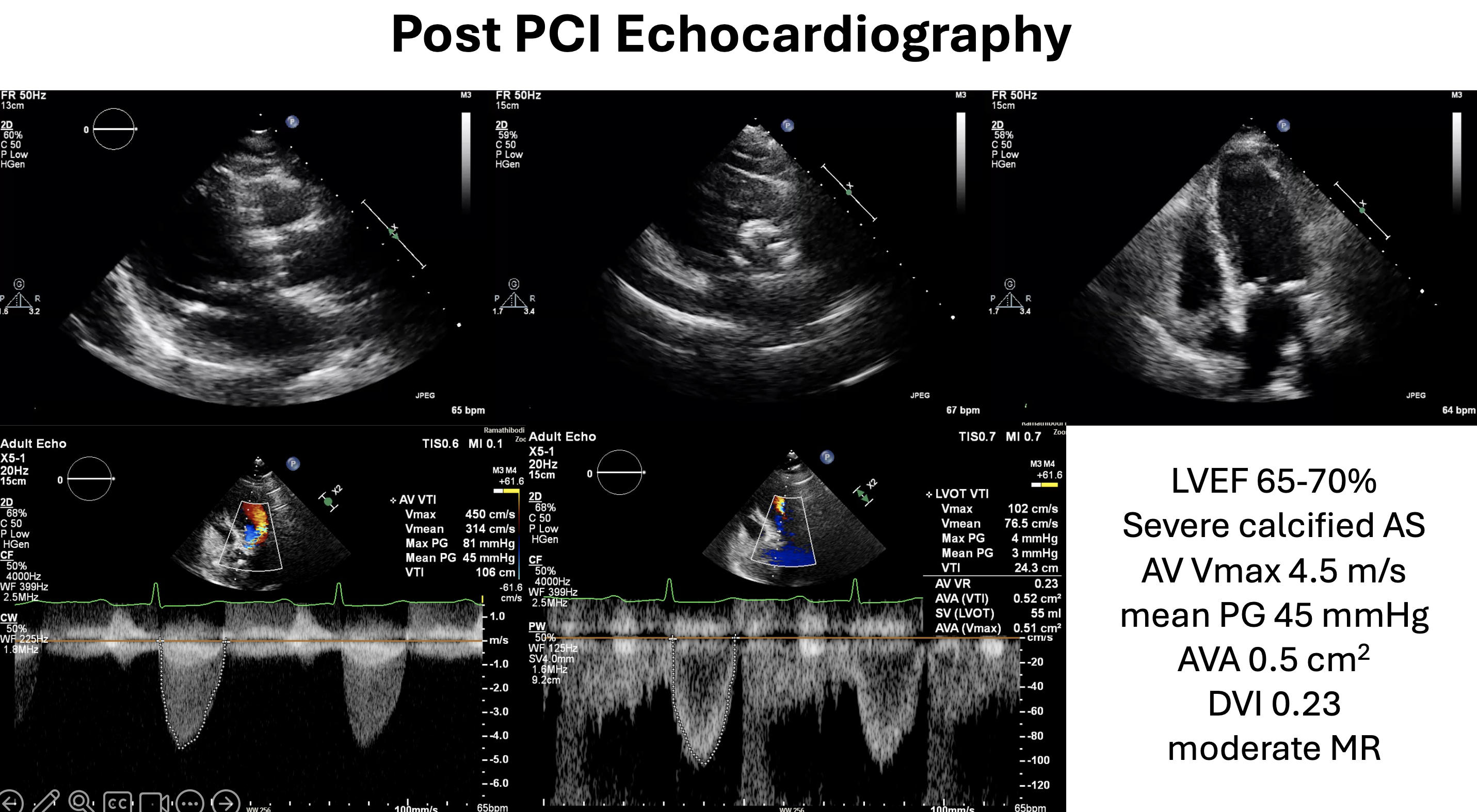
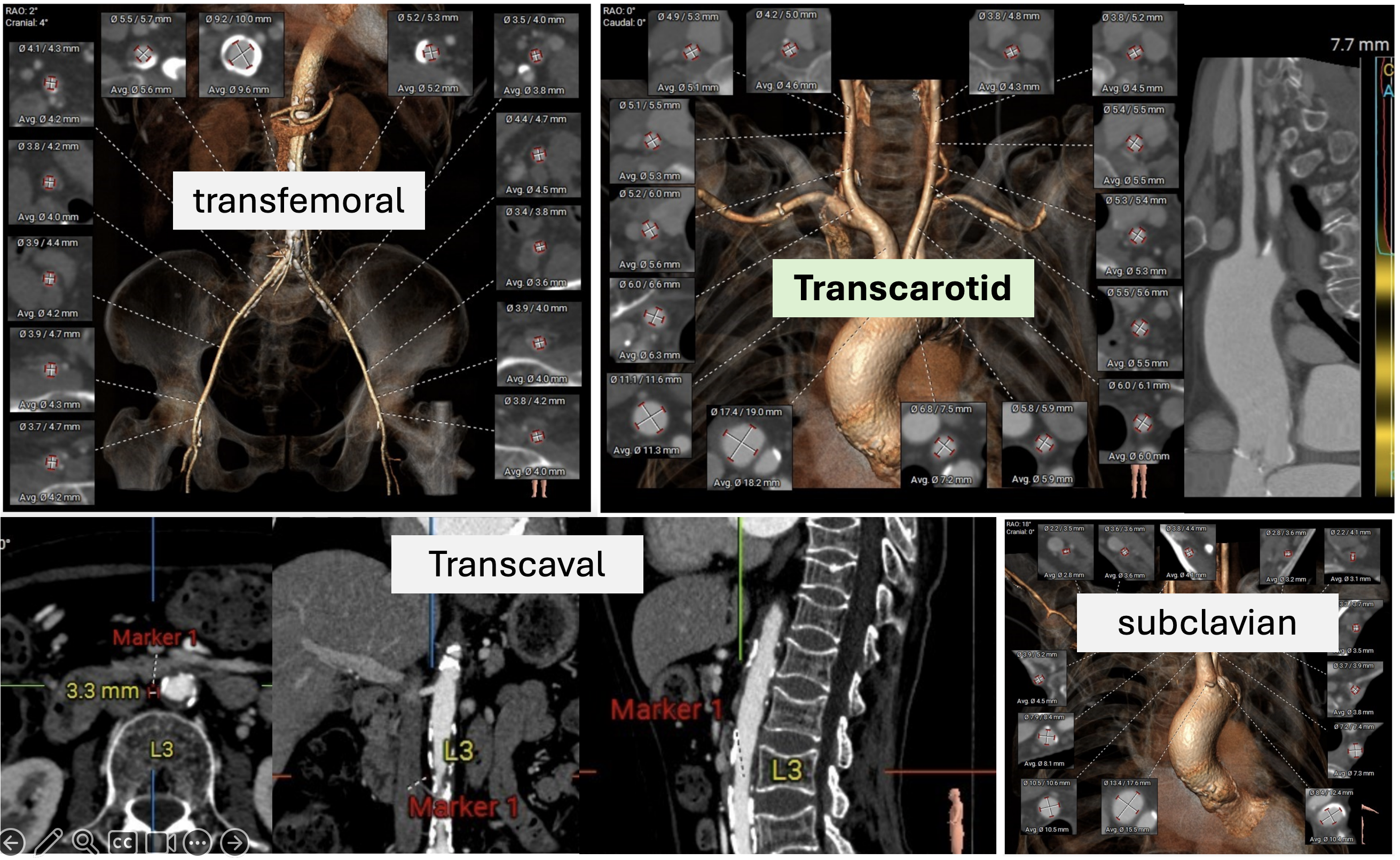
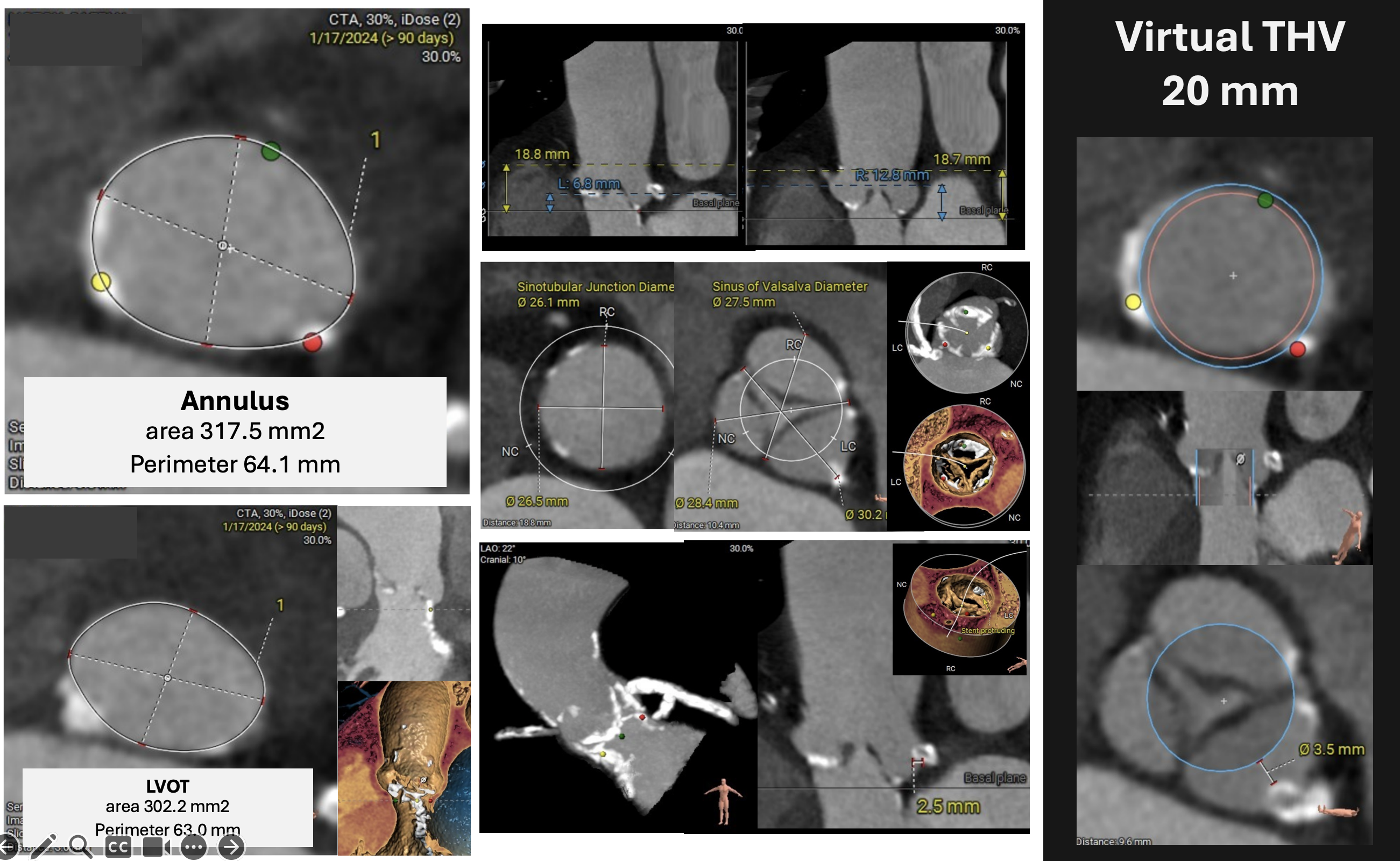
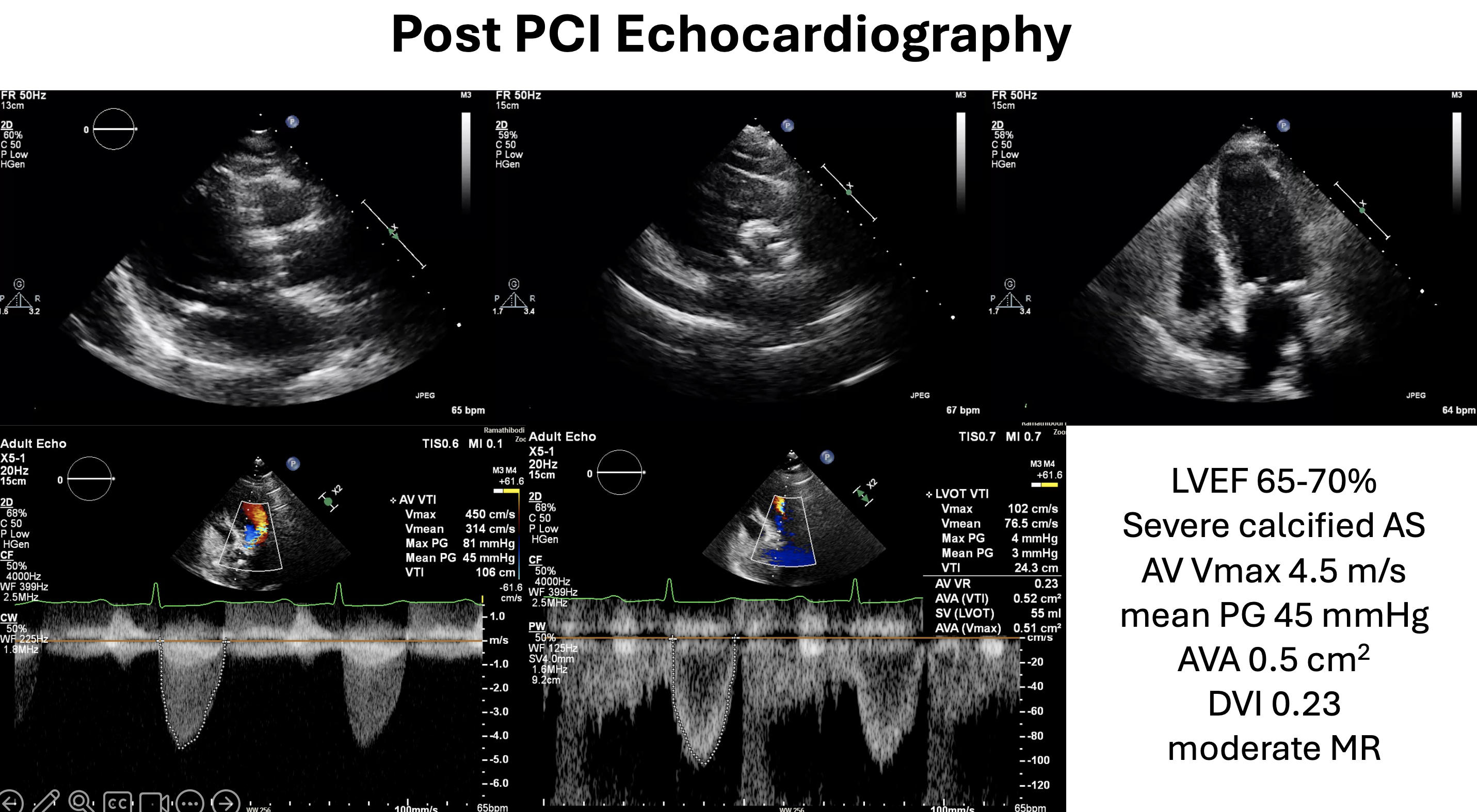
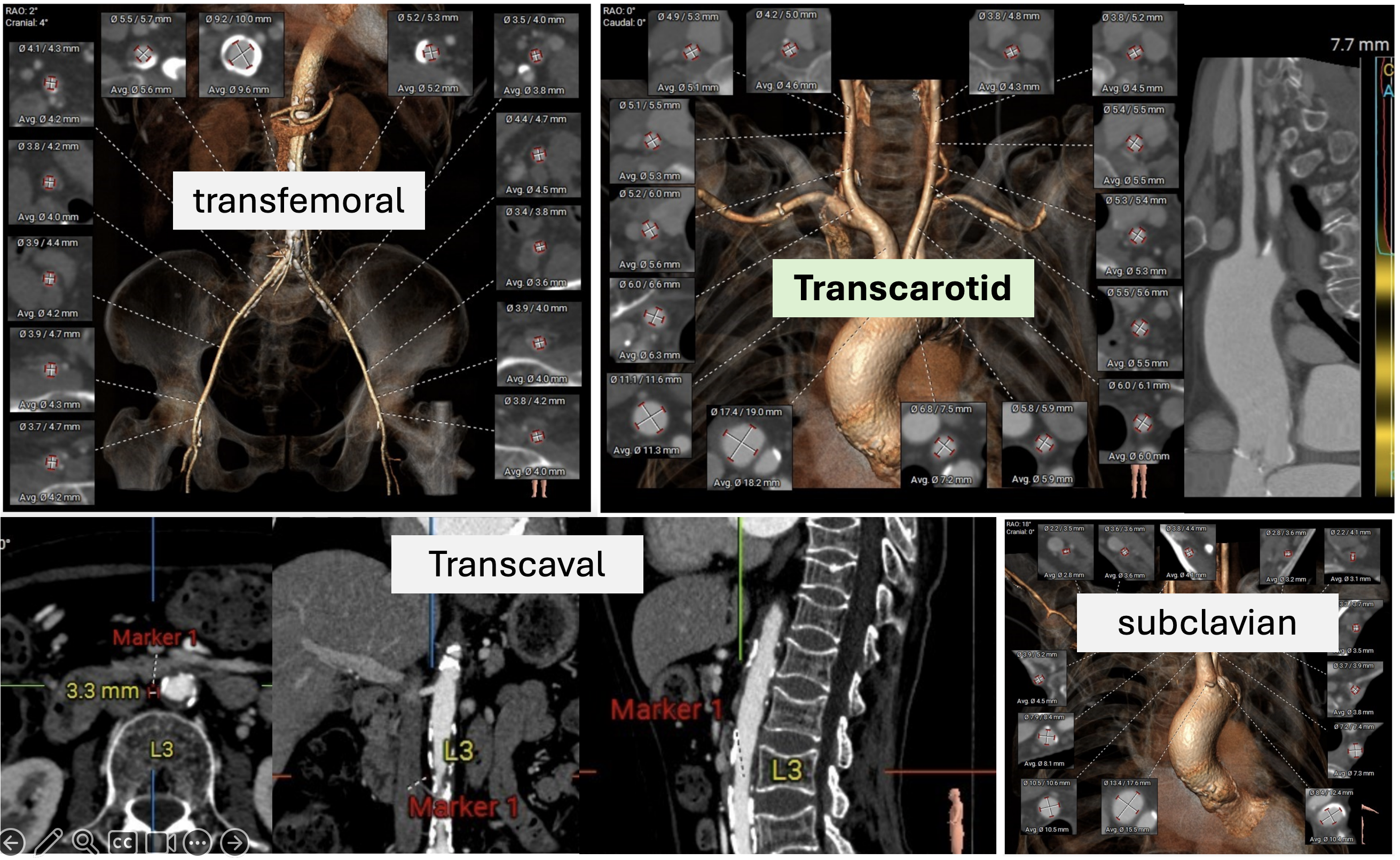
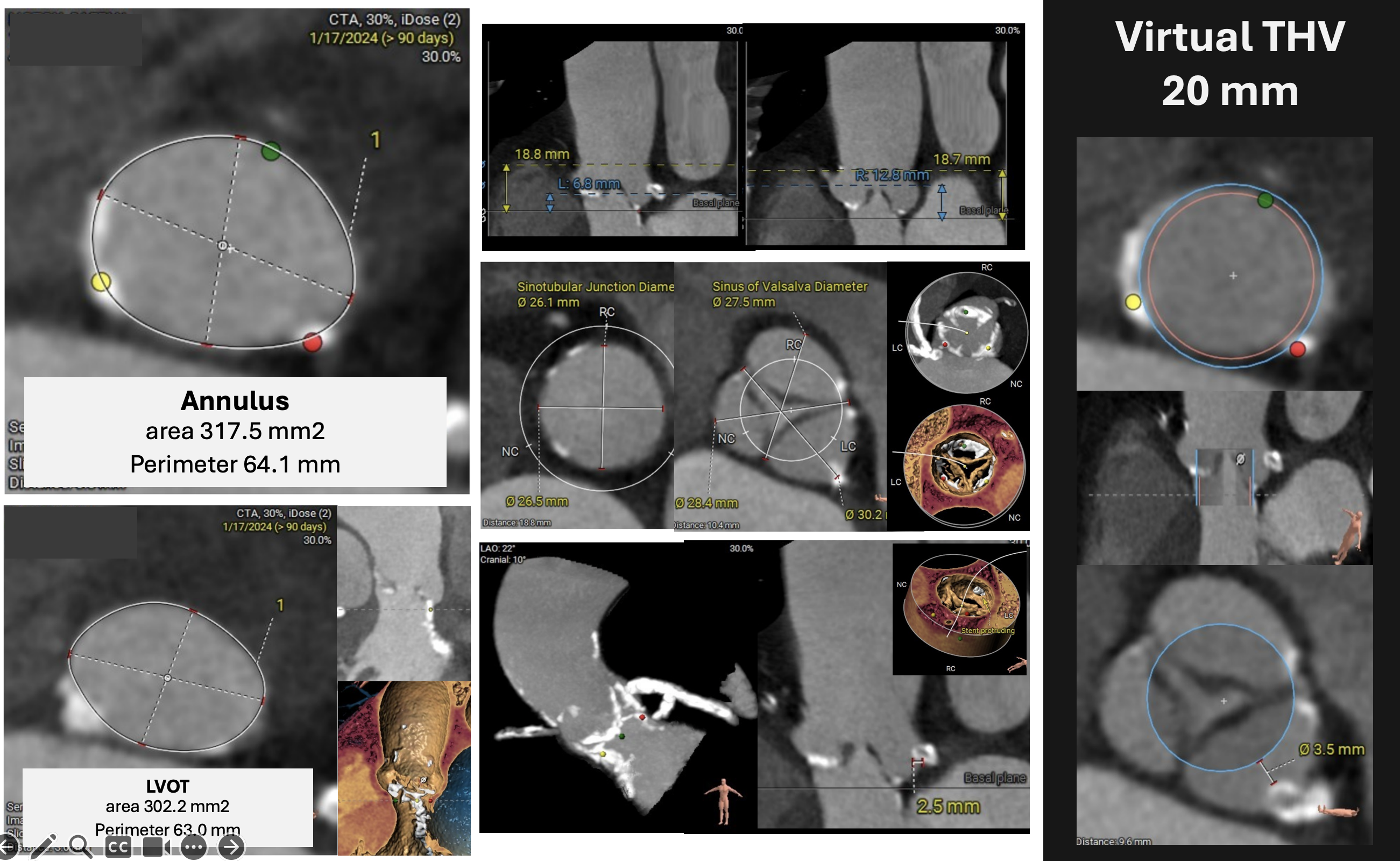
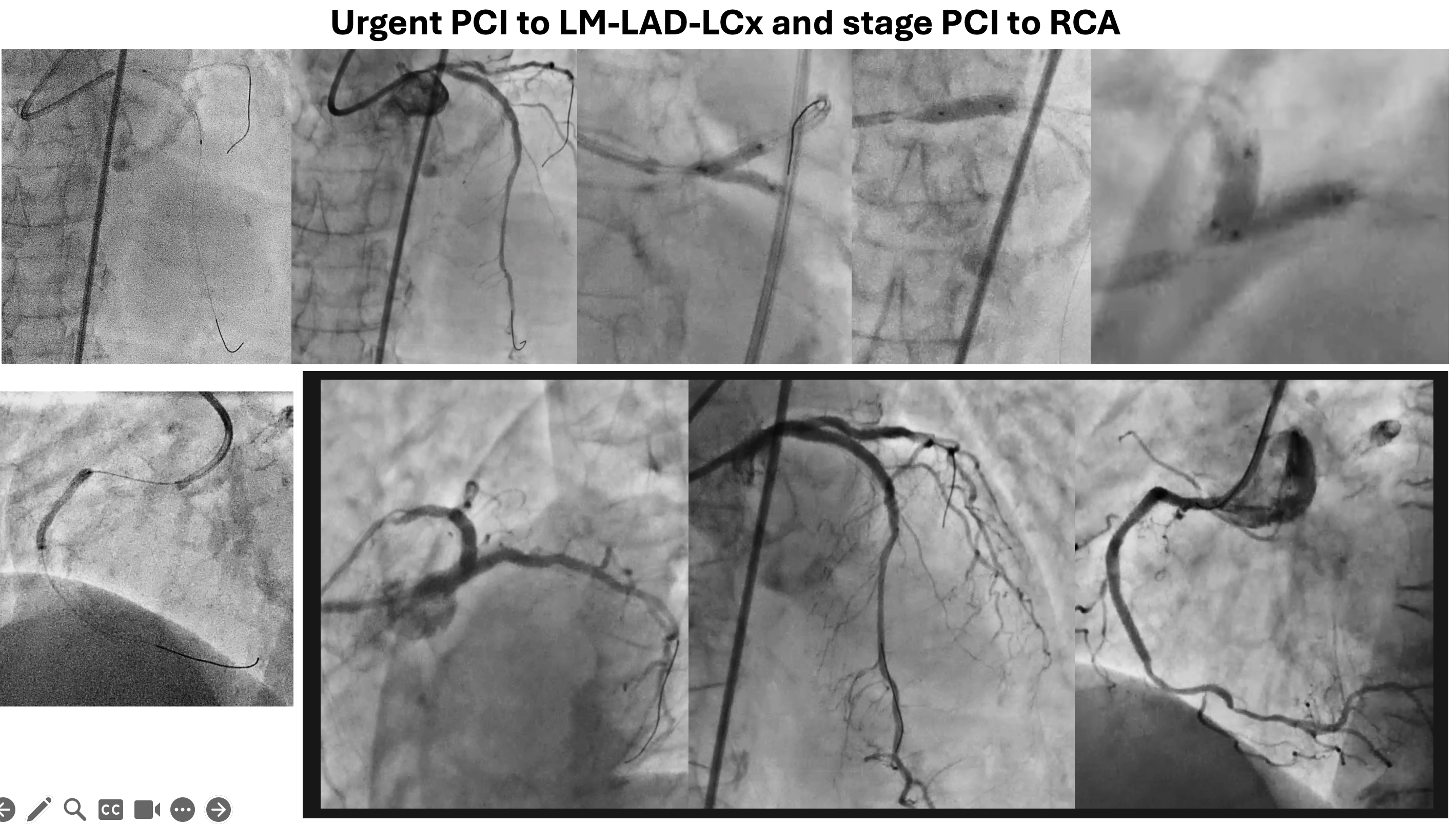
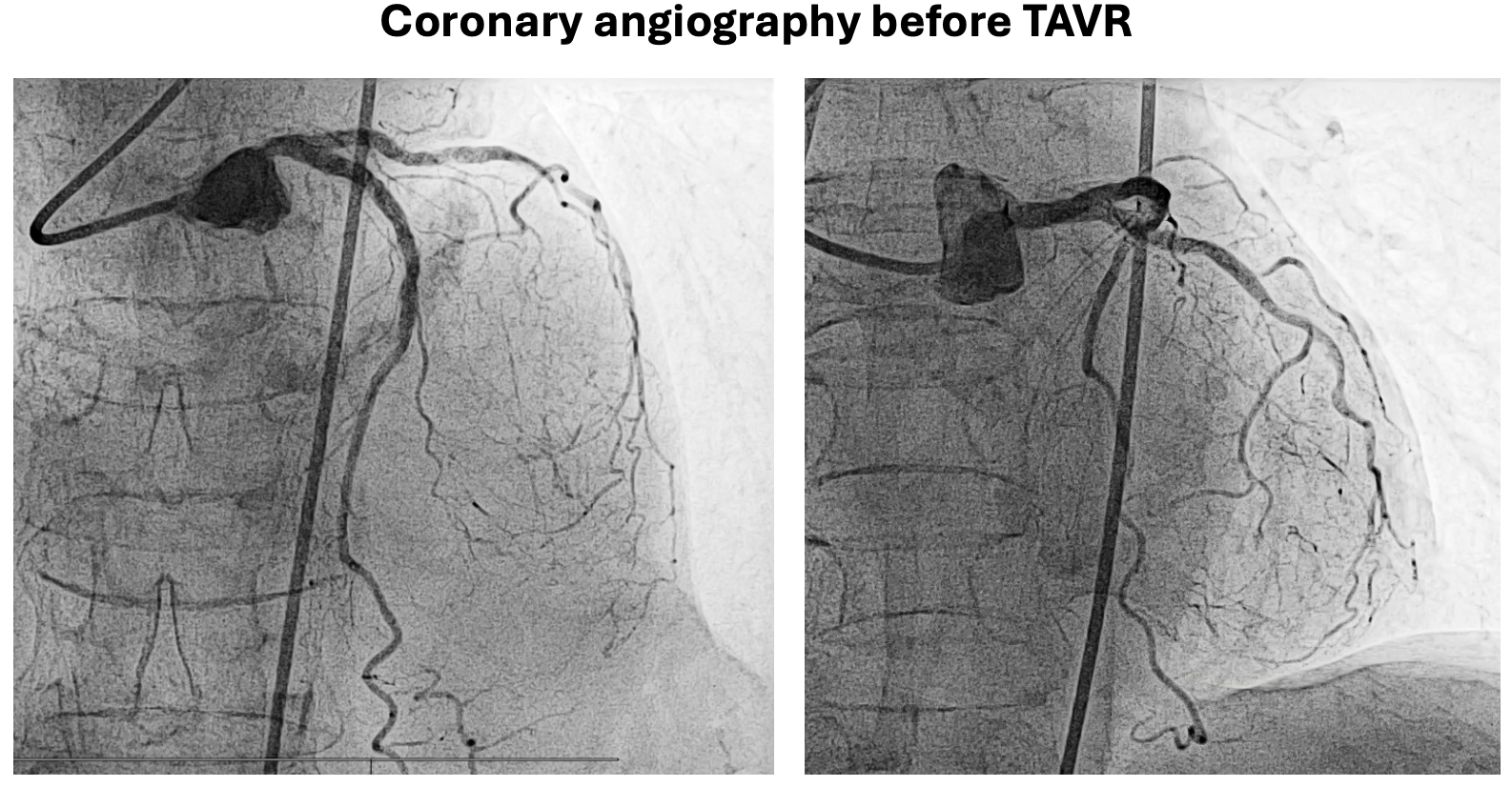
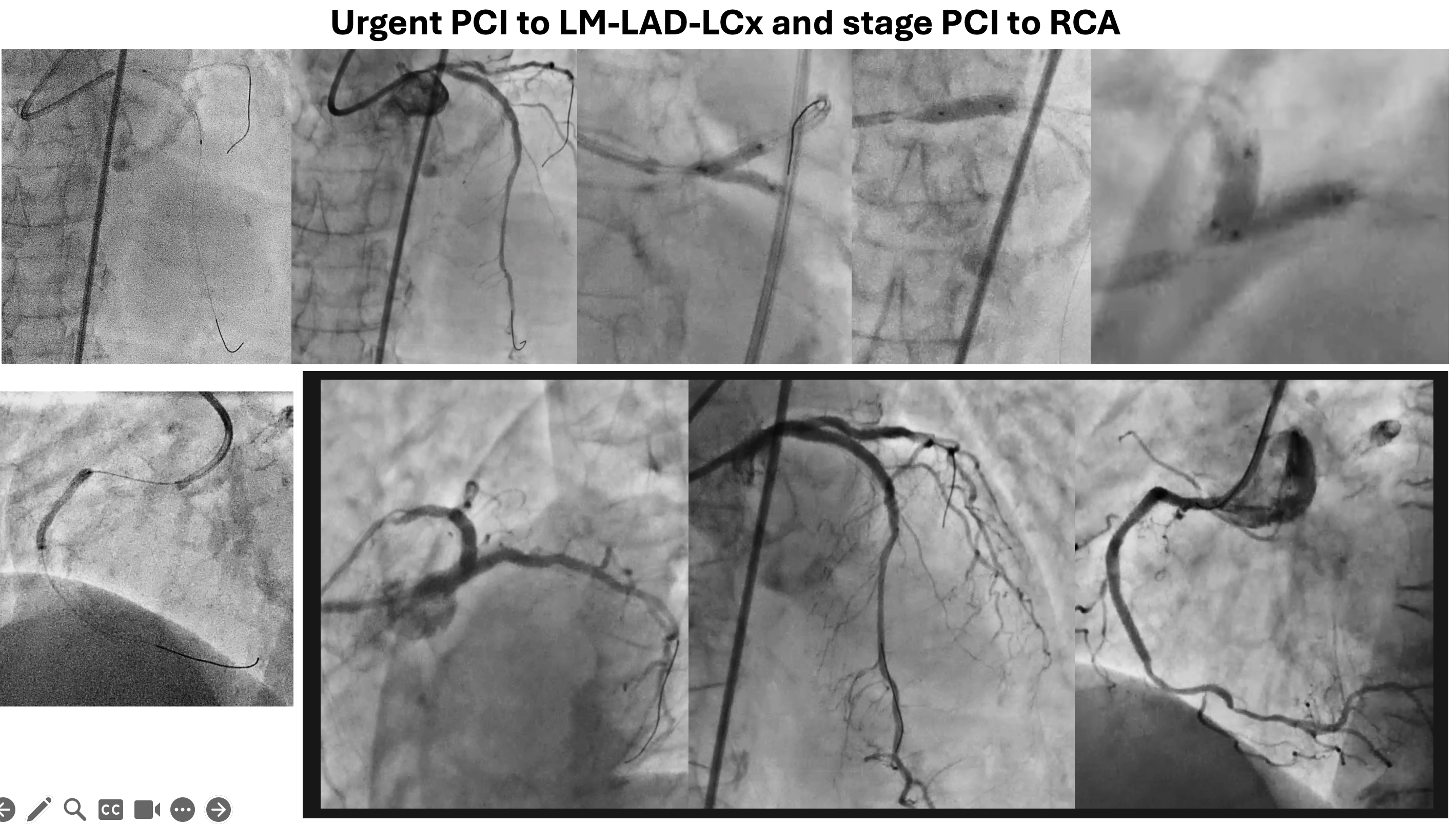
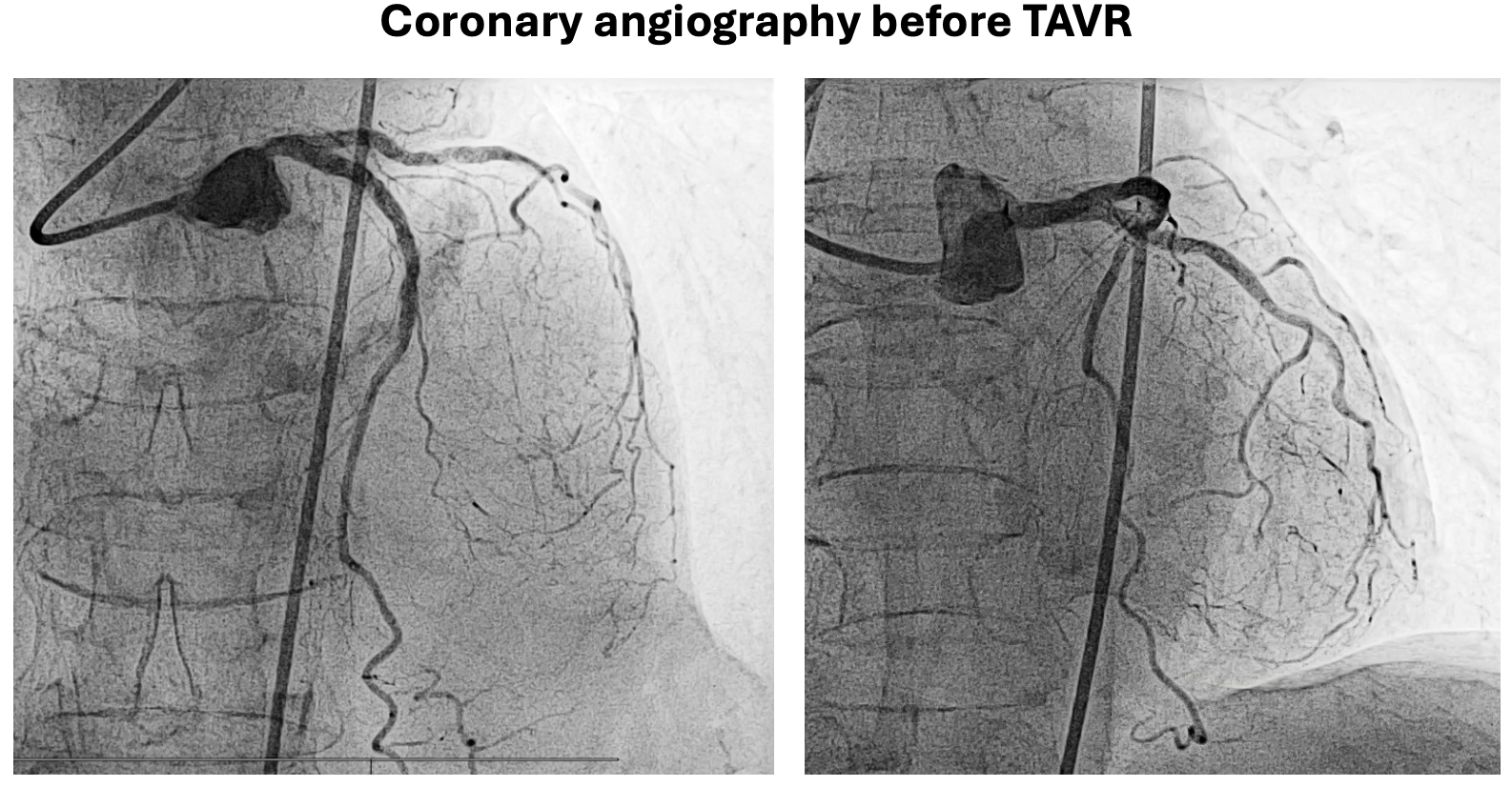
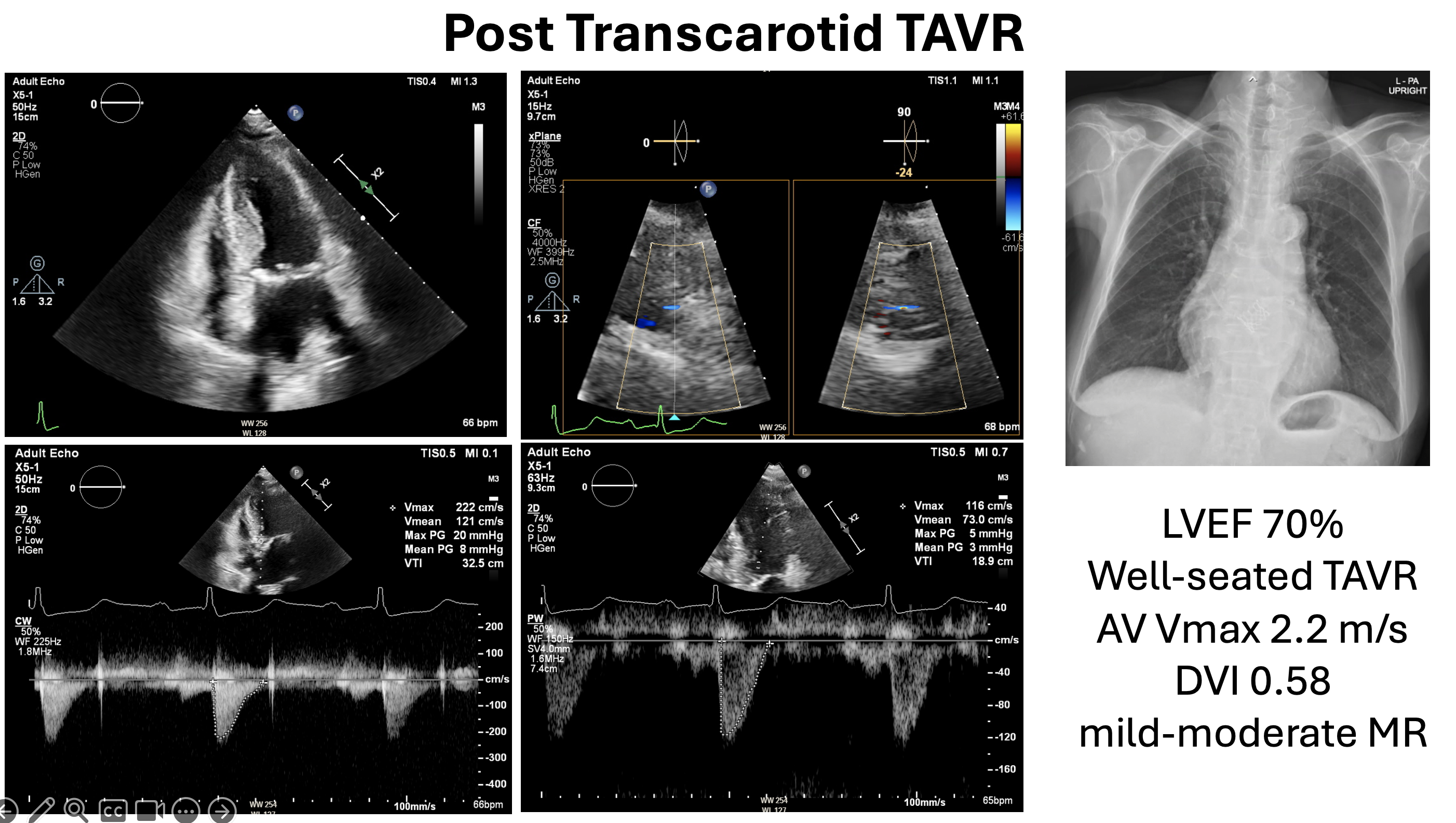
