Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-089
Long Diffuse RCA CTO With Ambiguous Proximal Cap and Distal Bifurcation Lesion at PDA and PLV Successfully Recanalized by Retrograde Approach
By Hou Tee Lu, Vicknesan Kulasingham, Kim Heng Shee, Sim Jian Hao, Lau Waye Young, Gurudevan Mahadevan
Presenter
Lau Waye Young
Authors
Hou Tee Lu1, Vicknesan Kulasingham1, Kim Heng Shee1, Sim Jian Hao1, Lau Waye Young1, Gurudevan Mahadevan1
Affiliation
Sultanah Aminah Hospital, Malaysia1,
View Study Report
TCTAP C-089
Coronary - Complex PCI - CTO
Long Diffuse RCA CTO With Ambiguous Proximal Cap and Distal Bifurcation Lesion at PDA and PLV Successfully Recanalized by Retrograde Approach
Hou Tee Lu1, Vicknesan Kulasingham1, Kim Heng Shee1, Sim Jian Hao1, Lau Waye Young1, Gurudevan Mahadevan1
Sultanah Aminah Hospital, Malaysia1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 71-year-old male was admitted to a district hospital for acute coronary syndrome and referred for further management. Risk factor was hypertension and diabetes mellitus. Non-smoker. The HR was 70/min and BP was 134/83 mmHg. He was on oral clopidogrel 75mg od, Cardiprin 100mgod, atovastatin 40mgod, perindopril 2mgod, bisoprolol 1.25mgod, and metformin 500 mg bd
Relevant Test Results Prior to Catheterization
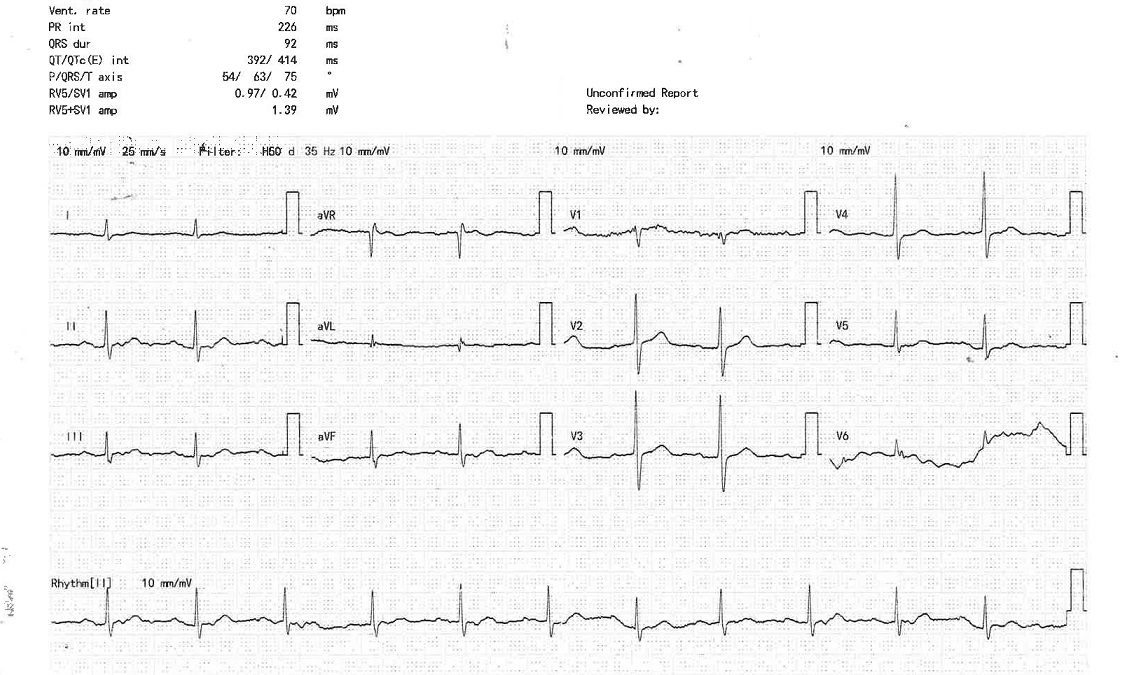
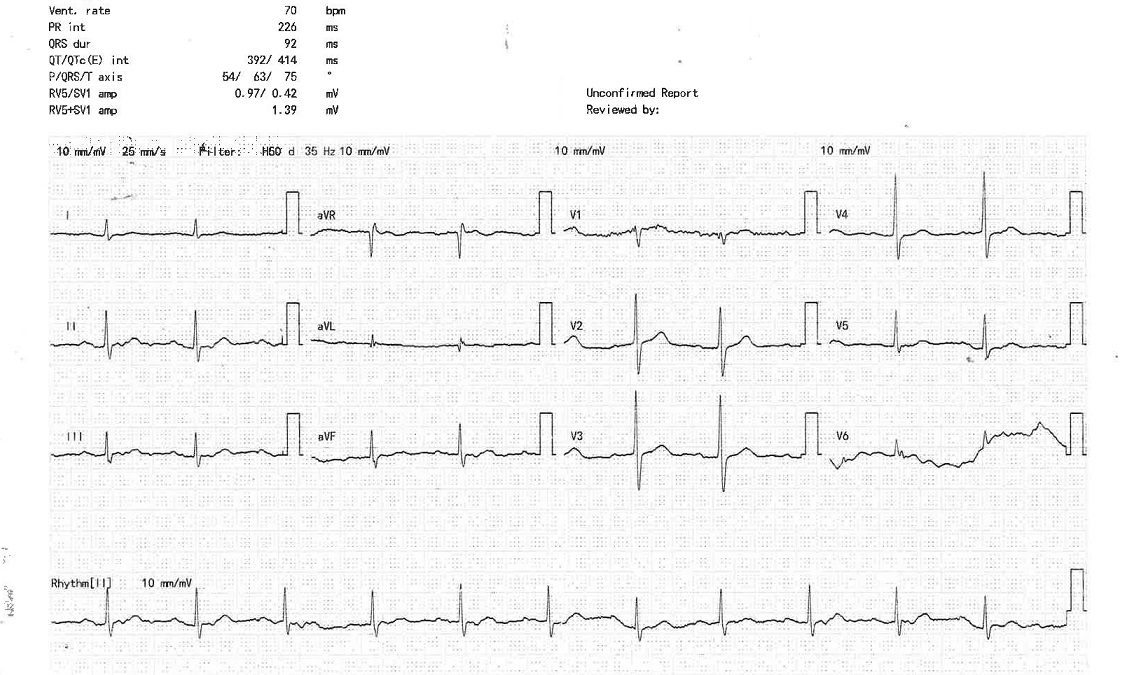
The baseline ECG was normal. The Trop-I: 394 ng/mL (high)
Exercise stress test was not feasible because of recent NSTEMI and joint pain.
Blood investigations: Hb: 14.1 g/dl ALT: 30 U/L, K: 2.9 mmol/l , LDL: 4.3 mmol/l, HbA1c: 8.0%, urea: 5.0 mmol/l Na: 139 mmol/l Creatine: 99 umol/l
CXR had minimal right lower zone haziness
The echocardiography showed good LVEF of 63%. Normal chambers and valves. No RWMA.
Exercise stress test was not feasible because of recent NSTEMI and joint pain.
Blood investigations: Hb: 14.1 g/dl ALT: 30 U/L, K: 2.9 mmol/l , LDL: 4.3 mmol/l, HbA1c: 8.0%, urea: 5.0 mmol/l Na: 139 mmol/l Creatine: 99 umol/l
CXR had minimal right lower zone haziness
The echocardiography showed good LVEF of 63%. Normal chambers and valves. No RWMA.
