Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-064
Heavily Calcified CTO RCA, Rotational Atherectomy in Last Remaining Vessel
By Vimean Sey, Doni Firman, Amir Aziz Alkatiri, Chinh Liv
Presenter
Vimean Sey
Authors
Vimean Sey1, Doni Firman2, Amir Aziz Alkatiri2, Chinh Liv3
Affiliation
Cambodia-China Friendship Preah Kossmak Hospital, Cambodia1, National Cardiovascular Center, Indonesia2, Calmette Hospital, Cambodia3,
View Study Report
TCTAP C-064
Coronary - Complex PCI - Calcified Lesion
Heavily Calcified CTO RCA, Rotational Atherectomy in Last Remaining Vessel
Vimean Sey1, Doni Firman2, Amir Aziz Alkatiri2, Chinh Liv3
Cambodia-China Friendship Preah Kossmak Hospital, Cambodia1, National Cardiovascular Center, Indonesia2, Calmette Hospital, Cambodia3,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 59 years old male who had past medical history of diabetes mellitus, hypertension, and bilateral lung fibrosis. He’s presented to the emergency department due to progressively worsening effort angina and dyspnea on exertion. He had been hospitalized multiple times for the past 3 months due to the same reason despite optimal medical treatment.
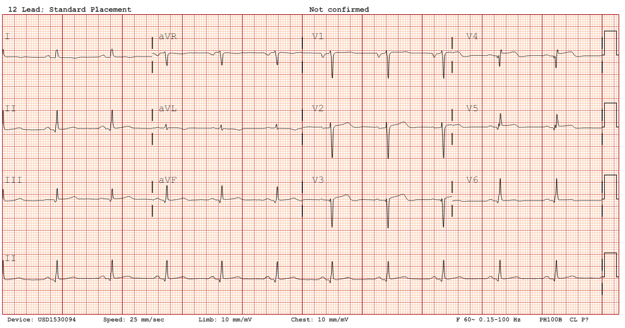
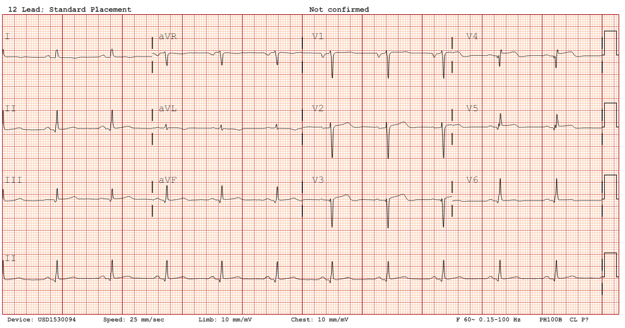
Relevant Test Results Prior to Catheterization
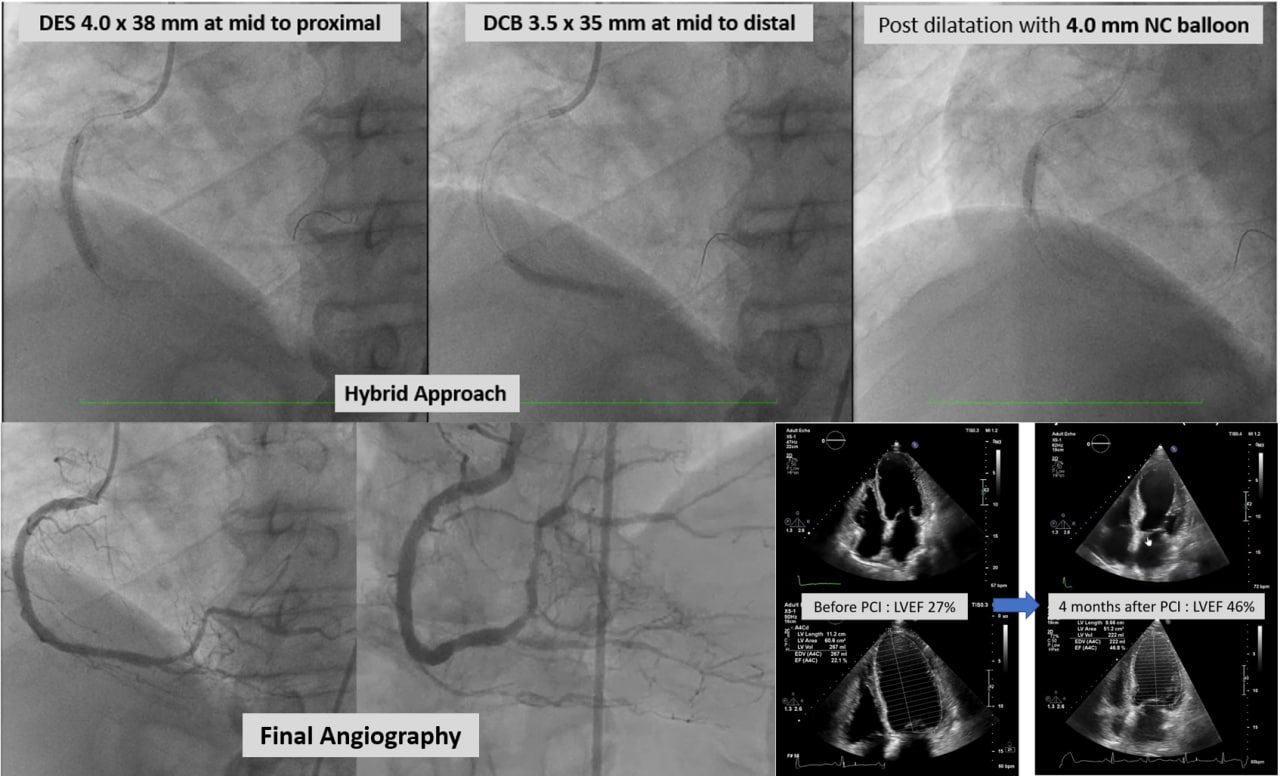
Echocardiography showed a reduced left ventricular systolic function with an ejection fraction of 27%. Cardiac biomarker - Troponin I test was negative at presentation. Rest of the laboratory parameters were within normal limit.
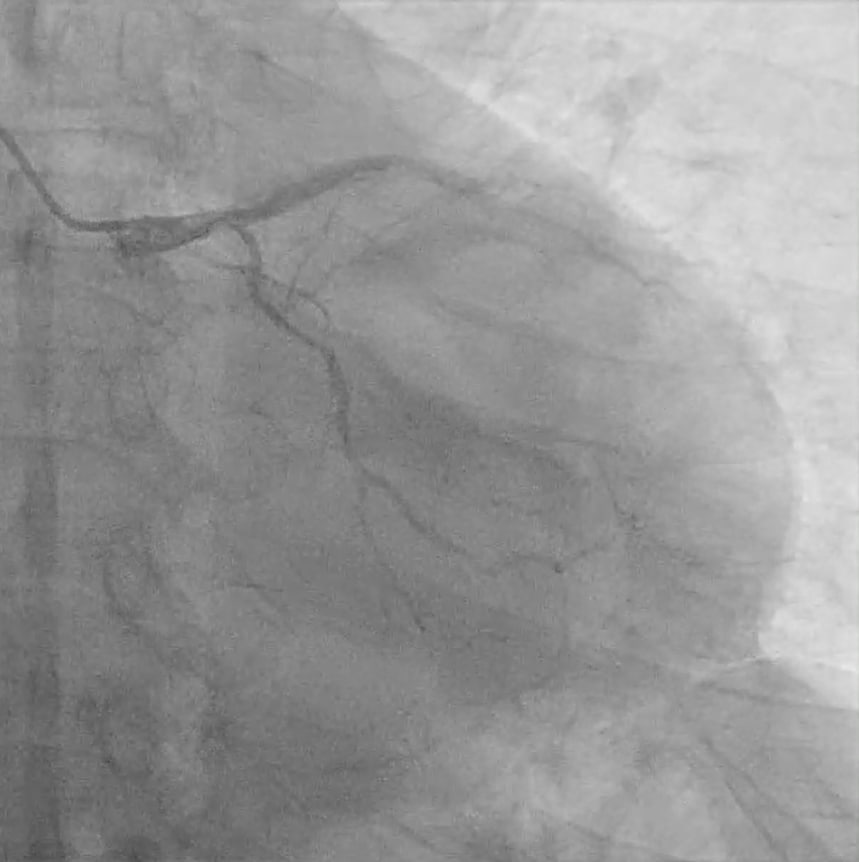
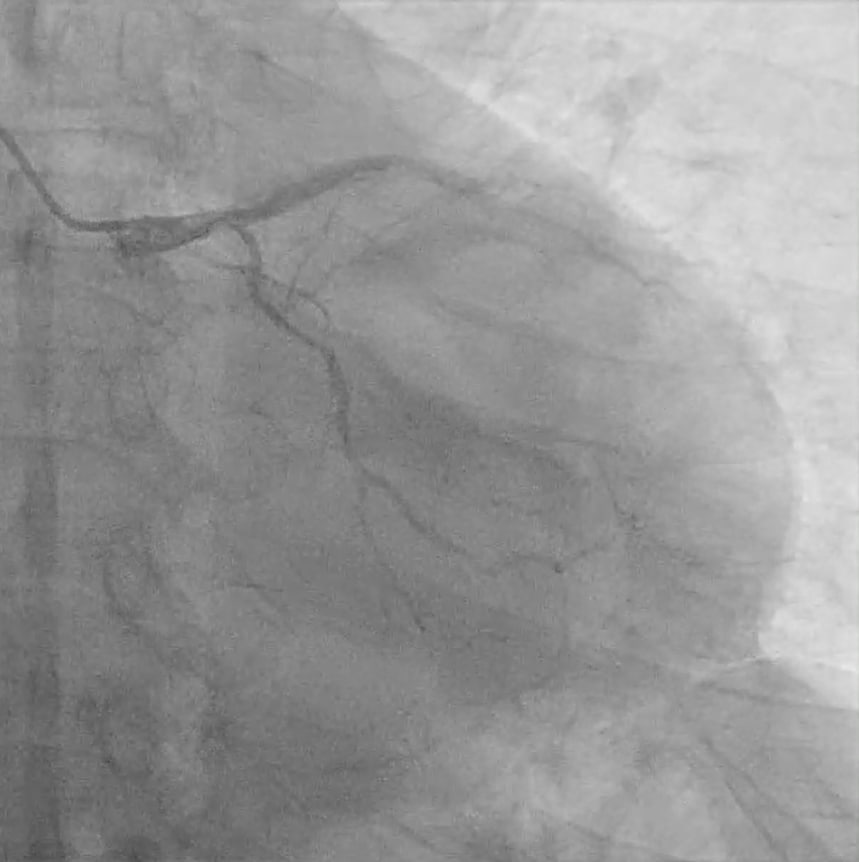
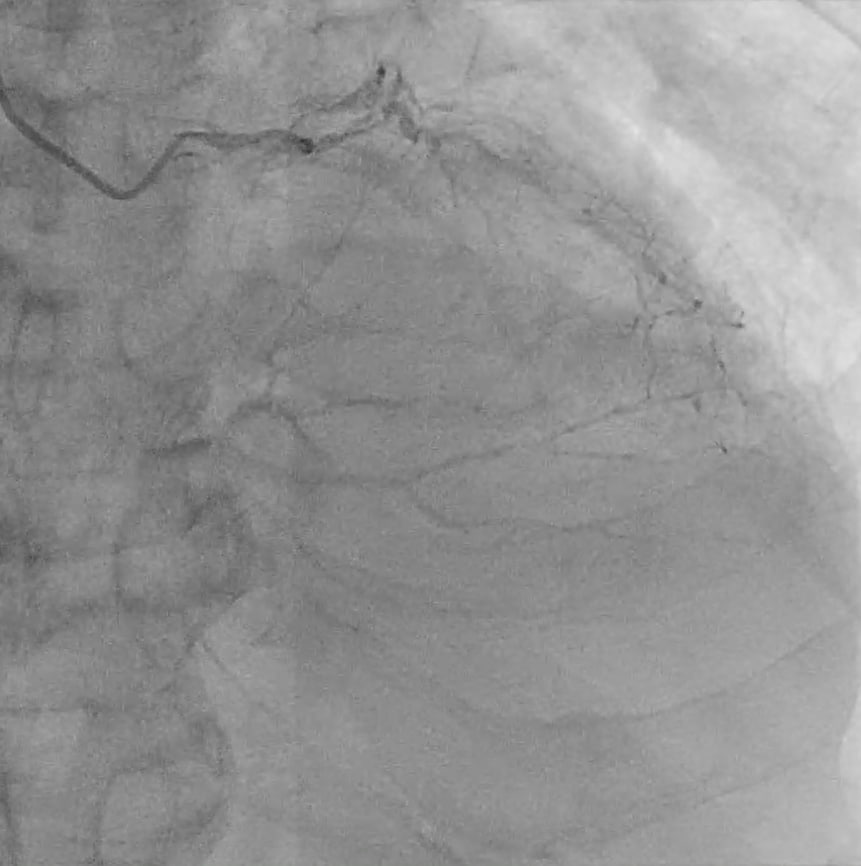