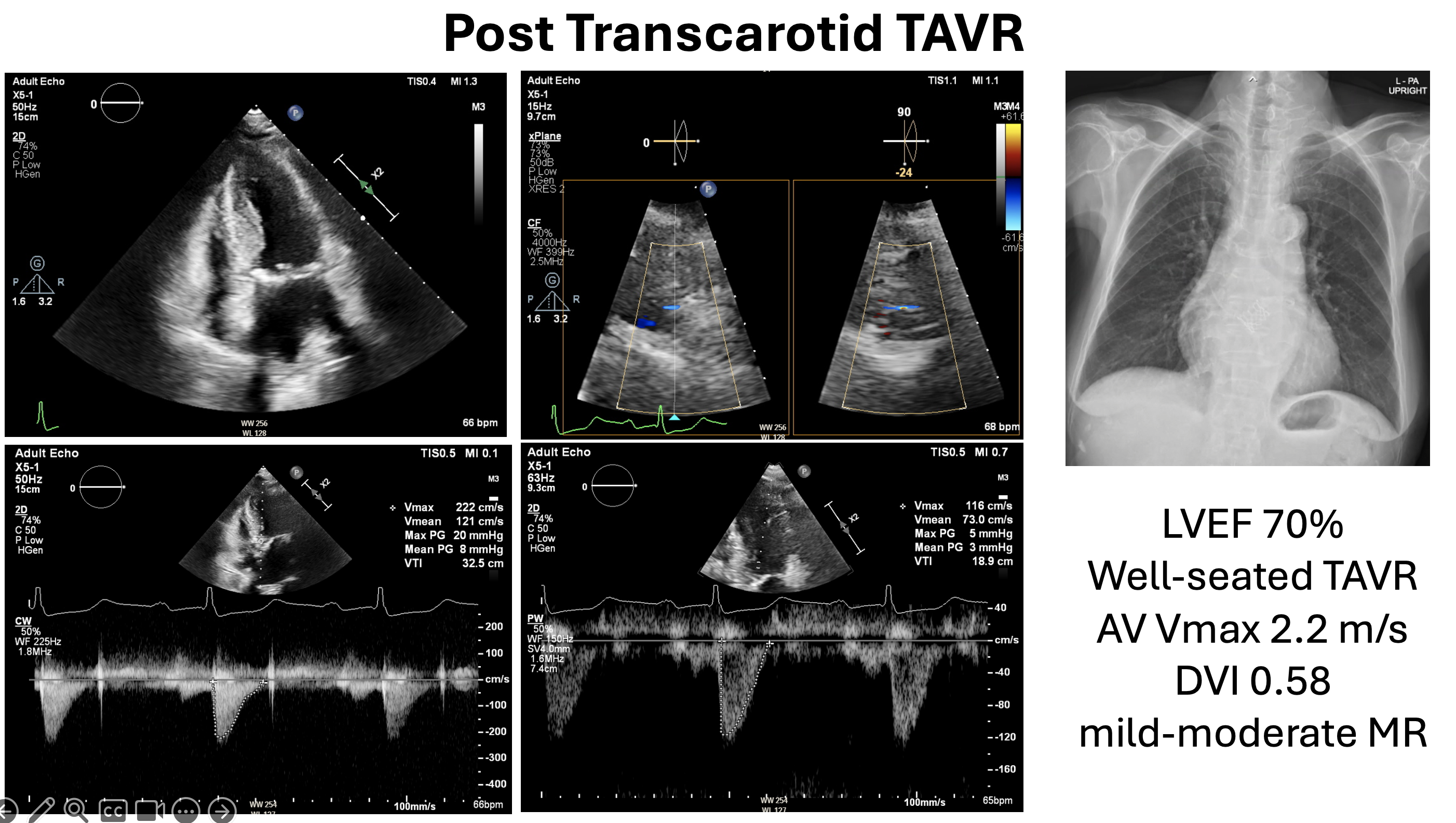
The patient experienced sudden deterioration with cardiogenic shock while awaiting surgery, urgent PCI on the LM bifurcation using a 2-stent DK crush technique, followed by staged PCI. Post-PCI, her LVEF improved to 65%, revealing severe AS (AV Vmax 4.5 m/s, mean PG 45 mmHg, AVA 0.5 cm², DVI 0.23) and moderate MR. CTA showed a small annulus (317.5 mm²), LVOT calcification, short LCA height (6.8 mm), and small femoral arteries (4 mm), making the left carotid artery the most suitable access.
