Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-190
In-Out-In: Labyrinth Traversed in Acute Coronary Syndrome
By Monika Bhandari, Akshyaya Pradhan, Pravesh Vishwakarma, Abhishek Singh, Rishi Sethi
Presenter
Monika Bhandari
Authors
Monika Bhandari1, Akshyaya Pradhan1, Pravesh Vishwakarma1, Abhishek Singh1, Rishi Sethi1
Affiliation
King George's Medical University, India1,
View Study Report
TCTAP C-190
Coronary - Imaging & Physiology - Invasive Imaging (IVUS, OCT, NIRS, VH, etc)
In-Out-In: Labyrinth Traversed in Acute Coronary Syndrome
Monika Bhandari1, Akshyaya Pradhan1, Pravesh Vishwakarma1, Abhishek Singh1, Rishi Sethi1
King George's Medical University, India1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 38-year-old woman presented with chest pain that had been ongoing for 20 hours. After assessment, she was found to have ST elevation anterior wall myocardial infarction. The patient had no history of diabetes mellitus, hypertension, and other conventional risk factors.The general examination and cardiovascular examination was within normal limits. The blood pressure was 112/70 mmHg with heart rate. The chest was clear and S1& S2 were normally heard with no added sounds or murmur.
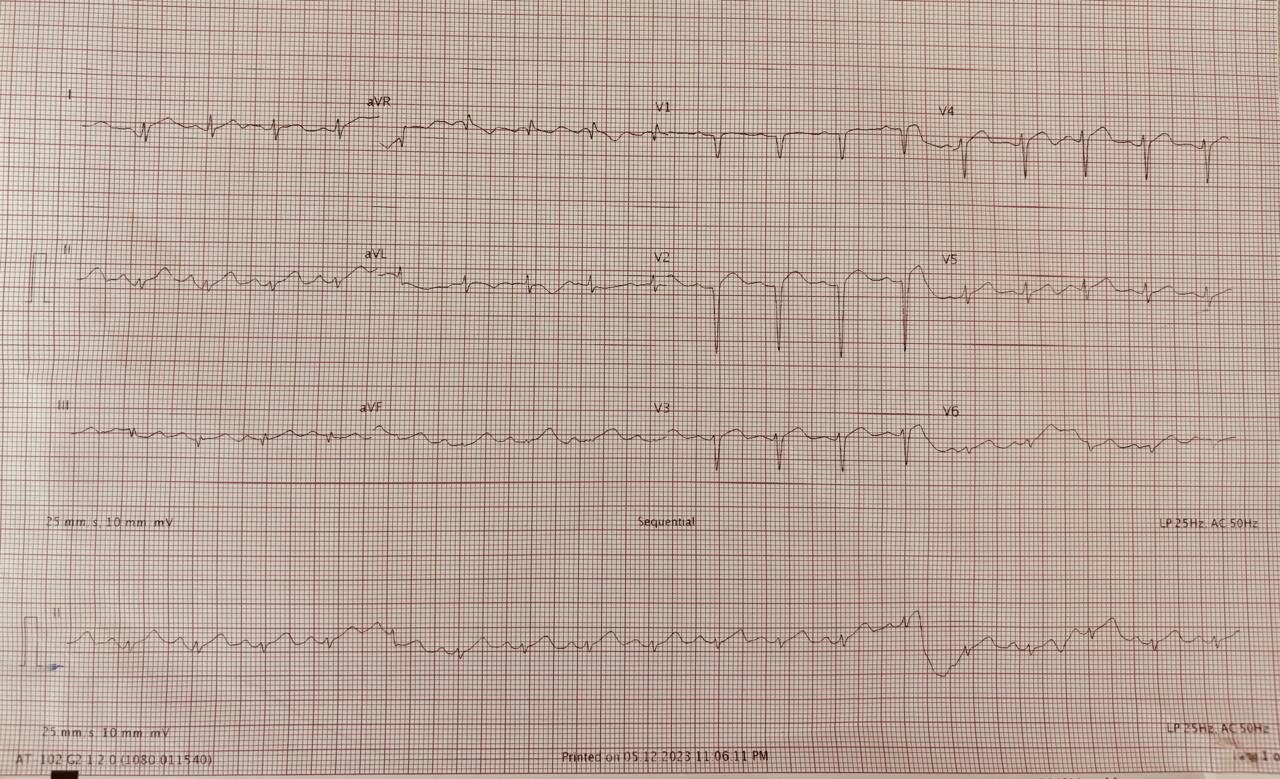
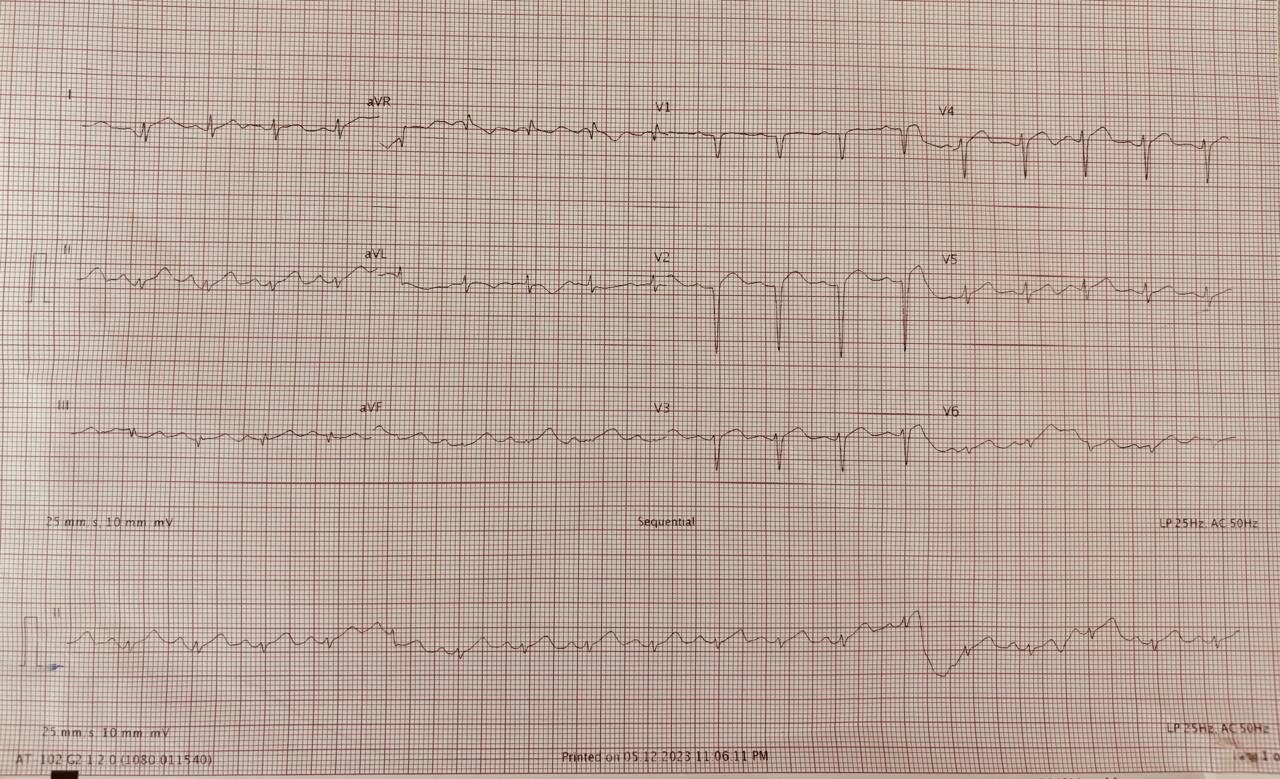
