Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-130
Caught in the Act: The Hidden Dangers of Cannulation-Induced Coronary Dissection
By Fawzia Arifin Daud, Arwin Saleh Mangkuanom, Doni Firman, Nanda Iryuza, Amir Aziz Alkatiri
Presenter
Fawzia Arifin Daud
Authors
Fawzia Arifin Daud1, Arwin Saleh Mangkuanom1, Doni Firman1, Nanda Iryuza1, Amir Aziz Alkatiri1
Affiliation
National Cardiovascular Center, Indonesia1,
View Study Report
TCTAP C-130
Coronary - Complication Management
Caught in the Act: The Hidden Dangers of Cannulation-Induced Coronary Dissection
Fawzia Arifin Daud1, Arwin Saleh Mangkuanom1, Doni Firman1, Nanda Iryuza1, Amir Aziz Alkatiri1
National Cardiovascular Center, Indonesia1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 67-year-old woman presents with complaint of chest pain during light activities. She had a history of hypertension and is currently undergoing treatment. A coronary CT scan was performed, revealing moderate to severe stenosis at proximal LAD and proximal RCA.
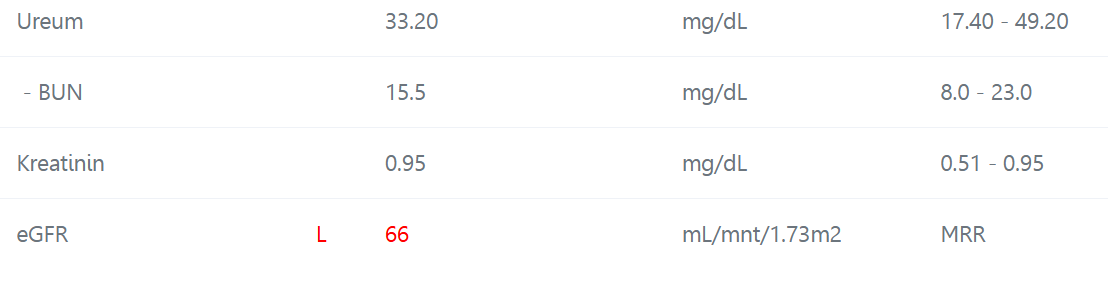
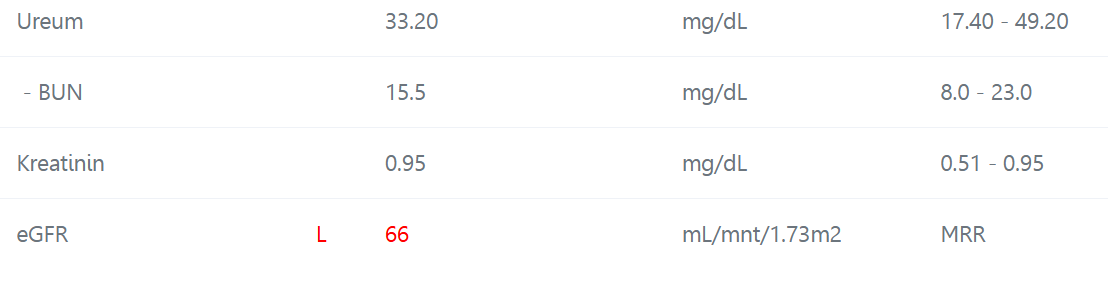
Relevant Test Results Prior to Catheterization
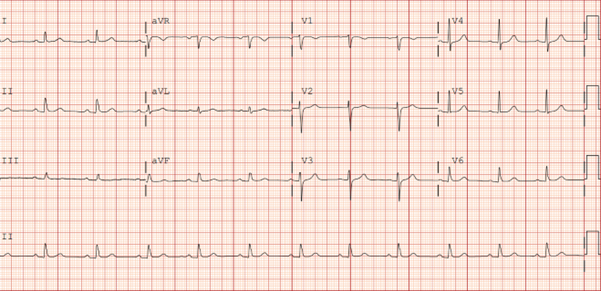
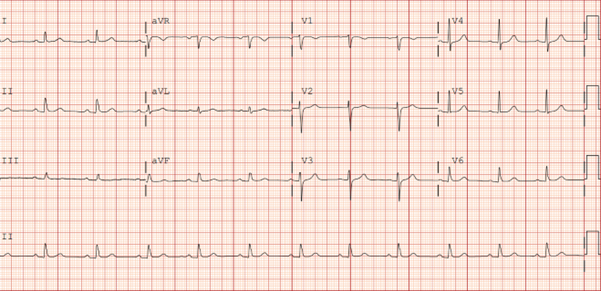
The electrocardiogram prior to catheterization procedure demonstrated normal sinus rhythm. Laboratory test result showed mild renal insufficiency (eGFR 62ml/min), others were unremarkable.