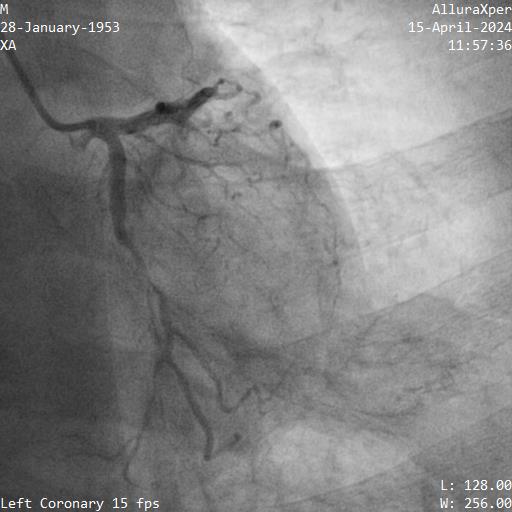
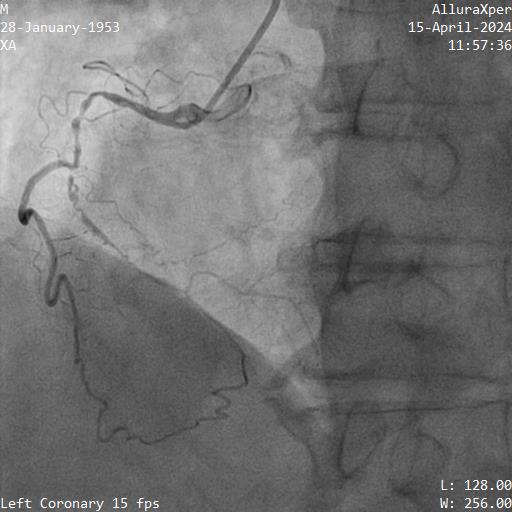
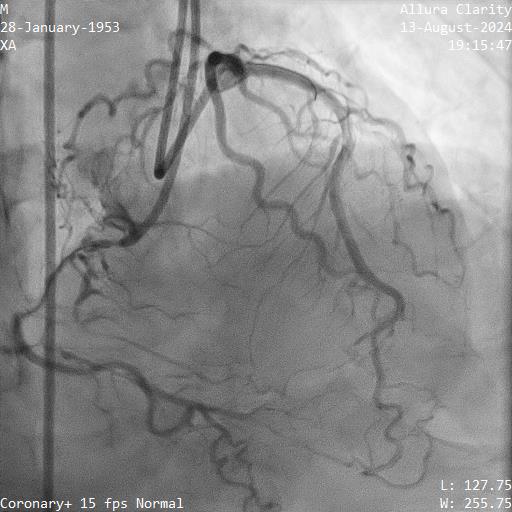
Relevant Catheterization Findings
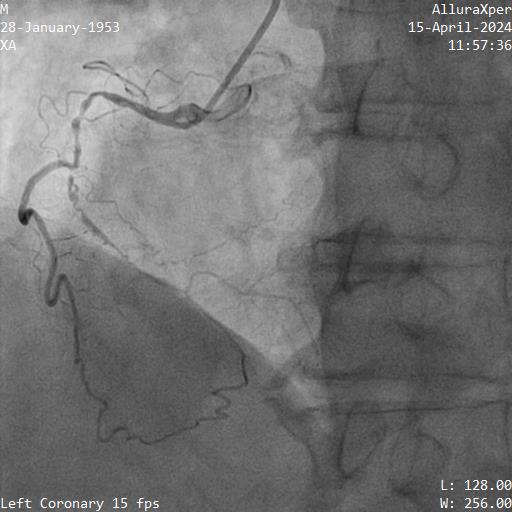
1. LMT was normal
2. Proximal LAD had a 70-80% stenosis, mid LAD had myocardial bridging. LAD supplied septal collateral (CC) to distal PDA
3. Proximal LCX artery had a 90% stenosis
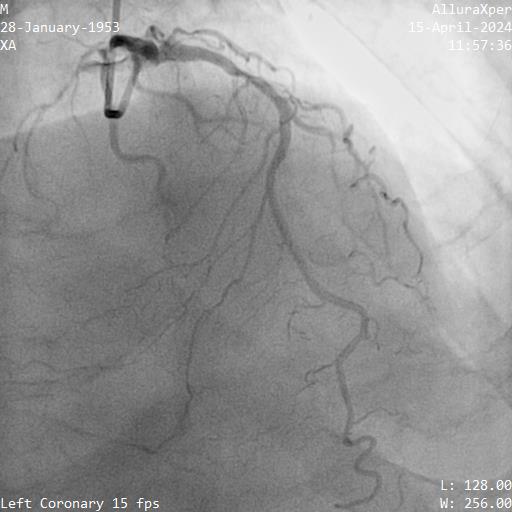
4. Proximal RCA was diffuse disease 70-80%, mid to distal RCA was a CTO. Ipsilateral CC from marginal to PDA
SYNTAX I score: 28 CABG was offered but patient declined.
PCI was performed for LCX with biolimus eluting stent (BES) 2.5x30mm and LAD with BES 3.0x29mm
He was scheduled for stage PCI RCA CTO 2 months later.
2. Proximal LAD had a 70-80% stenosis, mid LAD had myocardial bridging. LAD supplied septal collateral (CC) to distal PDA
3. Proximal LCX artery had a 90% stenosis
4. Proximal RCA was diffuse disease 70-80%, mid to distal RCA was a CTO. Ipsilateral CC from marginal to PDA
SYNTAX I score: 28 CABG was offered but patient declined.
PCI was performed for LCX with biolimus eluting stent (BES) 2.5x30mm and LAD with BES 3.0x29mm
He was scheduled for stage PCI RCA CTO 2 months later.