Relevant Test Results Prior to Catheterization
A transthoracic echocardiogram revealed segmental wall motion abnormalities in the apical septal, apical, and apical lateral wall of the left ventricle with an ejection fraction of 45%. Her cardiac biomarker (Troponin-I) levels were raised, and other blood parameters were normal. As a next step, she was scheduled for a coronary angiogram through the right radial route.
Relevant Catheterization Findings
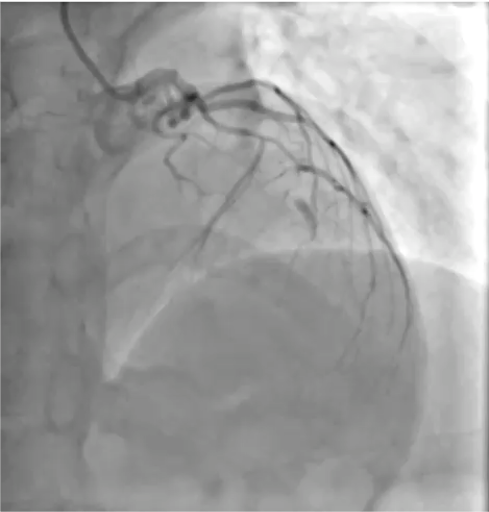
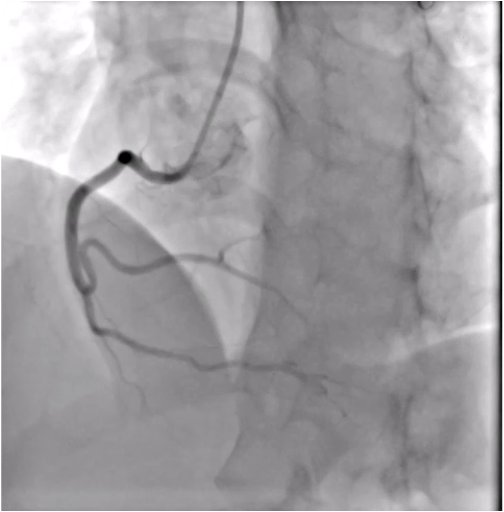
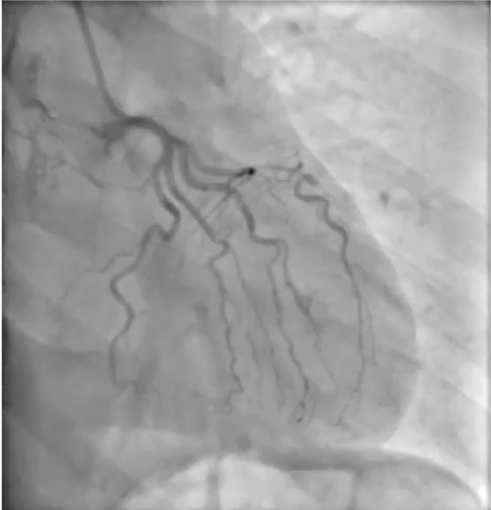