Relevant Catheterization Findings
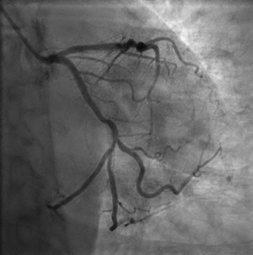
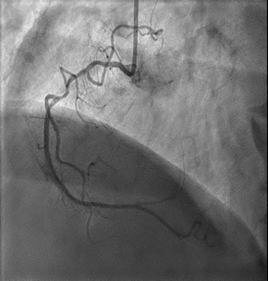
The diagnostic angiography one month after MSCT, showed calcification at LM without significant stenosis. Calcified and diffusely stenosis LAD ranging from 70-80% in the proximal segment. LCX is dominant, but only non-significantly stenosis, and the RCA is 50-60% stenosis at proximal. Hence, we planned for PCI of LAD.


Interventional Management
Procedural Step
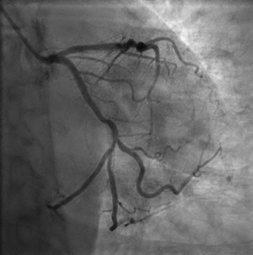
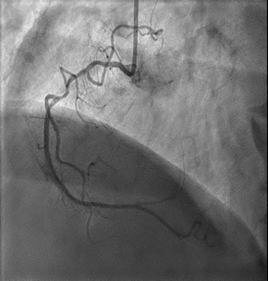
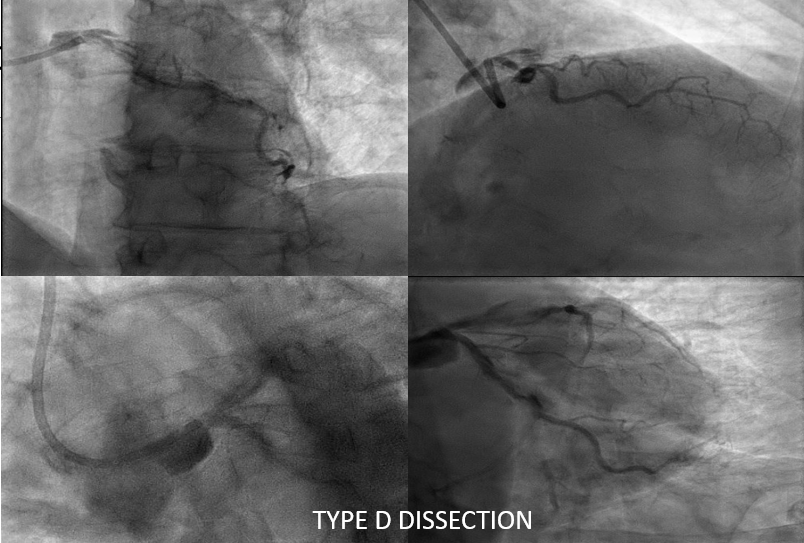
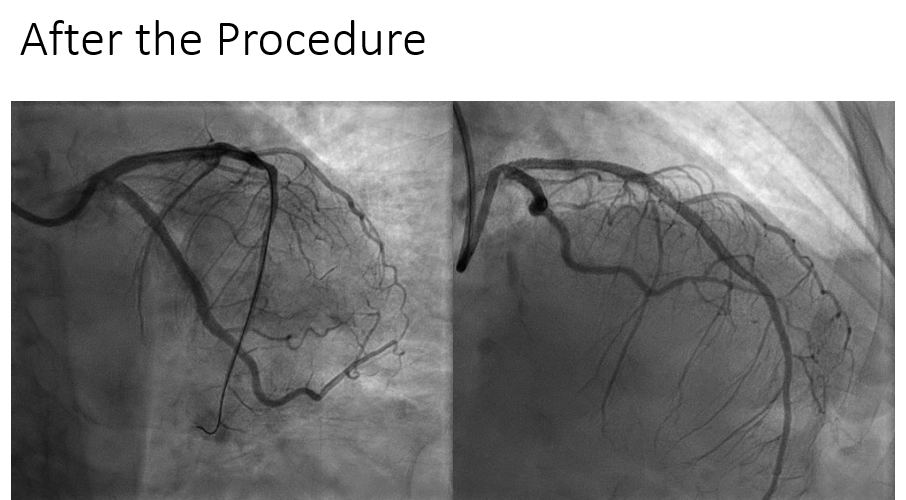
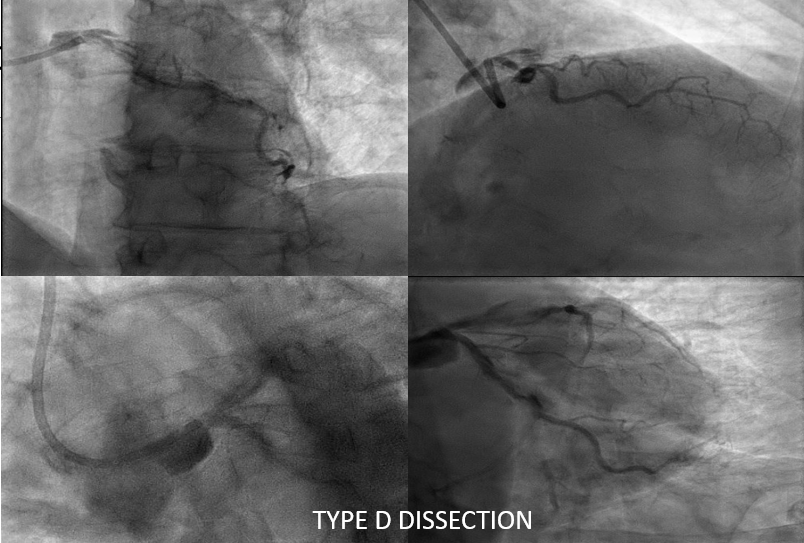
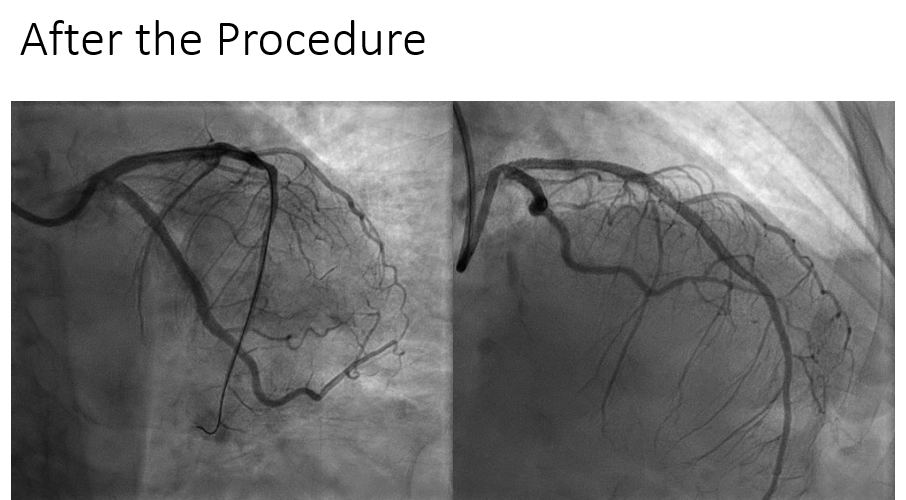
In our procedure, we initiated left coronary artery (LCA) cannulation using a Guiding Catheter XB 3.0/6F and captured several cine images. It was then that we detected a type D dissection extending from the proximal to distal segments of the left anterior descending artery (LAD) and left circumflex artery (LCX), which unfortunately progressed to involve the left main and aorta. The patient subsequently experienced severe chest heaviness and hemodynamic instability. We quickly disengaged the guiding catheter and stabilized the patient's condition with an intravenous vasopressor drip. Re-cannulation was performed using a GC JL 3.5/6F to address the LCA while preventing further dissection progression. Initial wiring with a workhorse wire successfully crossed the lesion to the distal obtuse marginal artery (OM2), but we needed to switch to a Polymer Jacketed wire to navigate through the dissected proximal LAD. After successfully positioning the wire in the distal LAD, we conducted predilatation with a scoring balloon 3.0 x 15 mm in both the proximal LCX and proximal-osteal LAD regions. We deployed drug-eluting stents (DES) at critical sites, including a 3.0 x 38 mm stent in the proximal LCX-OM2 segment and a 3.5 x 38 mm stent at the osteal left main-proximal LAD, utilizing flare techniques and post-dilatation with a 4.0 x10 mm non-compliant balloon. The final angiography showed TIMI III flow, confirming that the dissection was sealed with no thrombus formation observed.
Case Summary
Iatrogenic coronary dissection during catheterization is a serious issue often occurring with junior operators. Excessive guiding catheter manipulation can lead to compromised coronary blood flow due to pre-existing arterial disease or poor technique. Balloon angioplasty or stenting may be necessary for immediate restoration of blood flow and prevention of ischemia. Post-procedure monitoring is crucial to detect complications like thrombosis or re-dissection. Prompt recognition and skilled management significantly improve patient outcomes, emphasizing the importance of vigilance during procedures.