Interventional Management
Procedural Step
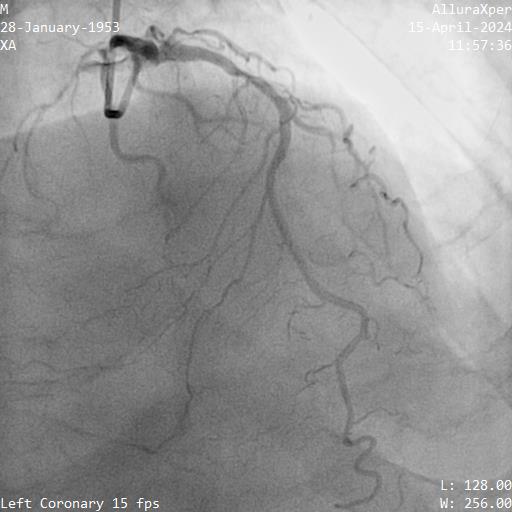
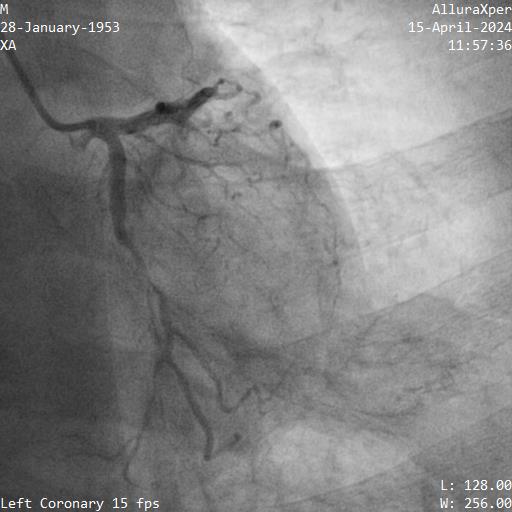
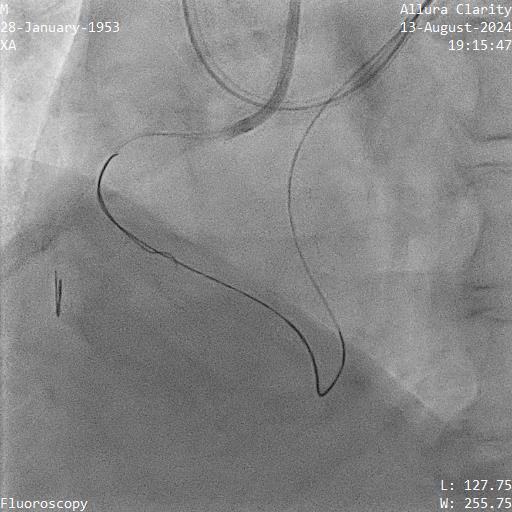
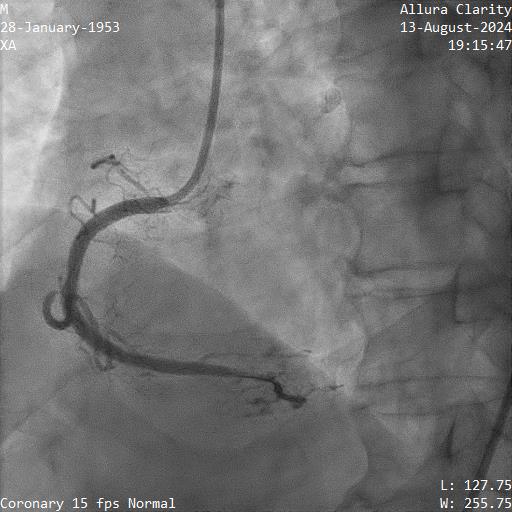
Right femoral and right radial arteries were punctured. A 7Fr EBU 3.5 guiding catheter (GC) was used to engage LMT. A 7Fr JR 4 GC was used for RCA CTO PCI. For antegrade preparation, a wire was delivered into right marginal artery. For antegrade proximal cap puncture, a Finecross microcatheter (MC) and Fielder XTR was used to wire into mid RCA CTO, but XTR fail to advance further. For retrograde approach, a CorsairPro ES (150 cm) MC, SION and SUOH 03 wire were used for LAD septal wiring but failed. A Sion Black with 90 degree tip successfully negotiate the collateral and entered PDA. The distal cap was hard to puncture. UB3 was used to puncture the distal cap and managed to cross and externalized into antegrade GC. Attempt was made to advance retrograde MC but failed at the point of PDA/PLV bifurcation.