Angiography was planned through right radial route. A 6 french access sheath was introduced into radial artery. After that 5 french Tiger catheter was taken to engage left and right coronary artery. The coronary angiogram revealed that the left anterior descending (LAD) coronary artery was 100% occluded after the origin of the first diagonal and left cirumflex (LCX) and right coronary artery were normal. Patient planned for primary PCI of LAD.
Interventional Management
Procedural Step
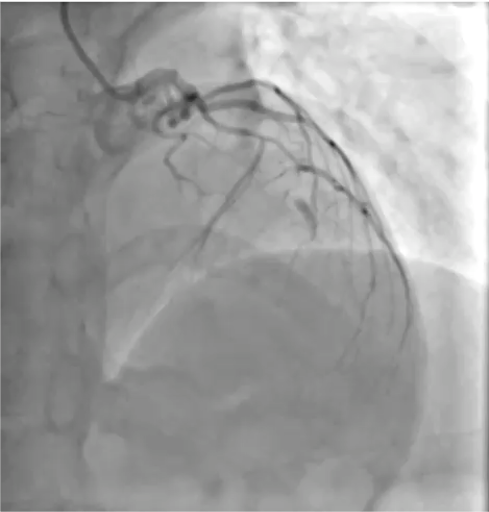
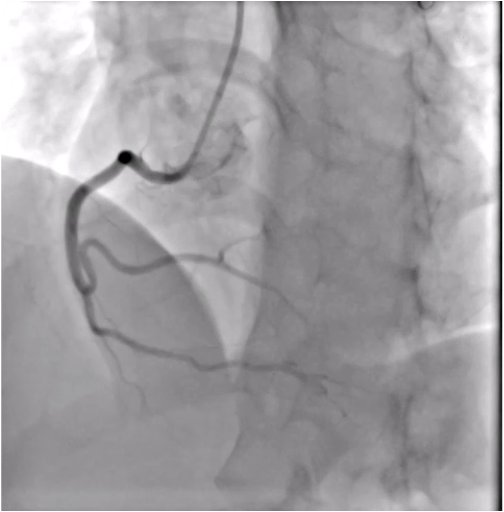
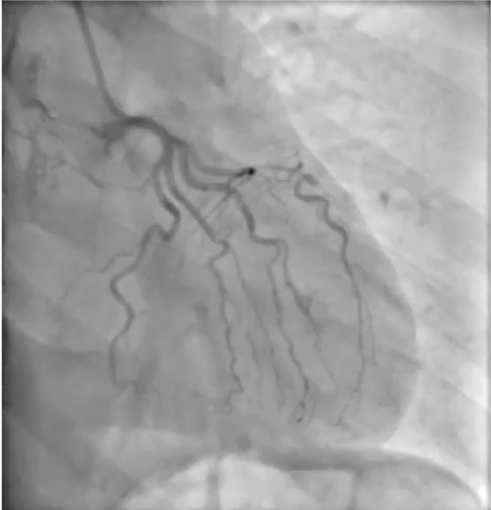
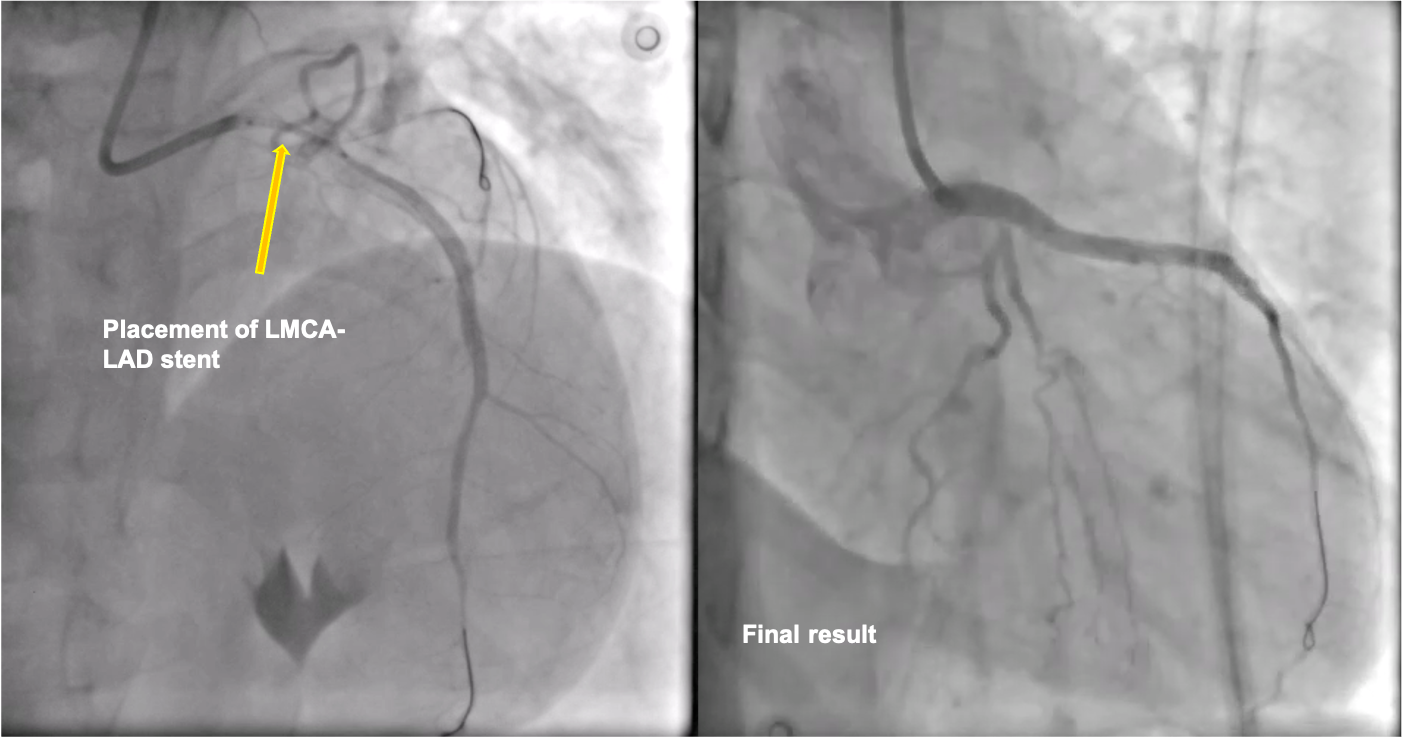
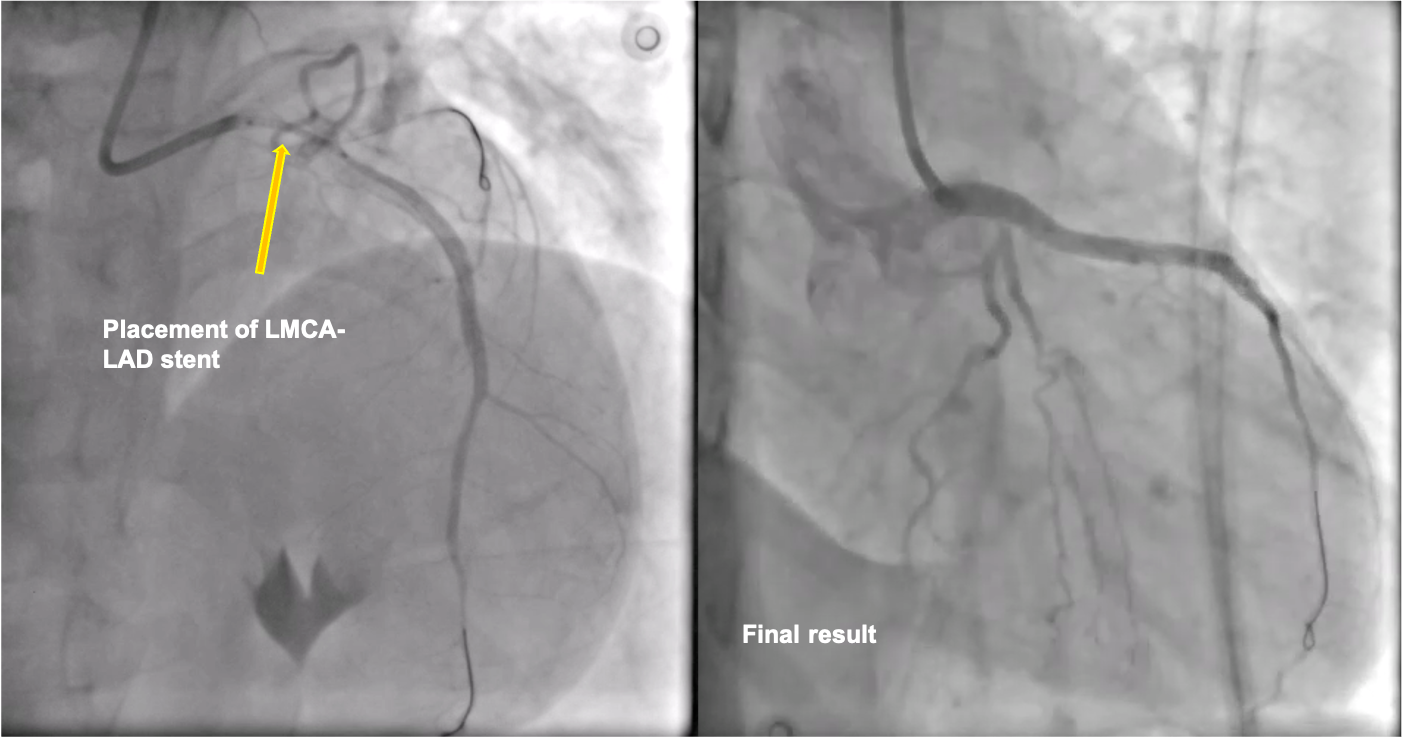