Relevant Catheterization Findings
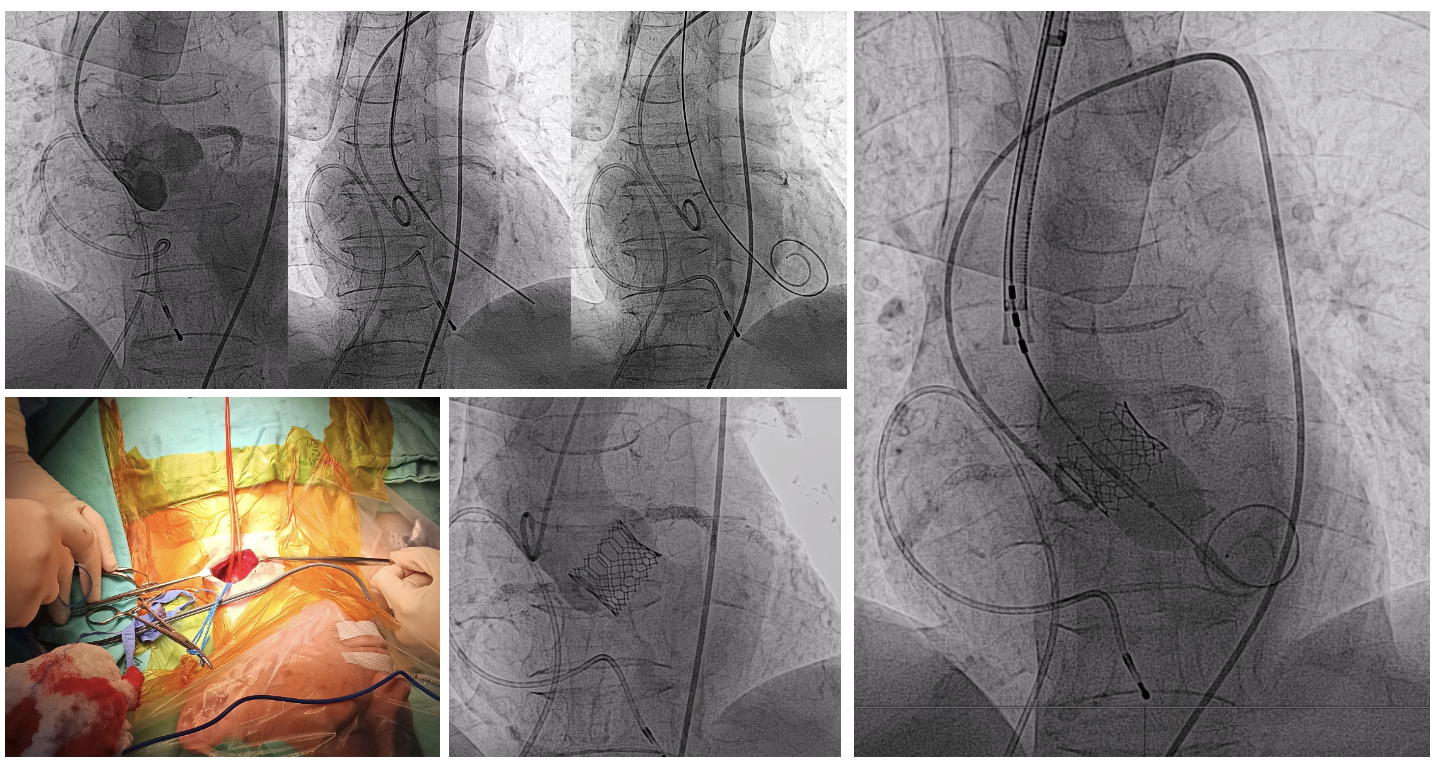
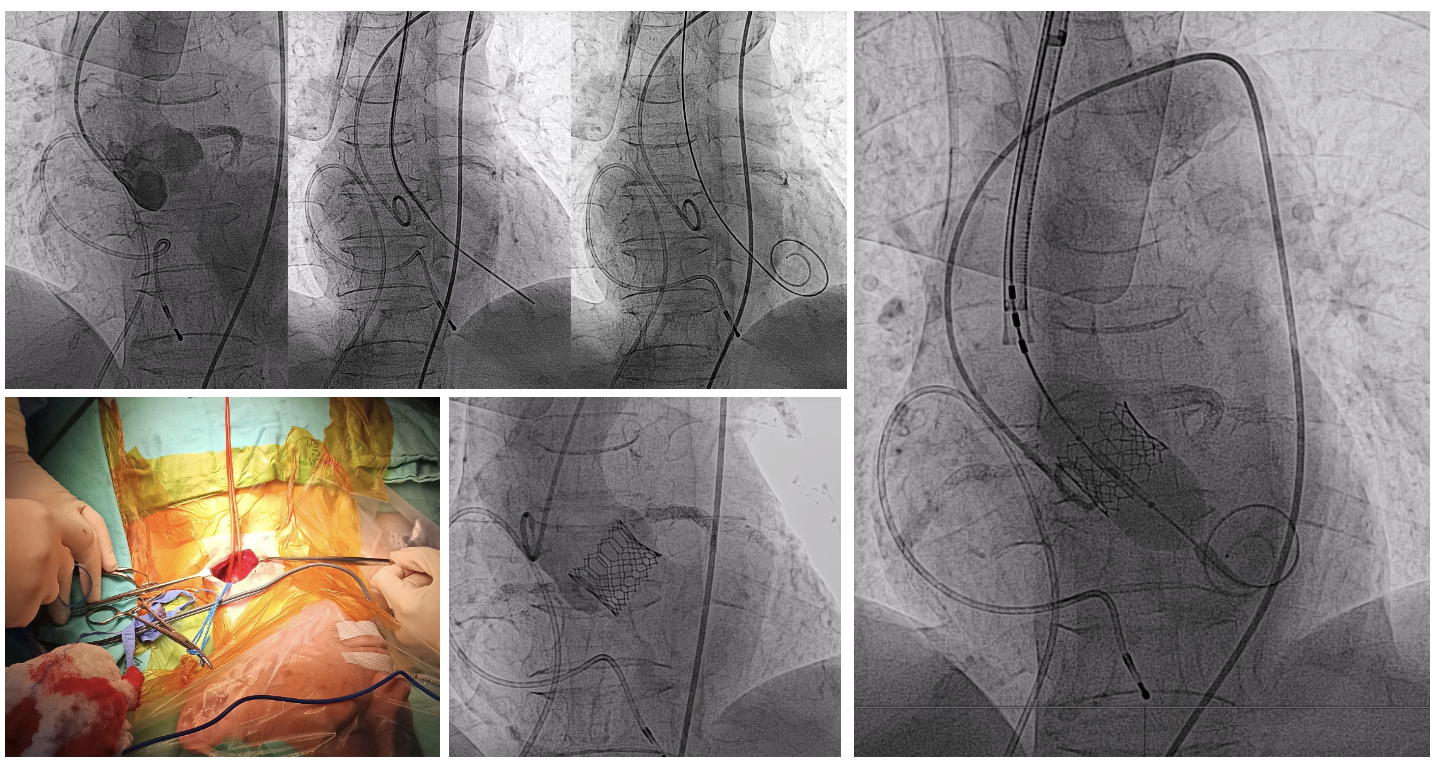
Right FA puncture was done, followed by left CAG, which showed a patent stent in the LM-LAD-LCx. 5F Pigtail catheter was introduced to the aortic sinus via the right femoral sheath, and an aortogram was performed. Coplanar and cusp overview adjustments were made due to the LAO position, hindering