Relevant Catheterization Findings
Coronary angiography revealed chronic total occlusion (CTO)of proximal left anterior descending (LAD) and right coronary artery (RCA),non-dominant left circumflex (LCX) with diffuses disease in proximal. Viability study (CMRI) after heart team discussion showed Ischemic cardiomyopathy without viability at partial LAD. Due to high surgical risk (bilateral lung fibrosis)and non-viable LAD territory, CABG was declined by the surgeon. PCI CTO RCA was planned.


Interventional Management
Procedural Step
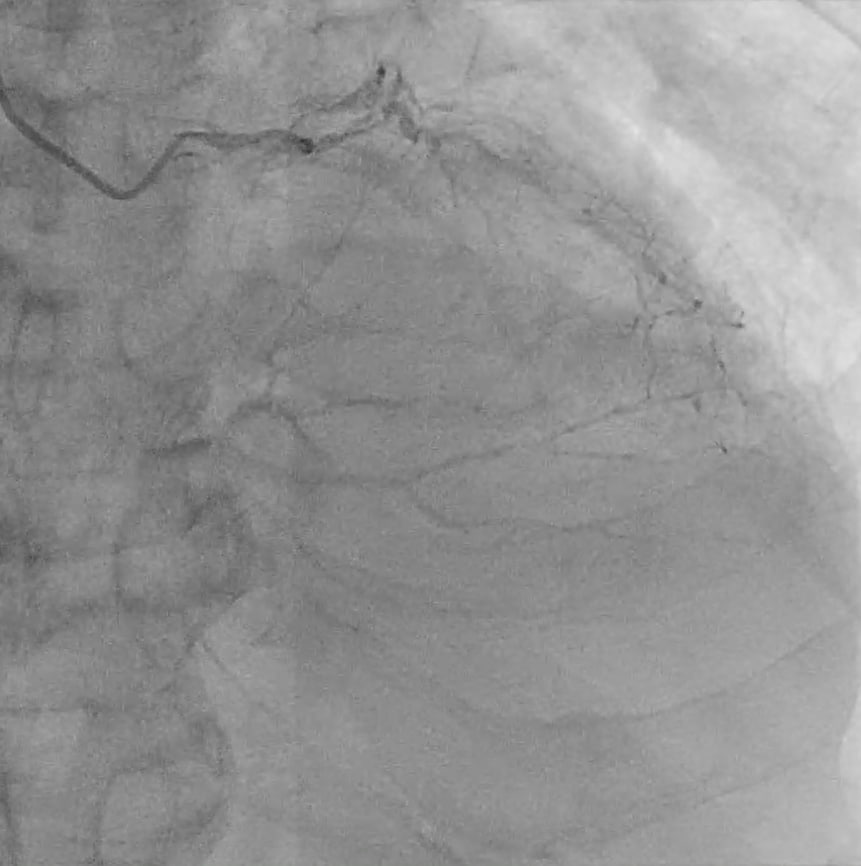
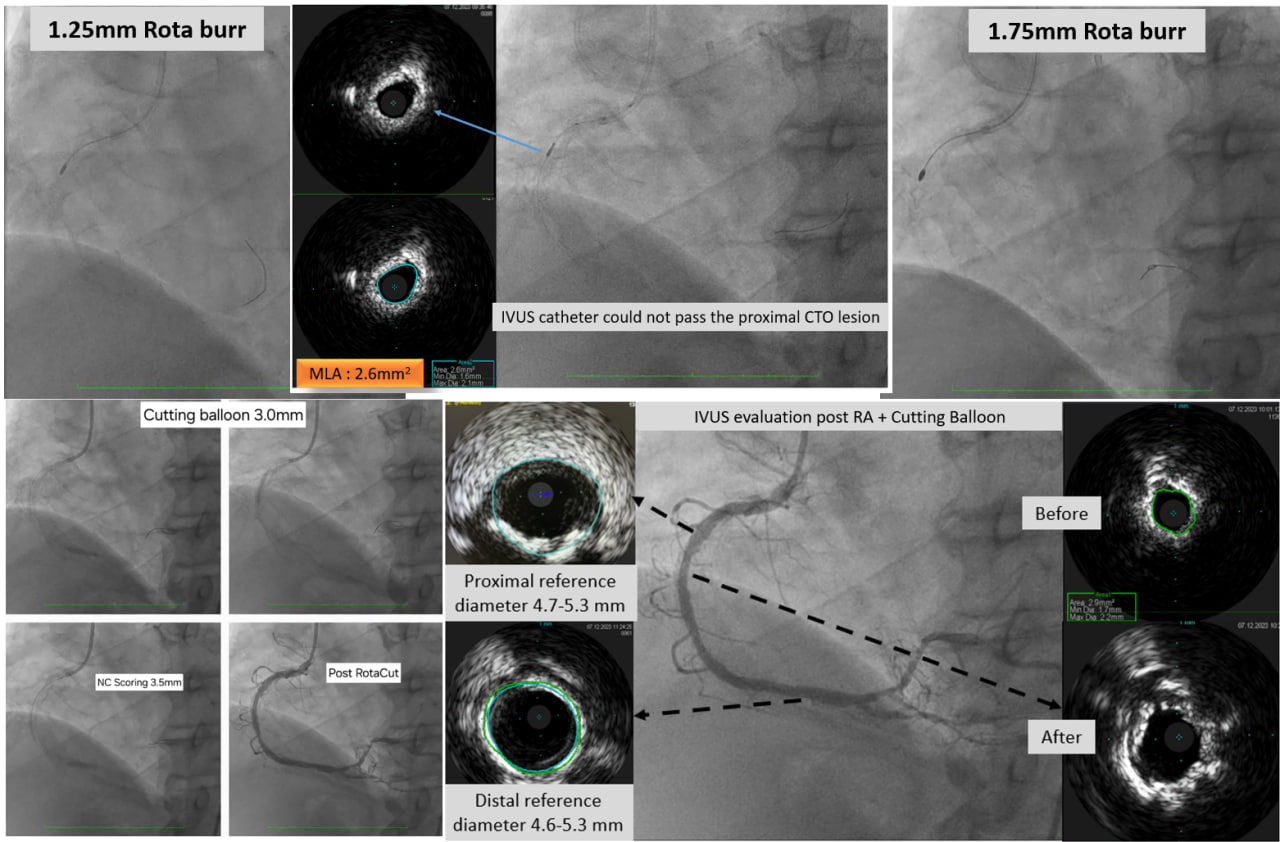
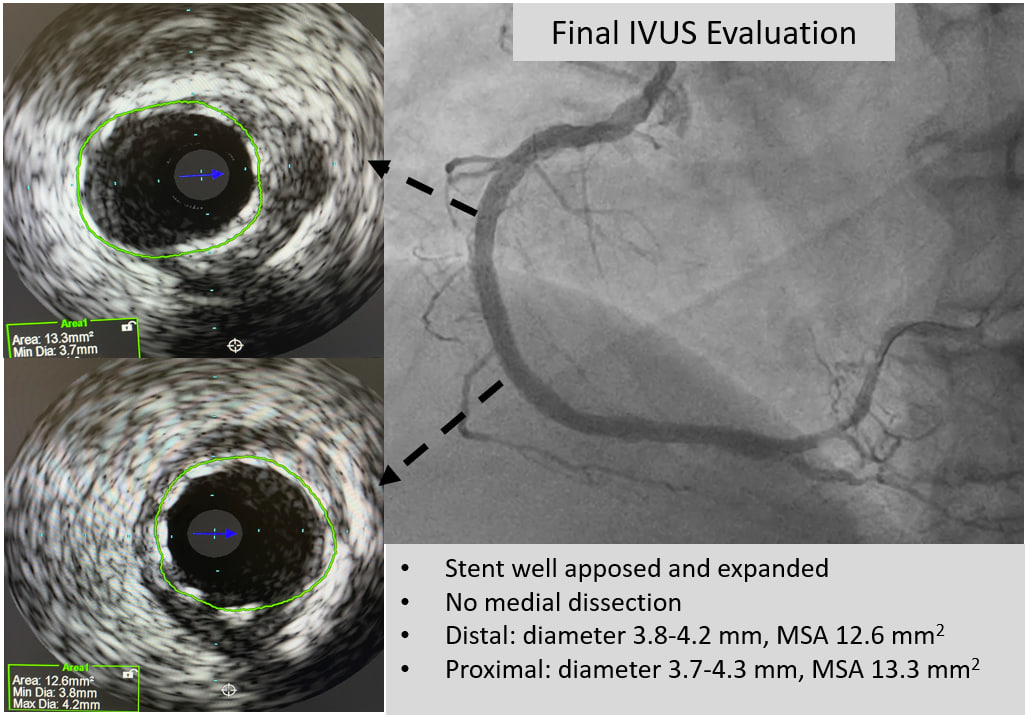
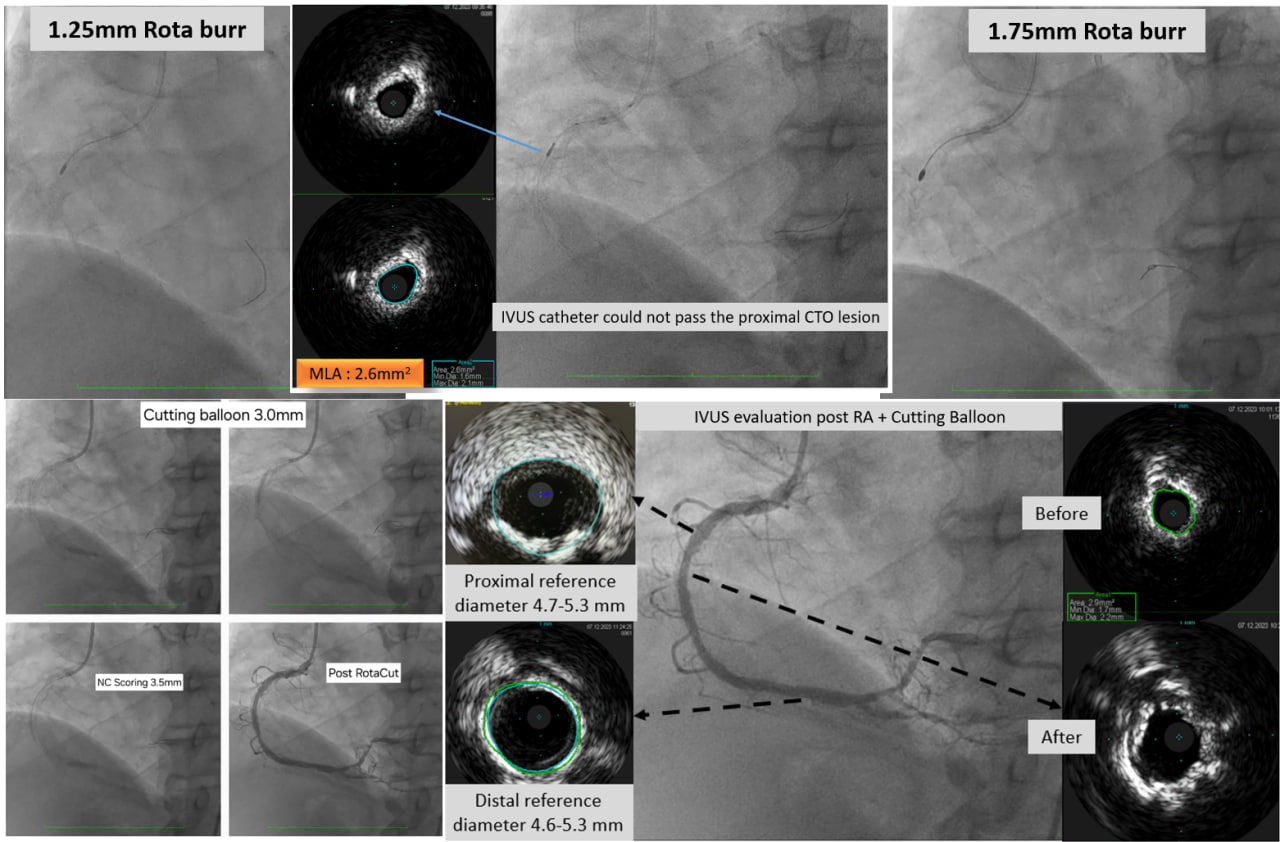
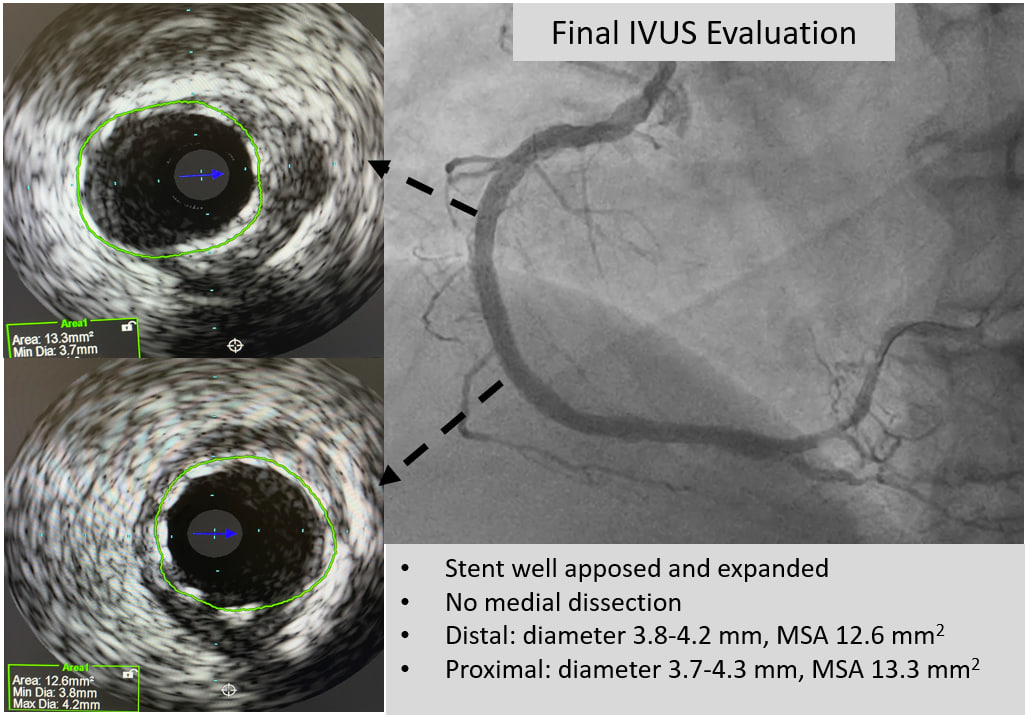
Dual injection with antegrade approach was chosen as primary strategy. Despite the use of Fielder XTA guidewire supported by Finecross 130 cm, the lesion was not crossed. Wire escalation to Gaia 2 was successfully crossed the lesion. However, Finecross and 1.25 mm semicompliant (SC) balloon could not pass the CTO lesion. Guidezilla 6F facilitate 1.0 mm SC balloon crossed the CTO lesion. After predilatation with 1.0 mm SC balloon, we were able to advance the microcatheter beyond the distal cap of the occlusion and perform rotational atherectomy with 1.25 mm burr size. IVUS Catheter could not pass CTO lesion. Segmental IVUS evaluation was performed and showed 360o superficial calcium with MLA 2.6 mm2. Rotational atherectomy with bigger burr size to 1.75 mm was performed. IVUS evaluation showed 180o-360o superficial calcium and MLA 2,6 mm2. Proximal reference diameter (lumen) 4.7-5.3 mm, mean vessel area 19.4 mm2. Distal reference diameter (EEM) 4.6-5.3 mm, mean vessel area 18.9 mm2. Lesion preparation was continued with 3.0 x 15 mm Cutting Balloon (Wolverine) from distal to proximal followed by 3.5 x 15 mm NC Scoring Balloon. Calcium cracks and Reverberations were detected by IVUS evaluation in multiple part of RCA. The lesion was treated with hybrid approach (Drug Coated Balloon 3.5 x 35 mm at mid to distal part and Drug Eluting Stent 4.0 x 38 mm at mid to proximal part). Post dilatation was done with 4.0 mm NC balloon with an excellent angiographic result.