Patient was taken up for percutaneous coronary intervention (PCI). The left main coronary artery (LMCA) was engaged with an EBU 3.5. The lesion was easily crossed with Sion blue guidewire. Immediately following the wiring, there was a cessation of flow in the LAD from the ostia. A 2.5x12 mm balloon was then taken, and dottering was done in LAD along with pre-dilation at 12 atmospheric pressure. A drug-eluting stent (DES) of size 3.0x38 mm was deployed into LAD and stent was post dilated with a 3.5x12 mm non-compliant (NC) balloon. Everything appeared normal.However, upon closer examination, a degree of haziness was observed in LMCA. This prompted the question: was the haziness caused by dissection, thrombus, or another factor altogether? Optical coherence tomography (OCT) imaging was conducted to resolve this uncertainty, and the findings proved remarkable.A dissection flap was identified in the distal LMCA, which extended into the LAD. The guidewire initially entered the true lumen of the LMCA and then passed into the false lumen through this dissection. Subsequently, it traversed through the false lumen in the proximal LAD and returned to the true lumen of the mid-LAD. As a result, the stent was placed in the false lumen proximally and in the true lumen of the LAD distally.What should we consider doing next? The patient had no chest pain and was hemodynamically stable, and the artery had a TIMI 3 flow. One potential approach was to use intravascular ultrasound (IVUS) guidance to re-enter the true lumen and then place an additional stent to compress the previous stent, which would have resulted in excessive metal. Alternatively, we could put a single stent from the LMCA to the LAD, overlapping the previous stent, which could have compromised the diagonal branch.
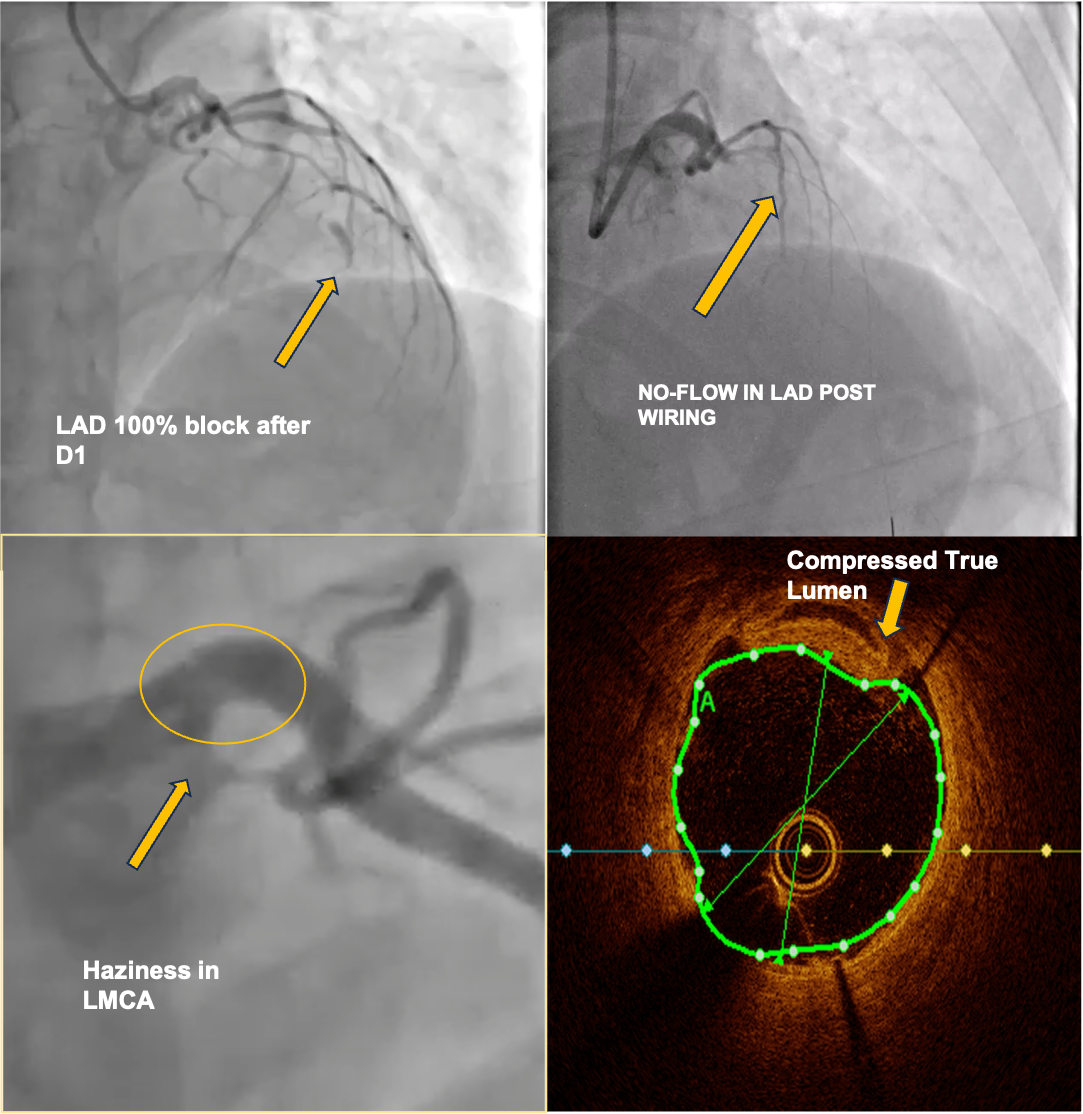
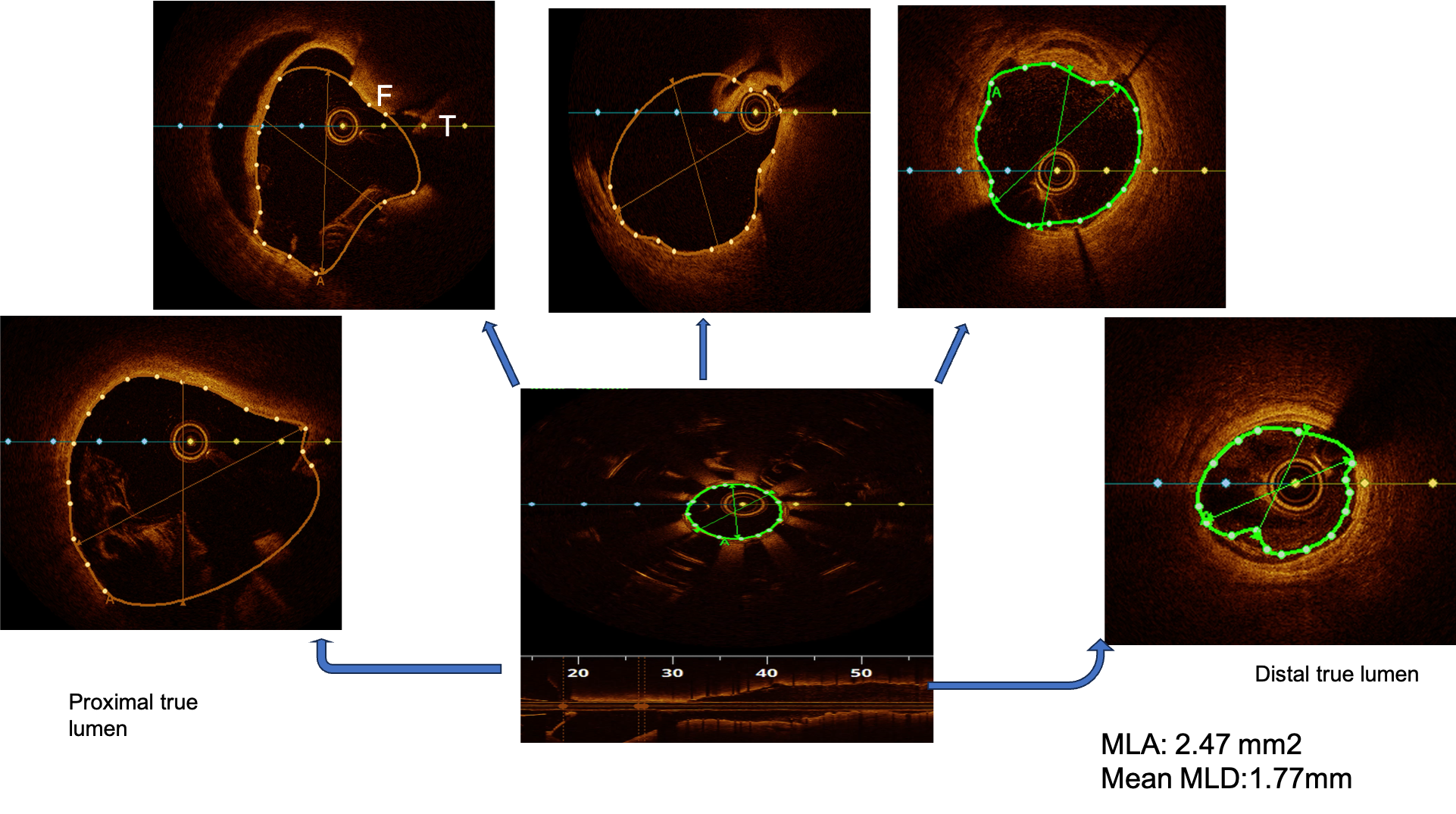
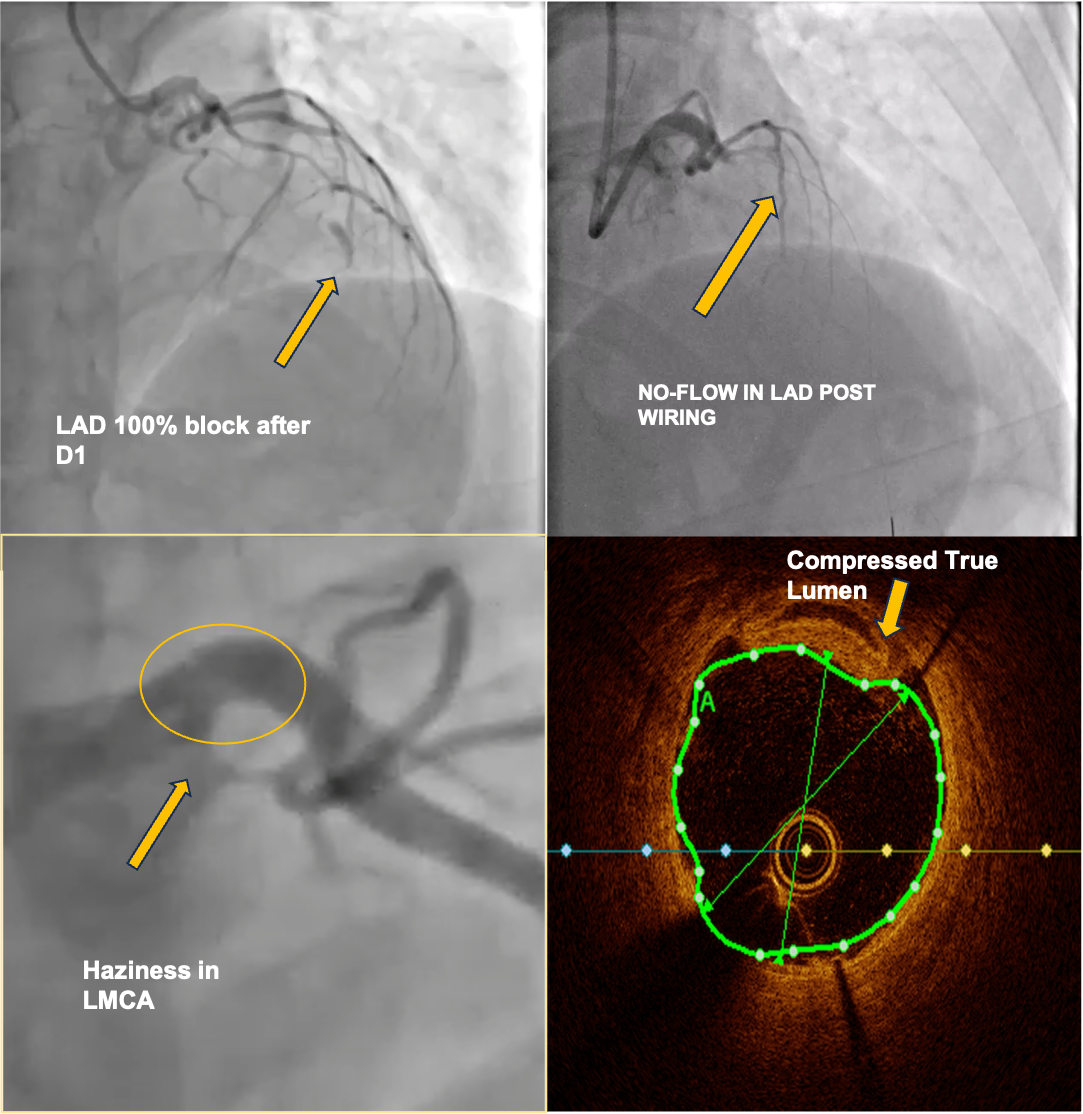