the left carotid approach from the operator. LV-Ao gradient measurement was omitted to shorten procedure time and reduce access sites. A temporary pacemaker was placed in the RV apex via the right FV.
Interventional Management
Procedural Step
The procedure began with an oblique incision at the left neck by a vascular surgeon for left carotid artery access via cut-down, with continuous brain saturation monitoring. A direct puncture of the left carotid artery was performed, and a 6F sheath was inserted. The aortic valve was crossed using a 6F AL1 catheter and a 0.035” straight wire, which was then exchanged for an ES Safari wire followed by the placement of a 14F E-Sheath. The Edwards Commander delivery system was used to navigate the valve across the proximal aortic arch and position it at the aortic valve under aortogram guidance. During rapid pacing, the valve's final position was confirmed, and an S3 valve (20 mm, nominal +0.5 ml) was deployed. Post-deployment assessment showed the valve in a stable position with properly functioning leaflets. Final aortogram revealed no contrast extravasation. TTE demonstrated trace PVL, no pericardial effusion, mean gradient of 8 mmHg. Vascular closure of the left carotid artery was achieved with soft tissue bleeding controlled by electrocautery. A final angiogram confirmed no extravasation or significant stenosis of the left carotid artery. The incision was closed with absorbable sutures, and a Jackson drain was placed. Femoral sheaths were removed, and hemostasis was obtained with manual compression. The patient was safely transferred to the post-procedural unit in stable condition and was discharged home within 2 days.
Case Summary
This case highlights the management of a frail 70-year-old female with low-gradient AS, moderate-to-severe MR, and TVD complicated by cardiogenic shock. Initially planned for CABG with DVR, she required urgent PCI to the LM bifurcation due to sudden deterioration. Post-PCI, her LVEF improved, MR reduced, but severe AS persisted. Given anatomical and access challenges, transcarotid TAVR was performed using a 20 mm Edwards S3 valve with excellent outcomes. The patient recovered well and was discharged, emphasizing the importance of tailored, multidisciplinary intervention in complex structural heart disease.