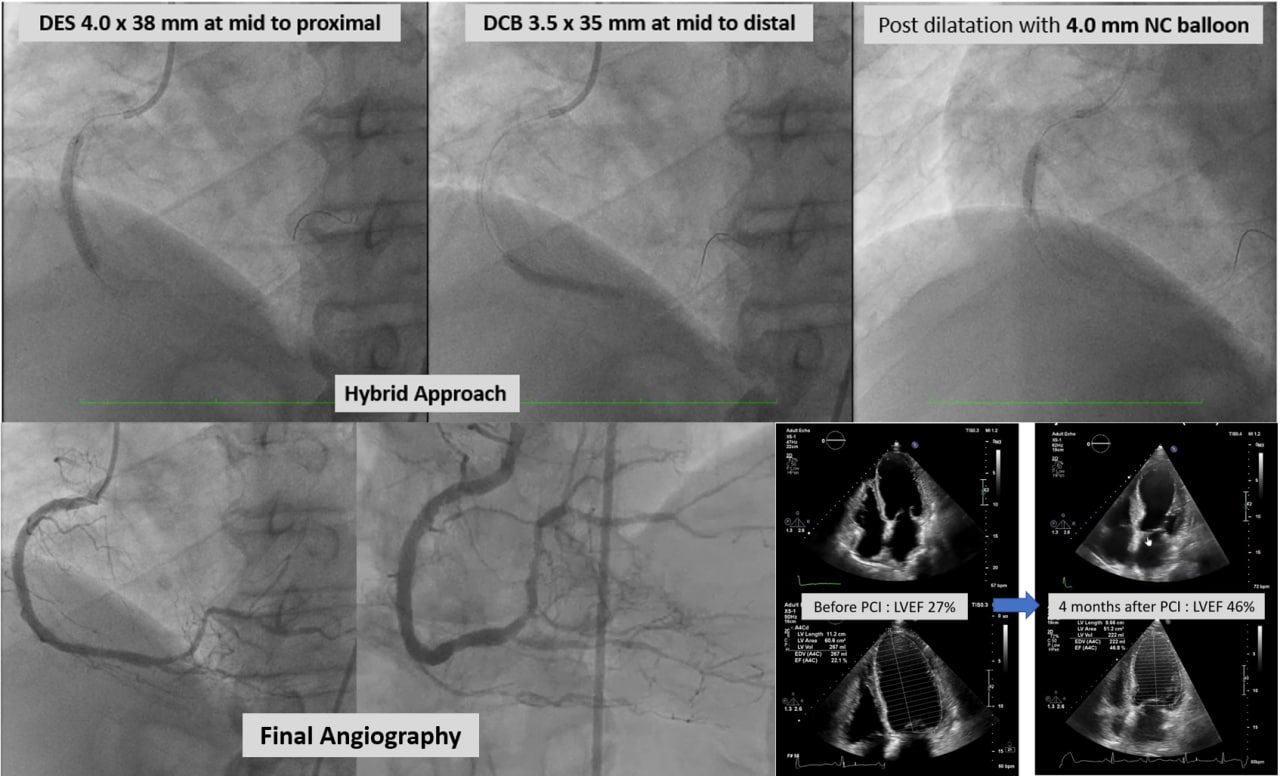
Case Summary
The burr is downsized initially for better penetration force and upsized the burr finally for better contact to the calcification within the lesion. Small burrs and low speeds, Intermittent runs with continuous flush solution, Optimal antiplatelet and antithrombotic regimen are keys factor for better outcome.