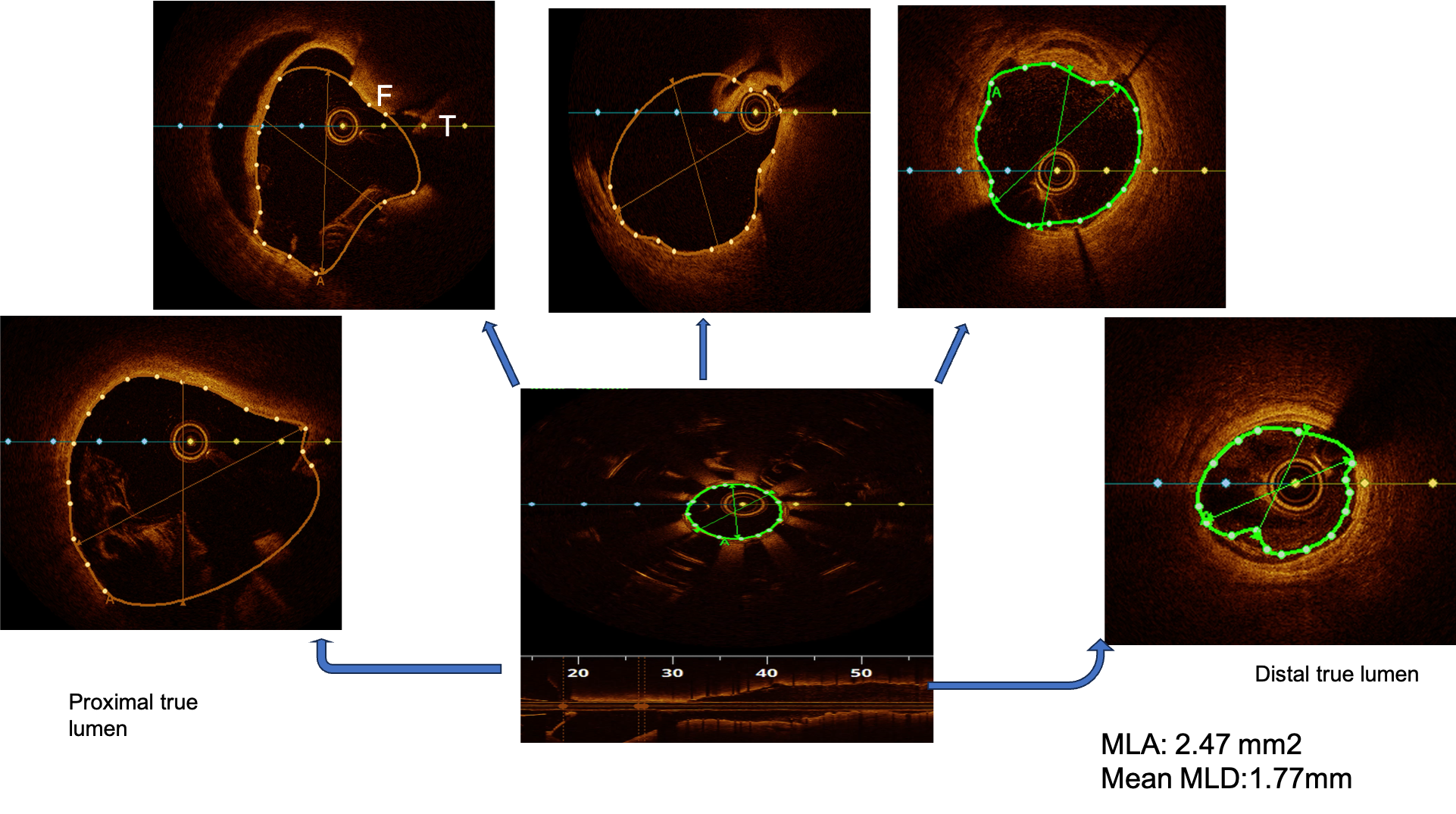
Case Summary
In this case, the aetiology was probably spontaneous coronary artery dissection (SCAD). The other possibility could be guide catheter-induced iatrogenic dissection. In STEMI, no reflow is expected due to thrombus; however, dissection was the cause of no-reflow here. Initially, since we had no difficulty crossing the guidewire, it was suspected to be a thrombus. However, the intracoronary imaging came to our rescue by delineating the exact cause. OCT was used instead of IVUS as it is better for understanding the morphology of dissection and thrombus, which were the likely culprits.