Next plan was using retrograde UB3 to tip in antegrade MC successfully. However, the antegrade MC crossed the CTO body but failed cross PDA despite anchoring balloon at marginal artery. Next, switched to antegrade, escalated the antegrade wire to GAIA Next2 and using retrograde wire as a marker to facilitate antegrade wiring. Fortunately, the GAIA Next 2 managed to entered PLV. IVUS confirmed wire in true lumen after predilatation. The PDA was wired using CRUSADE MC to keep wire access for PDA and PLV.Distal RCA-PDA stented with everolimus eluting stent (EES) 2.5x32mm, mid RCA EES 3.5x32mm, and ostial RCA EES 4.0x24mm, post dilated NC 3.0x15mm, and 4.0x15mm balloon.
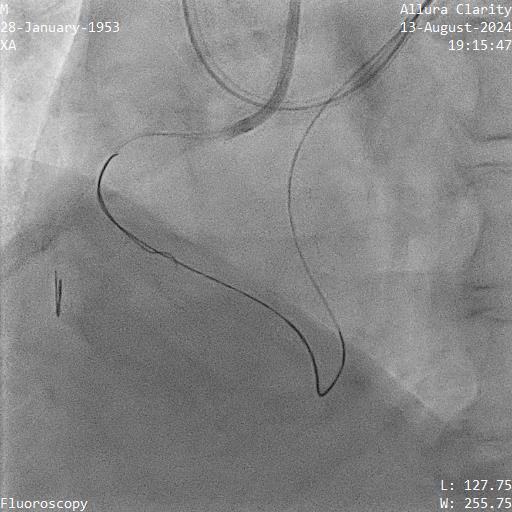
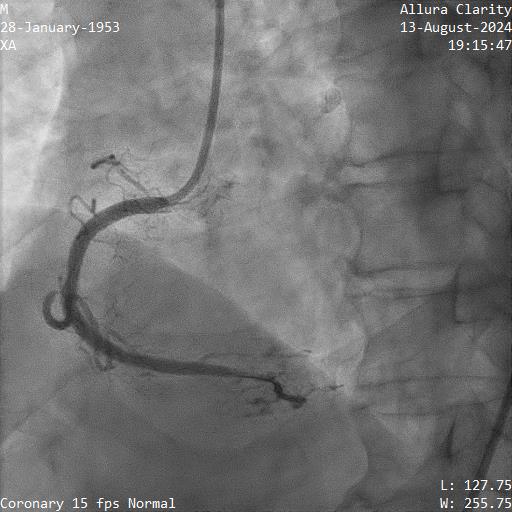
Next plan was using retrograde UB3 to tip in antegrade MC successfully. However, the antegrade MC crossed the CTO body but failed cross PDA despite anchoring balloon at marginal artery. Next, switched to antegrade, escalated the antegrade wire to GAIA Next2 and using retrograde wire as a marker to facilitate antegrade wiring. Fortunately, the GAIA Next 2 managed to entered PLV. IVUS confirmed wire in true lumen after predilatation. The PDA was wired using CRUSADE MC to keep wire access for PDA and PLV.Distal RCA-PDA stented with everolimus eluting stent (EES) 2.5x32mm, mid RCA EES 3.5x32mm, and ostial RCA EES 4.0x24mm, post dilated NC 3.0x15mm, and 4.0x15mm balloon.
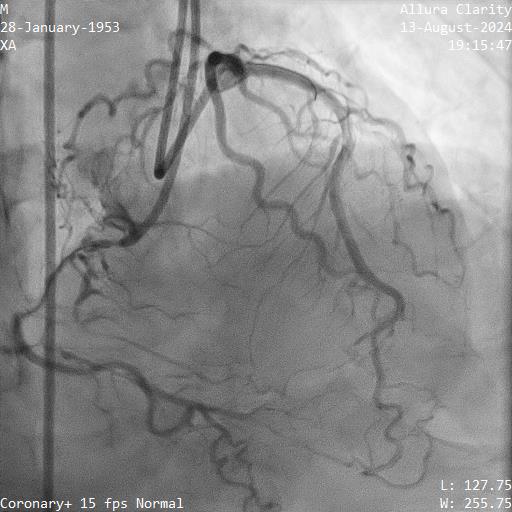
Case Summary
CTO with ambiguous proximal cap is challenging due to the difficulty of locating a suitable entry point. It is important to apply a step-wise hybrid CTO algorithm in order to select the best option suited to the patient. Our case also highlighted that IVUS is an essential tool in CTO PCI. Negative remodeling in vessel with CTO is common, therefore angiographic assessment may underestimate the true vessel size results in undersized stent and poor long term outcome.


